5,99 €
Mehr erfahren.
- Herausgeber: Shuttle Systems Ltd
- Kategorie: Ratgeber
- Sprache: Englisch
Irritable Bowel Syndrome (IBS) is a common condition that affects millions of people around the world. Symptoms include abdominal pain, bloating, and changes in bowel movements, which can cause discomfort and distress for those who suffer from it. Fortunately, there are many ways to manage IBS and reduce symptoms, and this is where "Irritable Bowel Syndrome: The Complete Guide to Understanding and Managing IBS" comes in.
This comprehensive guide is an essential resource for anyone who has been diagnosed with IBS or suspects they may be experiencing symptoms. With a complete breakdown of what IBS is, its causes, and its symptoms, as well as practical strategies for managing symptoms and improving overall health and wellness.
The book begins with an introduction to IBS, including what it is, how it is diagnosed, and the different types of IBS. It then delves into the various causes of IBS, including diet, stress, and other factors, and provides you with actionable advice for identifying and addressing these underlying causes.
The bulk of the book is dedicated to managing IBS, with detailed chapters on diet and nutrition, stress management, exercise, and other strategies for reducing symptoms and improving overall health.
You will learn about the low-FODMAP diet, a popular dietary approach for managing IBS symptoms, as well as other dietary strategies, such as probiotics and fiber supplements. The book also covers stress management techniques, such as mindfulness and meditation, as well as the benefits of exercise for reducing symptoms.
In addition to practical strategies for managing IBS, the book also provides you with helpful tips for coping with the emotional toll of the condition. Chapters on coping with anxiety and depression, building a support network, and seeking professional help provide you with the tools they need to manage the mental health aspects of IBS.
The author also provides real-life examples of people with IBS who have successfully managed their symptoms, offering inspiration and hope to readers who may be struggling with the condition.
"Irritable Bowel Syndrome: The Complete Guide to Understanding and Managing IBS" is a must-read for anyone who wants to take control of their IBS symptoms and improve their overall health and well-being. With its comprehensive coverage of the condition and practical strategies for managing symptoms, this book is an essential resource for anyone who wants to live a full and healthy life with IBS.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Veröffentlichungsjahr: 2023
Ähnliche
Created by BornIncredible.com
All rights reserved.
Copyright © 2005 onwards .
By reading this book, you agree to the below Terms and Conditions.
BornIncredible.com retains all rights to these products.
No part of this book may be reproduced in any form, by photostat, microfilm, xerography, or any other means, or incorporated into any information retrieval system, electronic or mechanical, without the written permission of BornIncredible.com; exceptions are made for brief excerpts used in published reviews.
This publication is designed to provide accurate and authoritative information with regard to the subject matter covered. It is sold with the understanding that the publisher is not engaged in rendering legal, accounting, health, relationship or other professional / personal advice. If legal advice or other expert assistance is required, the services of a competent professional should be sought.
A New Zealand Made Product
Get A Free Book At: BornIncredible.com/free-book-offer/
Table of Contents
Introduction
What is a IBS?
