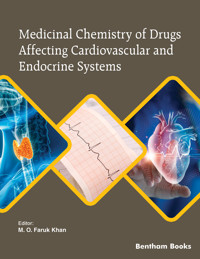
Medicinal Chemistry of Drugs Affecting Cardiovascular and Endocrine Systems E-Book
54,93 €
Mehr erfahren.
- Herausgeber: Bentham Science Publishers
- Kategorie: Fachliteratur
- Sprache: Englisch
The primary objective of this 4-volume book series is to educate PharmD students on the subject of medicinal chemistry. The book set serves as a reference guide to pharmacists on aspects of the chemical basis of drug action. Medicinal Chemistry of Drugs Affecting Cardiovascular and Endocrine Systems is the third volume of the series. This volume features 8 chapters focusing on a comprehensive account of drugs affecting both the cardiovascular system and the endocrine functions. The volume informs readers about the medicinal chemistry of relevant drugs, which includes the mechanism of drug action, detailed structure-activity relationships and metabolism. Topics covered include drugs that affect the renin-angiotensin system, calcium channel blockers, diuretics, hematological agents (anticoagulants, thrombolytic and antiplatelet agents), antidiabetics, antihistamines, proton pump inhibitors and therapeutic hormones. Each chapter also offers case studies and self-assessments to facilitate discussion and learning. The book equips students with a scientific foundation to competently evaluate, recommend and counsel patients and health care professionals regarding the safe, appropriate, and cost-effective use of medications. Students and teachers will also be able to integrate the knowledge presented in the book and apply medicinal chemistry concepts to understand the pharmacodynamics and pharmacokinetics of therapeutic agents in the body. The information offered by the book chapters will give readers a strong neuropharmacology knowledge base required for a practicing pharmacist.
Readership
PharmD / pharmacology students and teachers.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Veröffentlichungsjahr: 2024
Ähnliche
BENTHAM SCIENCE PUBLISHERS LTD.
End User License Agreement (for non-institutional, personal use)
This is an agreement between you and Bentham Science Publishers Ltd. Please read this License Agreement carefully before using the book/echapter/ejournal (“Work”). Your use of the Work constitutes your agreement to the terms and conditions set forth in this License Agreement. If you do not agree to these terms and conditions then you should not use the Work.
Bentham Science Publishers agrees to grant you a non-exclusive, non-transferable limited license to use the Work subject to and in accordance with the following terms and conditions. This License Agreement is for non-library, personal use only. For a library / institutional / multi user license in respect of the Work, please contact: [email protected].
Usage Rules:
All rights reserved: The Work is the subject of copyright and Bentham Science Publishers either owns the Work (and the copyright in it) or is licensed to distribute the Work. You shall not copy, reproduce, modify, remove, delete, augment, add to, publish, transmit, sell, resell, create derivative works from, or in any way exploit the Work or make the Work available for others to do any of the same, in any form or by any means, in whole or in part, in each case without the prior written permission of Bentham Science Publishers, unless stated otherwise in this License Agreement.You may download a copy of the Work on one occasion to one personal computer (including tablet, laptop, desktop, or other such devices). You may make one back-up copy of the Work to avoid losing it.The unauthorised use or distribution of copyrighted or other proprietary content is illegal and could subject you to liability for substantial money damages. You will be liable for any damage resulting from your misuse of the Work or any violation of this License Agreement, including any infringement by you of copyrights or proprietary rights.Disclaimer:
Bentham Science Publishers does not guarantee that the information in the Work is error-free, or warrant that it will meet your requirements or that access to the Work will be uninterrupted or error-free. The Work is provided "as is" without warranty of any kind, either express or implied or statutory, including, without limitation, implied warranties of merchantability and fitness for a particular purpose. The entire risk as to the results and performance of the Work is assumed by you. No responsibility is assumed by Bentham Science Publishers, its staff, editors and/or authors for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products instruction, advertisements or ideas contained in the Work.
Limitation of Liability:
In no event will Bentham Science Publishers, its staff, editors and/or authors, be liable for any damages, including, without limitation, special, incidental and/or consequential damages and/or damages for lost data and/or profits arising out of (whether directly or indirectly) the use or inability to use the Work. The entire liability of Bentham Science Publishers shall be limited to the amount actually paid by you for the Work.
General:
Any dispute or claim arising out of or in connection with this License Agreement or the Work (including non-contractual disputes or claims) will be governed by and construed in accordance with the laws of Singapore. Each party agrees that the courts of the state of Singapore shall have exclusive jurisdiction to settle any dispute or claim arising out of or in connection with this License Agreement or the Work (including non-contractual disputes or claims).Your rights under this License Agreement will automatically terminate without notice and without the need for a court order if at any point you breach any terms of this License Agreement. In no event will any delay or failure by Bentham Science Publishers in enforcing your compliance with this License Agreement constitute a waiver of any of its rights.You acknowledge that you have read this License Agreement, and agree to be bound by its terms and conditions. To the extent that any other terms and conditions presented on any website of Bentham Science Publishers conflict with, or are inconsistent with, the terms and conditions set out in this License Agreement, you acknowledge that the terms and conditions set out in this License Agreement shall prevail.Bentham Science Publishers Pte. Ltd. 80 Robinson Road #02-00 Singapore 068898 Singapore Email: [email protected]
FOREWORD
Gayle BrazeauFor a pharmacist, medicinal chemistry education is critical to developing an adequate knowledge base and critical thinking skills. In this eBook, the fundamental principles of medicinal chemistry including the functional groups occurring in medicinal agents, the acidity and basicity of drugs, and their water and lipid solubility as well as drug-receptor interactions are described. The physicochemical principles, isosterism, and spatial characteristics of drugs are prerequisites to understanding drug pharmacodynamics. Another important aspect that is crucial to comprehending the mechanism of drug action is the knowledge of important biosynthetic pathways that are frequently encountered in pharmaceutical interventions; a chapter has been devoted to this important aspect in this first volume. In this book, a comprehensive approach has been taken to explain the phases of drug metabolism, modifications of drug chemical structures, and their effects on drug pharmacokinetics, safety, and efficacy.