The Different Types Of IBS
IBS And Inflammatory Bowel Disease (IBD)
The Difference Between IBS And IBD
Strategies For Managing IBS Symptoms When You Have IBD
How do you get IBS
What are the symptoms of IBS
IBS And Chronic Fatigue Syndrome
The Link Between IBS And Chronic Fatigue Syndrome
Strategies For Managing Symptoms When You Have Both Conditions
The Impact Of Chronic Fatigue Syndrome On IBS Symptom Severity
IBS And Chronic Pain
The Link Between IBS And Chronic Pain
Strategies For Managing Chronic Pain With IBS
The Benefits Of A Multidisciplinary Approach To Pain Management
IBS And Autoimmune Diseases
The Link Between IBS And Autoimmune Diseases
Strategies For Managing Symptoms When You Have An Autoimmune Disease
The Impact Of Autoimmune Diseases On IBS Symptom Severity
Another strategy for managing symptoms when you have both IBS and an autoimmune disease is to prioritize self-care. This may involve incorporating regular exercise into your routine, getting adequate sleep, and staying hydrated. Exercise has been shown to be effective in reducing inflammation and improving gut function, while sleep and hydration are essential for overall health and wellbeing. IBS And Pelvic Floor Dysfunction
The Link Between IBS And Pelvic Floor Dysfunction
Strategies For Managing Symptoms Of Pelvic Floor Dysfunction And IBS
The Benefits Of Physical Therapy For Managing Pelvic Floor Dysfunction And IBS
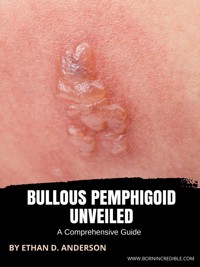
IBS And Skin Conditions
The Link Between IBS And Skin Conditions, Such As Eczema And Psoriasis
IBS And Irritable Bowel Disease-Associated Diarrhea (Ibd-D)
The Link Between IBS And Ibd-D
Strategies For Managing Symptoms When You Have Both Conditions
The Impact Of Ibd-D On IBS Symptom Severity
IBS And Sibo (Small Intestinal Bacterial Overgrowth)
The Link Between IBS And Sibo
Strategies For Managing Symptoms When You Have Both Conditions
The Benefits Of Sibo-Specific Treatment For Managing Symptoms
IBS And Endometriosis
The Link Between IBS And Endometriosis
Strategies For Managing Symptoms When You Have Both Conditions
The Impact Of Endometriosis On IBS Symptom Severity
IBS And Menopause
The Impact Of Menopause On IBS Symptoms
Strategies For Managing Symptoms During Menopause
The Benefits Of Hormone Replacement Therapy For Managing IBS Symptoms During Menopause
IBS And Insomnia
The Impact Of IBS On Insomnia
Strategies For Managing Insomnia With IBS
The Benefits Of Good Sleep Hygiene For Managing IBS Symptoms
What causes irritable bowel syndrome?
How can irritable bowel syndrome be prevented?
How is irritable bowel syndrome diagnosed?
Treatments for IBS
Medications For IBS
Over-The-Counter Medications For Relieving IBS Symptoms
Prescription Medications For Managing IBS
The Potential Risks And Benefits Of Medication Use With IBS
Alternative treatments for IBS
Acupuncture
Hypnotherapy IBS
Other Complementary Therapies For Managing IBS
The Future Of IBS Treatment
Emerging Therapies For IBS
The Potential Impact Of New Treatments On Managing Symptoms
The Importance Of Staying Informed About New Developments In IBS Research And Treatment
The role of diet in IBS
The Role Of The Gut-Brain Axis
Other Nutrition Advice
The Low-Fodmap Diet
Other Dietary Strategies For Managing IBS
The Role Of Probiotics And Fiber Supplements IBS
IBS And Food Intolerances
The Difference Between Food Intolerances And Allergies
Common Food Intolerances That May Exacerbate IBS Symptoms
Strategies For Identifying And Managing Food Intolerances
IBS And Nutrition For Vegetarians And Vegans
Strategies For Managing IBS Symptoms On A Vegetarian Or Vegan Diet
Nutritional Considerations For Those With IBS
The Role Of Plant-Based Foods In Managing IBS Symptoms
The role of stress in IBS
The Impact Of Stress And Anxiety
The Impact Of Stress On IBS Symptoms
The Emotional Toll Of Having IBS
Coping With Anxiety And Depression IBS
The Link Between IBS And Anxiety And Depression
Strategies For Managing Conditions
Strategies for Managing Anxiety and Depression
Mindfulness And Meditation
Other Stress-Reducing Techniques
The Benefits Of Seeking Professional Help IBS
Building A Support Network IBS
The Importance Of Social Support For Managing IBS
Tips For Building A Network Of Supportive People
The Role Of Support Groups In Managing IBS
IBS And Relationships
The Impact Of IBS On Personal Relationships
Strategies For Communicating With Loved Ones
The Importance Of Building Strong Relationships For Managing Symptoms
Living With IBS At Work
Strategies For Managing IBS Symptoms In The Workplace
Tips For Talking To Your Employer About Your Condition
The Impact Of IBS On Work Productivity
Traveling With IBS
Tips For Managing IBS Symptoms While Traveling
Strategies For Planning Ahead And Staying Prepared
The Benefits Of Taking Care Of Yourself While On The Road
Exercise And IBS
The Benefits Of Exercise For Managing IBS
Types Of Exercise That May Be Helpful
Tips For Incorporating Exercise Into Your Routine
Pregnancy And IBS
The Impact Of IBS On Pregnancy
Strategies For Managing Symptoms During Pregnancy
The Safety Of Medication Use During Pregnancy
Children And IBS
The Prevalence Of IBS In Children
Strategies For Managing Symptoms In Kids
The Importance Of Talking To Your Child's Doctor About IBS
IBS And Sleep
The Impact Of IBS On Sleep Quality
Strategies For Improving Sleep With IBS
The Benefits Of A Good Night's Sleep For Managing Symptoms
IBS And Sexual Health
The Impact Of IBS On Sexual Health
Strategies For Managing Symptoms During Sexual Activity
Tips For Talking To Your Partner About IBS
IBS And Aging
The Prevalence Of IBS In Older Adults
Strategies For Managing Symptoms In Older Adults
The Impact Of IBS On Quality Of Life In Older Age
The role of gut microbiota in IBS
IBS And The Gut Microbiome
The Role Of Gut Bacteria In IBS
Strategies For Promoting A Healthy Gut Microbiome
The Potential Benefits Of Microbiome-Targeted Therapies For Managing Symptoms
What are the risks and complications associated with IBS?
Living with Irritable Bowel Syndrome
Lila ‘s Story
Emma’s Story
Sophie’s Story
Natalie’s Story
Olivia’s Story
Emily’s Story
Maggie’s Story
Maria’s Story
Anna’s Story
Your IBS Action Plan
A Step-By-Step Guide For Developing A Personalized IBS Management Plan
Tips For Tracking Symptoms And Progress
The Importance Of Regular Follow-Up With Your Healthcare Provider
The Importance Of Taking A Holistic Approach To Managing IBS
Encouragement
FAQ
What is Irritable Bowel Syndrome
What does your poop look like with IBS?
Does IBS go away on its own?
What food should IBS sufferers avoid?
Is banana good for IBS?
What is the best medication for IBS?
Is yogurt good for IBS?
Is bread good for IBS?
How can I help myself with IBS?
What are 3 symptoms of IBS?
What is the main trigger of IBS?
What foods usually trigger IBS?
What stops an IBS flare up?
What to take to stop an IBS flare up?
How do you detect IBS?
Does coffee irritate IBS?
Where is IBS pain located?
Where is IBS pain located?
Is Metamucil good for IBS?
How do I reset my digestive system with IBS?
Does paracetamol help IBS pain?
Is colonoscopy needed for IBS?
Does IBS show on colonoscopy?
Does IBS show on colonoscopy?
What is IBS
What is the main trigger of IBS?
How can I help myself with IBS?
How do you detect if you have IBS?
What foods usually trigger IBS?
What does your poop look like with IBS?
What should you avoid with IBS?
How many times a day should I poop?
How can you tell the difference between IBS and irritable bowel?
Can you get IBS from stress?
What happens if IBS is not treated?
What are the warning signs of IBS?
What is an IBS flare up like?
How do you test for IBS?
Can you make IBS go away?
How long does a bout of IBS last for?
Can colonoscopy detect IBS?
What food calms IBS?
Is porridge good for IBS?
Can stress cause IBS?
How serious is IBS?
Is there a home test for IBS?
Are probiotics good for IBS?
Can you treat IBS without medication?
Can IBS get worse with age?
Is milk good for IBS?
What is the best yogurt for IBS?
How do you drink coffee with IBS?
Which fruit is good for IBS?
Does green tea help with IBS?
Are apples good for IBS?
Are potatoes good with IBS?
Is dark chocolate good for IBS?
Is peanut butter good for IBS?
Can you suddenly develop IBS?
Is there a cure for IBS?
Will IBS go away on its own?
How do you know if you suffer with IBS?
What should you avoid with IBS?
Where is IBS pain most commonly felt?
Where do you feel IBS discomfort?