It is apparent that the authors have taken into consideration the integrated aspect of PharmD curricula while developing the contents. The standout feature of this eBook series is its layout, which includes 4 volumes in three distinct areas - the fundamental concepts, detailed structure-activity relationships of different drug classes, and recent developments in the area of medicinal chemistry and drug discovery. It offers students the opportunity to learn the principles of drug action in a stepwise manner. The case studies, student’s self-study guide, and self-assessment at the end of each chapter are unique features of this book that would be beneficial to both students and instructors. Although there are several medicinal chemistry textbooks available on the market, to my understanding this is the first textbook of its kind focusing on the integrated aspects of PharmD curricula.
As a pharmacy educator, leader, journal editor, and an expert in pharmacy curriculum, I am pleased to testify and endorse this eBook to pharmacy educators, and learners as one of the most useful resources in medicinal chemistry. Based on my pedagogical research and assessment of student learning, it is my understanding that this book takes a student-friendly approach that incorporates appropriat Reillustrative diagrams and study guides as well as self-assessments. In my early years as a student in the pharmacy, I found medicinal chemistry as a challenging subject area. The inclusion of clinical and management focuses in the modern PharmD curriculum left the students with limited time available to grasp all the basic concepts which made it more challenging for them to manage the old hard-core science-driven medicinal chemistry courses. This eBook series brings those memories of my early years as a pharmacy student and the evolution of pharmacy education, and gives me the confidence that it will pave the way for future medicinal chemistry education for pharmacists and other health professionals.
PREFACE
M. O. Faruk Khan, Ph.D.This is the third volume of the 4-volume eBook series, “Medicinal Chemistry for Pharmacy Students”. The primary objective of this e-Book series is to educate PharmD students in the area of medicinal chemistry and serve as a reference guide to pharmacists on aspects of the chemical basis of drug action. A thorough discussion of key physicochemical parameters of therapeutic agents and how they affect the biochemical, pharmacological, pharmacokinetic processes and clinical use of these agents is the primary focus of the whole book. The rationale for putting together an e-Book of this nature is to equip PharmD students with the scientific basis to competently evaluate, recommend and counsel patients and healthcare professionals regarding the safe, appropriate, and cost-effective use of medications.
This third volume of the series is comprised of 8 chapters focusing on a comprehensive account of medicinal chemistry of drugs affecting the cardiovascular and endocrine systems. It provides the mechanism of drug action, detailed structure-activity relationships and metabolism as well as the clinical significance of drugs affecting the cardiovascular and endocrine system to give the knowledge base for pharmacists.
Chapter 1 provides a comprehensive account of the medicinal chemistry of drugs affecting the renin-angiotensin system (RAS). This chapter includes pathophysiologic principles, mechanism of action, structure-activity relationships (SAR) and metabolism of drugs affecting RAS including enzymes and hormones and their roles in blood pressure, structures, binding, and chemistry and SAR of the antagonists involved in RAS such as the angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs) and renin inhibitors. It also discusses the clinical significance and therapeutic evaluations of these classes of drugs by solving case studies as well as the discovery process of ACEIs and ARBs.
Chapter 2 is a comprehensive account of the medicinal chemistry of antihypertensive drugs, Ca2+-channel blockers (CCBs). It details the pathophysiologic principles, mechanism of drug action, SAR, classifications, and their clinical significance.
Chapter 3 focuses on the medicinal chemistry of the diuretic agents. It provides a detailed account of the pathophysiologic principles of diuretics, the mechanism of drug action and the SAR of these drugs. The chemical principles and classification of diuretics, their metabolism and pharmacokinetic parameters, and the clinical significance as well as safety parameters of these drugs have been clearly delineated.
Chapter 4 is a comprehensive account of the medicinal chemistry of the anticoagulants, antiplatelets and thrombolytic agents and their relatives – their pathophysiologic principles, mechanism of action, SAR and metabolism. Topics include the physiology and pathophysiology of clotting, major classes of anticoagulant drugs and their structures and binding, distinctions among drugs used as antiplatelets, anticoagulants, and fibrinolytic agents and delineation of the clinical significance, therapeutic evaluations and discovery story of these classes of drugs.
Chapter 5 is a comprehensive account of the medicinal chemistry of antihistamines, H2 receptor (H2R) blockers, H3 receptor (H3R) blockers, and proton pump inhibitors (PPIs). It provides the pathophysiologic principles, mechanism of drug action, and detailed SAR of the drugs in these classes Topics include a concise account of the physiochemical properties of histamine and histamine receptors, chemical classes of antihistamines, H2R and H3R antagonists, the distinction between sedating and non-sedating antihistamines, as well as the first generation, second generation, and third generation antihistamines. It also discusses the structural features of cromolyn and related mast cell stabilizers as well as the proton pump inhibitors including their development, mechanism of action, and structural and physicochemical features.
Chapter 6 is a comprehensive account of diabetes and the medicinal chemistry of antidiabetic drugs. It discusses the physicochemical principles, mechanism of action, SAR, and metabolism of the antidiabetic drugs. The clinical features of diabetes and differentiation between type I and type II diabetes, various risk factors and corresponding mechanisms responsible for the development of diabetes and pathophysiologic mechanisms responsible for the clinical features of diabetes have also been discussed. A review of biosynthesis of insulin, its metabolic outcomes, regulation of insulin secretion, and insulin signaling have been explained. This chapter has classified all the injectable and oral antidiabetic drugs and provided their clinical significance as well.
Chapter 7 is a comprehensive account of the medicinal chemistry of hormonal therapy. It provides the physicochemical principles, mechanism of drug action, SAR, and drug metabolism of the hormonal agents. This chapter discusses in detail hormone replacement therapy (HRT), androgen replacement therapy (ART), oral contraceptive pills and gender-affirming hormone therapy. It also provides a detailed understanding of thyroid hormones and their clinical significance.
Chapter 8 provides a comprehensive account of the medicinal chemistry of drugs arising from structural modifications of prostanoids, which are naturally occurring eicosanoids. These drugs are used for a variety of disease states including but not limited to glaucoma, pulmonary arterial hypertension, and peptic ulcers. This chapter provides the pathophysiologic principles, mechanism of drug action, and SAR of these agents with their clinical significance.
The chapters in this volume are designed to guide the reader to review, integrate, and apply principles of medicinal chemistry to drug action of therapeutic agents. All concepts are illustrated with diagrams or figures, with the keywords highlighted, bulleted or numbered. Wherever needed, special boxes and case studies are included. In addition, each chapter is reinforced with student’s self-study guides and self-assessment questions. Special notations are highlighted using call-out boxes for visual effect. Tables and figures are used to augment the text as needed.
We would like to express our sincere gratitude to the contributing authors for their time and effort in completing this volume. We would also like to thank Bentham Science Publishers, particularly Ms. Asma Ahmed (Manager Publications) and Mr. Mahmood Alam (Director Publications) for their support. We are confident that this volume of the eBook series will guide students and educators of pharmacy and related health professions worldwide.
List of Contributors
Drugs Affecting Renin-Angiotensin System
M. O. Faruk Khan1,*,Karrie Murphy1Abstract
This chapter presents a comprehensive account of the medicinal chemistry of drugs affecting the renin-angiotensin system (RAS). It provides the mechanism of drug action and details structure-activity relationships (SAR) of the drugs affecting RAS to give the knowledge base for pharmacists. After studying this chapter, students will be able to:
• Describe the historical background the RAS and drugs acting on this system.
• Explain RAS enzymes and hormones and their roles in blood pressure.
• Classify drugs acting on the RAS and their structures and binding.
• Discuss in detail the chemistry and SAR of the antagonists involved in RAS including angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs) and renin inhibitors.
• Delineate the clinical significance and therapeutic evaluations of these classes of drugs by solving case studies.
• Explain the discovery process of ACEIs and ARBs.
HISTORICAL BACKGROUND
As early as 1898, renin’s role in increasing blood pressure was suggested based on the observation that the injection of kidney extracts dramatically increased rabbit’s blood pressure [1]. In the 1930s, a pathologist named Harry Goldblatt discovered a vasoconstricting agent (which later appeared to be renin) secreted by the kidneys responsible for increasing blood pressure [2]. In 1939, it was concluded that renin is an enzyme which catalyzes the formation of angiotensin (Ang) [3]. Decades later, two forms of Ang, Ang I and Ang II, were identified.
A zinc metallopeptidase, angiotensin converting enzyme (ACE), was discovered in 1954 from equine plasma and purified in 1956 [4, 5]. It is now known that renin first converts angiotensinogen (a 14-amino acid peptide) into Ang I (a decapeptide), which is then converted by ACE into Angiotensin II (Ang II, an octapeptide; Asp-Arg-Val-Tyr-Ile-His-Pro-Phe) that causes vasoconstriction and hypertension [6].
In 1965, a Brazilian scientist, Sérgio Henrique Ferreira, reported the presence of a bradykinin potentiating factor (BPF) in the venom of a South American pit viper Bothrops jararaca [7], then he moved to the laboratory of Sir John Vane in London, UK for further research. Ng and Vane in 1967 showed that Ang I is quickly converted into Ang II by ACE in the pulmonary circulation and lung. The finding that BPF inhibits the conversion of Ang I into Ang II led to believe that bradykinin also disappears in the lung by the action of ACE [8-10].