How would you describe IBS pain?
Can you suffer with IBS everyday?
What is the difference between IBD and IBS?
Is IBD worse than IBS?
What can be mistaken for IBD?
Have Questions / Comments?
Get Another Book Free
Introduction
If you've ever felt like you can't talk about your digestive issues, you're not alone. IBS can be a difficult condition to manage, but you don't have to suffer in silence.
Irritable bowel syndrome (IBS) is a disorder that affects the large intestine. Symptoms include abdominal pain, diarrhea, constipation, and bloating. IBS can be uncomfortable and embarrassing, but it is not dangerous.
This book will give you everything you need to know about IBS, from causes and symptoms to treatment options. We'll also dispel some common myths about IBS and help you understand how to best manage your condition.
Irritable bowel syndrome (IBS) is a chronic gastrointestinal disorder that affects the large intestine. It is characterized by abdominal pain, bloating, and changes in bowel habits. IBS is a common condition, affecting an estimated 10–15% of the population. While there is no cure for IBS, treatment options are available to manage the symptoms.
This book will provide you with everything you need to know about IBS, from its causes and diagnosis to its symptoms and treatment options. You will also learn tips for coping with the condition and some commonly asked disease-related questions.
What is a IBS?
Irritable Bowel Syndrome (IBS) is a common disorder that affects the large intestine or colon. It is characterized by a group of symptoms that include abdominal pain, bloating, constipation, and diarrhea. IBS is a chronic condition, which means that it can last for a long time, and it can have a significant impact on a person's quality of life.
IBS is classified into four subtypes, based on the predominant symptom: IBS-D (diarrhea-predominant), IBS-C (constipation-predominant), IBS-M (mixed), and IBS-U (unclassified). IBS-D is characterized by frequent, loose stools and the urgent need to have a bowel movement. IBS-C is characterized by infrequent stools and difficulty passing stools. IBS-M is characterized by a combination of diarrhea and constipation. IBS-U is characterized by symptoms that do not meet the criteria for any of the other subtypes.
The exact cause of IBS is not fully understood. However, research suggests that a combination of factors may be involved, including:
Abnormalities in the muscles of the gut, which can cause contractions that are stronger or weaker than normal
Abnormalities in the nerves of the gut, which can cause increased sensitivity to pain
Abnormalities in the immune system
Abnormalities in the gut bacteria
Gastrointestinal infections
Psychological factors, such as stress and anxiety
A diagnosis of IBS is made based on the presence of certain symptoms, as there are no specific tests for the disorder. A doctor will typically use the Rome III criteria to make a diagnosis of IBS, which include the presence of abdominal pain or discomfort for at least 12 weeks (not necessarily consecutive) in the last 12 months, and two or more of the following:
The pain or discomfort is relieved by having a bowel movement
The pain or discomfort is associated with a change in the frequency of bowel movements
The pain or discomfort is associated with a change in the appearance of the stool
Treatment for IBS typically involves a combination of lifestyle changes and medication. Lifestyle changes that may be recommended include:
Eating a diet high in fruits, vegetables, and whole grains
Drinking plenty of fluids
Exercising regularly
Managing stress
Medications that may be prescribed for IBS include:
Antispasmodics, which can help to relax the muscles in the gut and reduce cramping
Laxatives, which can help to relieve constipation
Antidepressants, which can help to reduce pain and improve bowel function
Antibiotics, which can help to improve gut health by altering the balance of gut bacteria
IBS is a common disorder that affects the large intestine, or colon. It is characterized by a group of symptoms that include abdominal pain, bloating, constipation, and diarrhea. IBS is a chronic condition, which means that it can last for a long time, and it can have a significant impact on a person's quality of life.
IBS is a multifactorial disorder, it's caused by a combination of abnormalities in the muscles of the gut, nerves of the gut, immune system, gut bacteria, gastrointestinal infections and psychological factors, such as stress and anxiety.
A diagnosis of IBS is made based on the presence of certain symptoms, as there are no specific tests for the disorder. A doctor will typically use the Rome III criteria to make a diagnosis of IBS.