Vane convinced Bristol Myers Squibb Pharmaceutical Company to work on the project of snake venom and started fractional analysis of the BPF. They isolated a nonapeptide, teprotide (SQ 20,881), to be the most potent ACE inhibitor (ACEI) and antihypertensive agent in vivo (see later in drug discovery case studies) [11]. They purified a few more peptides: all of which were found to be ACEIs Table (1) [12]. As a peptide, teprotide is orally ineffective. In search of an orally effective drug, they investigated about 2000 non-peptides without any success. In the early 1970s, they started using the other mechanistically similar, but widely studied enzyme carboxypeptidase A and its 3D-structure of the active site to design ACEI and successfully launched captopril as the first orally active ACEI in 1975, which was approved by US Food and Drug Administration (FDA) in 1981 (see later in drug discovery case studies) [13].
The first Ang II receptor type 1 (AT1R) was identified during the 1970s and was cloned in the 1990s. The AT2R was identified during the early 1980s and cloned in the early 1990s [14] although the existence of different forms of ATRs was suggested in 1974 [15] by Papadimitriou and Worcel. Other ATRs including AT3R and AT4R have also been recognized to date, all of which are G-protein coupled 7-transmembrane (7-TM) containing receptors. Only AT1R and AT2R are clinically significant [16]. AT1R mediates most of the functions of Ang II while AT2R contributes to the regulation of blood pressure and renal functions. This discovery triggered the development of AT1R blockers (ARBs). Saralasin, a peptide analog of Ang II, was found to be a potent ARB but lacked oral bioavailability [17]. Takeda, a Japanese company, in the early 1980s, tested a series of compounds to find a lead and developed losartan as the first clinically useful, orally active, potent and selective nonpeptide ARB by DuPont chemists [18].
Another drug acting on the renin-angiotensin system (RAS) is aliskiren, an orally effective, nonpeptide, low-molecular-weight renin inhibitor. It was co-developed by the Swiss pharmaceutical companies Novartis and Speedel through a combination of molecular modeling techniques and crystal structure elucidation of renin and the renin-drug complex [19, 20]. Aliskiren was approved for clinical use in the USA in 2007 for the treatment of primary hypertension.
Angiotensin inhibition has also been combined with neprilysin inhibition for the treatment of chronic heart failure. This angiotensin receptor neprilysin inhibitor (ARNI) is a combination of valsartan (an ARB) and sacubitril, a neprilysin inhibitor approved in July 2015 by the FDA [21, 22]. The development of this drug was prompted by the need to inhibit neprilysin and RAS concurrently. Neprilysin inhibition alone can enhance the beneficial response of natriuretic peptides released in heart failure but can result in in the counteractive activation of the RAS by increasing angiotensin II. Although both ACEIs and ARBs inhibit RAS, only ARBs are recommended to be utilized with neprilysin inhibitors. Prior to valsartan/sacubitril approval, a drug containing an ACEI and a neprilysin inhibitor called omapatrilat was developed. This drug was never marketed due to the increased incidences of angioedema observed in clinical trials [23].
Today, drugs affecting the RAS comprise a large class of clinical agents and many of these frequently are among the top 200 medications dispensed. Those included in the last few years are shown in Fig. (1).
INTRODUCTORY CONCEPTS
The Renin-Angiotensin System (RAS)
The RAS regulates blood pressure and fluid balance. Renin, secreted by kidneys when blood volume or blood pressure is low, stimulates the biosynthesis of Ang I from angiotensinogen. ACE in the lung and pulmonary circulations then converts Ang I to Ang II, which causes vasoconstriction resulting in increased blood pressure. Ang II also stimulates the secretion of aldosterone which causes increased sodium reabsorption in exchange for potassium and thus increased blood volume resulting in high blood pressure. The major blood pressure-elevating effects of the most prominent bioactive component of the RAS, Ang II, is summarized below and in Fig. (2) [24].
Fig. (1)) Structures of renin-angiotensin system inhibitors frequently included in the top 200 drugs list. Fig. (2)) Renin-angiotensin system (RAS) and its role in increasing blood pressure. Vasoconstriction of arterioles.Increased sodium and fluid reabsorption from tubules.Increased aldosterone release from the adrenal cortex.Increased vasopressin (antidiuretic hormone; ADH) release.Inhibition of RAS determines an antihypertensive effect. Examples of clinically used antihypertensive agents include ACEIs (e.g., captopril), ARBs (e.g., losartan) and the renin inhibitor aliskiren. The inhibition of ACE reduces the formation of Ang II while the ARBs directly inhibit the action of Ang II by blocking the AT1Rs at different sites. The renin inhibitor blocks the production of both Ang I and Ang II.
Angiotensin-Converting Enzyme Inhibitors (ACEIs)
The potent vasoconstrictor Ang II, which affects peripheral resistance, renal function and cardiovascular structure, is biosynthesized from Ang I by the action of ACE. Between these two isoforms of ACE, the somatic isoform and the testicular isoform, the C-domain of the somatic isoform is predominantly involved in blood pressure regulation. There is also another active domain of the somatic isoform called the N-domain involved in hematopoietic stem cell differentiation and proliferation. Overall, the somatic isoform of ACE is involved with the production of high blood pressure, inhibition of which is antihypertensive (Fig. 3). The ACEIs effectively block the conversion of Ang I to Ang II. ACE inhibitors have much greater affinity for and inhibitory activity against the C-domain of somatic ACE. A number of ACEIs are now in clinical practice; all of which have similar therapeutic and pharmacologic effects differing primarily in their potency and pharmacokinetic profiles.
Fig. (3)) Site of action of angiotensin converting enzyme inhibitors (ACEIs).Structure of ACE Active Site and Mechanism of Ang I Hydrolysis
To date, the X-ray crystal structure of ACE found in adult human testes (tACE) and its complex with lisinopril have been resolved [25]. It is a 701-residue-long enzyme and is identical to the somatic ACE (sACE) in C-terminal, except for the first 36 residues [26]. The tACE is mainly a helical structure comprising 27 helices and only 6 short β-strands that pack together to form an ellipsoid structure with a 30Å deep central cavity, which is surrounded by four α helices (α13, α14, α15 and α17) and one β strand (β4). The cavity is covered by three highly charged N-terminal helices that keep large, folded peptides away from entering into and processed by ACE. The active site contains a characteristic HExxH sequence (His383-Glu-Met-Gly-His387), located on the helix α13, as the Zn2+-binding motif like other metallopeptidases. This site, together with Glu411 of helix α14, binds the metal ion (Fig. 4) [25].
Fig. (4)) Binding of Ang I C-terminal tripeptide to the active site of ACE showing the mechanism of cleavage of the scissile bond.The hydrolysis of Ang I is mediated by the attack of the water molecule (that becomes electron rich getting from glutamate anion) on the carbonyl carbon of the scissile bond (the peptide bond between -Phe-Glu- that is to be cleaved by the action of ACE is called scissile bond). Glu384 activates water as the nucleophile (base). Zinc (Zn2+) bound by the HExxH (His-Glu-xx-His) motif serves to polarize the carbonyl group, increasing the electrophilicity of the carbonyl carbon and set it in the correct position for attack by water Fig. (4). While the carbonyl oxygen of Ala354 stabilizes the scissile bond N atom through hydrogen bonding, Lys511, Tyr520 and possibly Gln281 stabilize the terminal carboxylate; and Tyr523 promotes the formation of the intermediate. Cleavage of the C-N bond with subsequent abstraction of proton (H+) on the amine nitrogen and hydroxyl on the carbonyl carbon is coordinated by Glu281.
The hydrolysis is highly chloride (Cl-) dependent, and this dependency is increased with the increase of pH. Two Cl- ions, the first one being 20.7 Å and the second 10.4 Å away from the Zn2+, are involved in this activation by an indirect mechanism that may include restraining some residues (possibly Arg522) from interfering with the active site or keeping the active site in a favorable conformation. The first Cl- ion is bound to the active site residues Arg489, Arg186 and Trp485 while the second Cl- ion is bound to Arg522 and Tyr224 [25, 27].
Inhibition of ACE – The ACEI-ACE Interaction
The ACEI-ACE interaction is illustrated by those of lisinopril and captopril in Fig. (5). It is clearly evident that the inhibitors bind at the same active site as Ang I (Fig. 4) in a similar fashion. The carboxyl group of lisinopril and thiol group of captopril bind the active site Zn2+. The carboxylate on the proline molecule of both drugs causes similar type of hydrogen bonding and charged interactions with Tyr520 and Lys511. His513 and His353 are involved in hydrogen bonding interaction with the peptide carbonyl oxygen on the proline. Lisinopril, being a larger molecule occupies other sites causing more hydrophobic, charged and hydrogen bonding interactions with Glu384, Glu162, and Tyr523, which are absent for captopril (Fig. 5A). This interaction competitively inhibits the ACE’s peptide bond hydrolyzing activity [25, 27, 28]. The ACEI-ACE interactions are shown in Fig. (5B) using captopril as a model ACEI.
Fig. (5)) Binding of (A) lisinopril and (B) captopril to the active site of ACE.Pharmacophore and SAR Summary of ACEIs
The general structure of the ACEIs is illustrated in Fig. (6). All the ACEIs are acidic with pKa ranging from 0.2 for captopril to 6.1 for fosinopril. Overall, the acidity is in the order: captopril > lisinopril > enalapril > perindopril > ramipril > trandolapril > moexipril > quinapril > benazepril > fosinopril.
Fig. (6)) General Pharmacophoric group of ACEIs.SAR Summary
The important structural requirements and SAR of the ACEIs can be summarized as follows:
SAR 1: Since Zn2+ is a critical site for the action of the ACE, a perfectly oriented Zn2+-ligand is the primary requirement for any ACEI. A thiol, carboxylate or phosphinate is usually used as a Zn2+-ligand. Based on the nature of Zn2+-ligand, there are three types of ACEIs: 1) Sulfhydryl-containing inhibitors (e.g., captopril); 2) Dicarboxylate-containing inhibitors (e.g., enalapril); 3) Phosphinate- containing inhibitors (e.g., fosinopril).
SAR 2: The carboxylate function on the heterocyclic site, common to all ACEIs, causes hydrogen bonding as well as ionic interactions with the receptor. Large hydrophobic heterocyclic rings attached to this carboxylate function increase potency and bioavailability. The aromatic ring system is less tolerated by ACE active site than a purely alicyclic ring system.
SAR 3: The alkyl chain R may be a methyl (e.g., in captopril), which mimics the side chain of alanine and should also have a similar stereochemical arrangement as L-alanine. Lisinopril contains n-butylamine (lysine side chain) which increases the binding by involving a charged interaction at a nearby glutamate in the ACE active site Fig. (5).
SAR 4: In case of inhibitors with carboxylate or phosphinate, a phenethyl or phenpropyl side chain (Ar) at a close proximity of the Zn2+-ligand that mimics the phenylalanine of Ang I improve the binding and inhibitory potency by causing hydrophobic interaction with tyrosine in the enzyme active site. On the contrary to SAR 2, an aromatic ring is favored over an aliphatic system.
The Individual ACEIs and their Structural and Therapeutic Evaluations
Sulfhydryl-Containing Inhibitor – Captopril
Captopril is the first nonpeptide compound prepared to be marketed as an anti-hypertensive drug and is a thiol-containing ACEI. It acts by binding to ACE and inhibiting the formation of Ang II from Ang I. The reduced level of Ang II and the resulting loss of feedback inhibition of renin release leading to an increase in plasma renin activity may develop resistance to the drug over long-term use. The interaction of captopril and ACE is shown in Fig. (5B) above. Captopril binds with ACE with approximately 30,000 times greater affinity than Ang I. It has only one chiral center and the S isomer is more potent.
Captopril is a small, orally active compound, easily absorbed into the bloodstream. Among all the ACEIs currently on the market, it is the least potent and requires more frequent administration (at least twice daily or three times daily while others are administered once or twice daily) to control hypertension. It also causes cough due to increased production of bradykinin, which is common to all ACEIs. The other principal side effects, e.g., rashes, and loss of taste, are reversible on cessation or a reduction of dose and are assumed to be due to the presence of the thiol function.
Captopril exhibits approximately 30-40% oral bioavailability although about 60-75% is absorbed. The bioavailability decreases in the presence of food although some evidence supports that this may be clinically insignificant. The thiol undergoes easy oxidation to disulfides (Fig. 7), which leads to a short duration of action, in addition to decreased bioavailability of captopril that explains its twice daily (BID) or three times daily (TID) administration. About 40-50% of its dose is excreted unchanged [29, 30].
Fig. (7)) Thiol oxidation of captopril to inactive disulfides.Dicarboxylate Containing Inhibitors
Enalapril
Enalapril is also a prodrug useful for the treatment of hypertension. Merck & Co. developed this as the first nonthiol ACEI to overcome the drawbacks like taste disturbances and other thiol-related side effects of captopril. It contains a phenethyl side chain on the Zn2+-site that accounts for about ten times more potency than captopril in controlling hypertension (SAR 4). Its active form is the metabolite dicarboxylate enalaprilat (Fig. 8).
Fig. (8)) Metabolic activation of enalapril.While enalaprilat is only suitable for intravenous administration, enalapril is active orally giving a peak plasma enalaprilat concentration within 2 to 4 hours. Enalapril is about 60% orally bioavailable and acts for about 24 h. Enalaprilat, which is excreted unchanged via urine, is only active for 6 h. In addition to dry cough, it may also cause hypotension and dizziness [30, 31].
Lisinopril
Lisinopril is the lysine-analog of enalaprilat and is unique in that it is hydrophilic yet orally active. The lysine residue may permit peptide-carrier-mediated transport of the drug from the gut to the portal circulation thus allowing it to be orally effective. It binds the ACE very strongly as conforms with SARs 2, 3 & 4 (Fig. 5A) but due to its low bioavailability of about only 25%, the dosage requirement is similar to that of enalapril.
It is absorbed very slowly allowing peak serum concentrations in about 7 hours of oral administration to adult patients. It has a long half-life; it is not metabolized by the liver and is excreted unchanged in the urine. Some of its serious side effects include oliguria, angioedema, anaphylaxis, itching, stomach pain, jaundice, chest pain dry cough, joint pain, and blurred vision [30, 32].
Benazepril (LotensinTM)
Benazepril is a prodrug used alone or in combination with hydrochlorothiazide or amlodipine to treat hypertension, congestive heart failure, and chronic renal failure. It has a fused aromatic ring on the heterocyclic terminal and a phenethyl ring system on the Zn2+-site; and is slightly less potent than enalapril (SAR 2 and 4). It is about five times more potent than captopril in controlling hypertension. Long-term therapy is beneficial to kidneys. The ester prodrug needs cleavage to the active carboxylate form, benazeprilat. In addition to cough, it may also cause headache, angioedema and anaphylaxis and should be avoided during pregnancy.
The terminal carboxylic acid extended from the ring by one more carbon atom is susceptible to ester glucuronidation. It is highly protein bound (>95%), has low oral bioavailability (~37%), and has a long duration of action of about 24 h [27, 30].
Moexipril
Moexipril is slightly more potent than benazepril but less potent than enalapril possibly due to an unfavorable aromatic ring on the heterocyclic site (SAR 2) and/or its low oral bioavailability (~13%). It also has another fused aromatic ring on the heterocyclic site. It is an ester prodrug and is hydrolyzed to the active carboxylate moexiprilat.
It is mainly excreted in the feces and the rest through urine unchanged or as a cyclized metabolite Fig. (9). It should not be used by pregnant or breast-feeding mothers. It has similar pharmacological and toxicological profiles to benazepril [30].
Fig. (9)) Cyclization of moexipril and moexiprilat. Similar cyclization is observed with ramipril and perindopril.Perindopril
Perindopril is a nonaromatic ring containing dicarboxylate ACEI, which is a prodrug activated to carboxylate perindoprilat. It has a larger aliphatic ring system on the heterocyclic site and a three-carbon chain on the Zn2+-site. It is commonly used as a tert-butylamine salt. Recently, arginine salt has been shown to be equipotent and pharmaceutically more stable. It has potency and toxicological profiles comparable to enalapril.
It has high oral bioavailability (65-95%) and a long duration of action of about 24 h. It is extensively metabolized by hydrolysis and glucuronidation as well as cyclization similar to moexipril and eliminated mostly via urine [30, 33-35].
Quinapril
Quinapril contains the favorable aromatic group on Zn2+-site (SAR 4) but also unfavorable aromatic ring on the aliphatic site (SAR 2). It is structurally similar to enalapril except for the pyrrole ring which is replaced with a tetrahydroisoquinoline ring system giving half the potency of enalapril. Other pharmacological and toxicological profiles are similar to enalapril. It exhibits moderate oral bioavailability (~60%); is highly protein bound (~97%) and undergoes renal elimination [30, 36].
Ramipril
Ramipril is structurally similar to enalapril, but it has a fused cyclopentane ring with the pyrrole-2-carboxylate ring which may account for its 2-times more potency (SAR 2). Broadly it exhibits similar pharmacological and toxicological profiles to enalapril except for the difference in potency, thus it needs lower therapeutic dosages. It has an oral bioavailability of 50-60%, undergoes extensive metabolic transformation including hydrolysis, glucuronidation and cyclization like moexipril and is eliminated via fecal and renal routes [30, 37, 38].
Trandolapril
Trandolapril is the most potent among all the currently available ACEIs (SAR 2 & 4); however, it is only slightly more potent than ramipril. It is structurally similar to ramipril, but it has a cyclohexyl ring fused with the pyrrole-2- carboxylate ring and exhibits similar pharmacological and toxicological profiles. Its oral bioavailability is about 70% and eliminated mainly through faces and some via renal excretion as trandolaprilat or glucuronide and cyclized metabolites. About 80% is bound to proteins [30].
Phosphinate Containing Inhibitor - Fosinopril
Fosinopril (MonoprilTM)
Fosinopril is the only phosphinate-containing ACEI marketed. It is a prodrug and is activated by hydrolysis to fosinoprilat Fig. (10). It is eliminated by both liver and kidneys and is thus useful in patients with renal impairments. Its phosphinate is attached to a butyl phenyl group (SAR 4) and the pyrrole ring is attached to a cyclohexyl ring (SAR 2) to increase lipophilicity and potency.
Fig. (10)) Activation and metabolism of fosinopril.Fosinopril is absorbed slowly when given orally, only 36% bioavailable, and is highly protein bound (95%). Both fosinopril and fosinoprilat are p-hydroxylated at the aromatic ring. The p-hydroxy fosinoprilat is equipotent and is completely deactivated by glucuronidation at the p-hydroxy group (Fig. 10) [30, 39].
ANGIOTENSIN II RECEPTOR BLOCKERS (ARBs)
Most functions of Ang II including vasoconstriction, aldosterone release, and sodium reabsorption, and thus all hemodynamic effects of ARBs, are mediated through the AT1Rs. AT1Rs are abundant in vascular smooth muscles including kidneys, liver, adrenal gland, brain, and heart [15].
The AT1R Binding Pockets
Ang II bends in the Tyr-Ile-His region to form a hairpin shape which is stabilized by charged interaction between the amino and carboxyl terminals. The aromatic ring of the C-terminal Phe residue is crucial for its binding and activity. Aromatic groups of Tyr, His and Arg as well as the charged carboxyl terminal are essential for binding and agonist activity of Ang II. Lys102 (TM III) and Lys199 (TM V) are believed to be important charged residues involved in binding the carboxylate function of Phe at the C-terminal of Ang II. This interaction is stabilized by the Trp253 (TM VI) of AT1R. Residues Phe259 and Asp263 (TM VI), Ser105 (TM III) and Arg167 (TM IV) are also involved in this binding. The Asp281 (or Asp278) (TM III) causes ionic interaction with the guanidium cation of Arg in Ang II (Fig. 11) [15, 30, 41].
Fig. (11)) Schematic representation of binding of Ang II with AT1R.Pharmacophore of ARBs and Structure-Activity Relationship
Broadly, there are two types of ARBs based on their mechanism of action:
Insurmountable antagonists: candesartan, carboxylate metabolite of losartan, valsartan and irbesartan. These noncompetitive antagonists inhibit the receptor by stabilizing their inactive state (inverse agonists) and are bound tightly exhibiting a longer duration of action.Surmountable antagonists: losartan, eprosartan, and telmisartan. These are competitive antagonists which occupy the same active site as Ang II.The important residues required for binding losartan at the active site have been identified to be Val108 (TM III), Ala163 (TM IV), Pro192 and Thr198 (TM V), Ser252 (TM VI) and Leu300, Phe301 and Asn295 (TMVII). The imidazole ring binds to Asn295 (TM VII) and the biphenyl group binds to Phe301, Phe300, Trp253 and His256 (TM VI & VII). The tetrazole group mimics the carboxylate of Ang II and interacts with Arg167 and Lys199 (TM IV & V). Similar binding is observed with other surmountable antagonists (Fig. 12) [15, 18, 40].
Fig. (12)) Schematic representation of binding of losartan with AT1R.Each ARB, especially the inverse agonist type, differs in interacting with the receptor. It has been suggested based on valsartan binding and mutations of important amino acid residues that Ser105, Ser109 and Lys199 are the most critical for the inverse agonists’ binding and activity [42]. There are great structural similarities among ARBs (Fig. 13) and their SAR pattern can be summarized as follows [15, 18, 40, 43].
Fig. (13)) Structures of ARBs.SAR Summary
SAR 1: A lipophilic alkyl substituent (2-butyl, -propyl or -ethyl) together with the biphenyl-methyl group is needed for interaction with hydrophobic pockets of the receptor. The biphenyl-methyl group can be replaced by an equivalent, e.g., carboxy benzyl group that mimics more closely the phenolic moiety of Tyr of Ang II (e.g., in eprosartan).
SAR 2: An acidic tetrazole or CO2H at the 2-position of the biphenyl-methyl group is required to bind with a basic group in the receptor. Tetrazole derivatives are more potent in controlling blood pressure than carboxyl analogs, possibly due to more lipophilicity and thus bioavailability.
SAR 3: An imidazole or equivalent system e.g., N-acyl valine or aromatic ring-fused imidazole, is important for proper binding. The chlorine atom in the 4-position of the imidazole ring in losartan is probably not of much importance in receptor binding. The hydroxymethyl group, a medium-sized hydroxyalkyl group and a charged carboxylate group at 4- or 5-position of the imidazole ring, are favorable for receptor binding through hydrogen bonds. A bulky alkyl or alkenyl group is unfavorable at this place.
Candesartan and olmesartan have the highest affinity for the AT1Rs, followed by irbesartan and eprosartan. Valsartan and telmisartan have about ten-fold less affinity than that of candesartan; losartan has the least affinity. All ARBs show about 10,000 times less affinity for the AT2R [15, 18, 40, 43].
The Individual ARBs and their Structural and Therapeutic Evaluations
In general, all ARBs have a large therapeutic index and low oral bioavailability and are highly plasma protein bound. Oral administration once a day provides sufficient antihypertensive effects by the ARBs [40]. The individual agents are discussed below.
Losartan is the first member of this class of antihypertensive agents, which is a potent AT1 antagonist in its own right. About 14% of the dose is metabolized to the carboxylic acid form (Fig. 14), which has a 10-fold higher affinity for the AT1R and controls the blood pressure for 24 h.
Fig. (14)) Active metabolite of losartan.Losartan is well absorbed orally and undergoes substantial first-pass metabolism with a systemic bioavailability of ~33%. Both losartan and its active metabolite are highly bound to plasma proteins (~99%). Losartan does not cross the blood-brain barrier. It is primarily metabolized by CYP2C9 and CYP3A4 forming the active carboxylate as the major metabolite, in addition to several inactive metabolites. It is eliminated both in urine and faces and is not accumulated after repeated doses [15, 30].
Candesartan is patterned after losartan with a phenyl ring fused to the imidazole ring. It is administered in its cilexetil prodrug form. Hydrolysis of the first hydrolyzable group in cilexitil results in spontaneous decomposition to the active metabolite having a carboxylate functional group in the gastrointestinal tract.
Candesartan is absorbed orally with a systemic bioavailability of ~15% and is highly protein bound (~99%). About 26% of the oral dose of candesartan is excreted unchanged in urine and the rest is excreted in feces (via bile). About 25% of candesartan undergoes hepatic O-deethylation to an inactive metabolite (Fig. 15) [15, 30].
Fig. (15)) Bioactivation and inactivation of candesartan.In valsartan, imidazole is replaced by an N-acylvaline in an attempt to mimic Ang II binding to the receptor. It is well absorbed orally with a bioavailability of about 25% and the absorption is largely hampered by food intake. It is highly protein bound (~95%), is eliminated mostly by biliary excretion and only 10% of the dosage appears intact in urine. Only about 20% of the dose is metabolized, half of which is believed to be a CYP2C9 mediated hydroxylated product, valeryl 4-hydroxy Valsartan (Fig. 16) [15, 30].
Sacubitril/valsartan (Entresto®) is a co-crystallized combination drug in a one-to-one molar ratio of sacubitril and valsartan. It is a fixed-dose combination medication for use in heart failure. Sacubitril is a neprilysin inhibitor and thus the combination is also known as ARNI. Sacubitril is a prodrug that activates sacubitrilat via esterase hydrolysis Fig. (16). The major limitation of this combination is the potential to develop angioedema, kidney problems, and low blood pressure.
Fig. (16)) Metabolism of valsartan and metabolic activation of sacubitril via esterase hydrolysis. Metabolism of telmisartan. Olmesartan activation.