Treatment for IBS typically involves a combination of lifestyle changes and medication. Lifestyle changes
The Different Types Of IBS
Irritable Bowel Syndrome (IBS) is a gastrointestinal disorder that affects millions of people worldwide. It is characterized by a group of symptoms that includes abdominal pain, bloating, and changes in bowel movements. While the exact cause of IBS is not known, it is believed to be related to changes in the way the muscles in the bowel contract and relax, changes in the way the brain and gut communicate, and changes in the gut microbiome.
There are several types of IBS, each with its own set of symptoms and diagnostic criteria. Understanding the different types of IBS is essential for effective diagnosis and management of the condition. Below we will discuss the four main types of IBS and their associated symptoms.
IBS-D (Diarrhea-Predominant IBS)
IBS-D is the most common type of IBS and is characterized by frequent loose or watery stools, urgency, and an increased frequency of bowel movements. Individuals with IBS-D may also experience abdominal pain and cramping, bloating, and gas. The symptoms of IBS-D are often triggered by food, stress, or hormonal changes.
To be diagnosed with IBS-D, a person must have experienced diarrhea or loose stools for at least three months, along with other symptoms such as abdominal pain or discomfort, bloating, or changes in bowel habits. Additional tests may be required to rule out other conditions that can cause similar symptoms, such as inflammatory bowel disease or celiac disease.
Management of IBS-D typically involves dietary changes, such as avoiding trigger foods and increasing fiber intake, as well as stress reduction techniques and medication, such as antidiarrheals or laxatives.
IBS-C (Constipation-Predominant IBS)
IBS-C is characterized by infrequent bowel movements or difficulty passing stools, along with abdominal pain, discomfort, bloating, and gas. Individuals with IBS-C may also experience straining during bowel movements and a feeling of incomplete evacuation.
To be diagnosed with IBS-C, a person must have experienced constipation or hard, lumpy stools for at least three months, along with other symptoms such as abdominal pain or discomfort, bloating, or changes in bowel habits. Additional tests may be required to rule out other conditions that can cause similar symptoms, such as colon cancer or hypothyroidism.
Management of IBS-C typically involves dietary changes, such as increasing fiber intake and drinking plenty of fluids, as well as stress reduction techniques and medication, such as laxatives or stool softeners.
IBS-M (Mixed IBS)
IBS-M is characterized by a combination of symptoms of IBS-D and IBS-C, with alternating periods of constipation and diarrhea. Individuals with IBS-M may also experience abdominal pain, discomfort, bloating, and gas.
To be diagnosed with IBS-M, a person must have experienced a combination of symptoms of IBS-D and IBS-C for at least three months, along with other symptoms such as abdominal pain or discomfort, bloating, or changes in bowel habits. Additional tests may be required to rule out other conditions that can cause similar symptoms.
Management of IBS-M typically involves a combination of dietary changes, stress reduction techniques, and medication, depending on the predominant symptoms. For example, if constipation is the predominant symptom, laxatives or stool softeners may be recommended, while antidiarrheals may be recommended for diarrhea.
Post-Infectious IBS (PI-IBS)
Post-Infectious IBS (PI-IBS) is a type of IBS that develops after an acute episode of infectious diarrhea. PI-IBS is characterized by persistent abdominal pain, discomfort, and changes in bowel habits that develop after an episode of infectious diarrhea. The acute episode of infectious diarrhea can be caused by a bacterial, viral, or parasitic infection, and the symptoms of PI-IBS typically develop within a few weeks to a few months after the initial infection.
IBS And Inflammatory Bowel Disease (IBD)
Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are two gastrointestinal conditions that can have a significant impact on a person's quality of life. While these conditions share some similarities, they are distinct and require different treatment approaches. Below we will explore the differences between IBS and IBD and the potential impact of IBS on IBD.
What is IBS?
IBS is a common gastrointestinal disorder characterized by abdominal pain and changes in bowel movements such as diarrhea, constipation, or a combination of the two. Other symptoms may include bloating, gas, and nausea. IBS does not cause inflammation or damage to the intestines, and it does not increase the risk of developing colon cancer.
What is IBD?
IBD is a group of chronic inflammatory conditions that affect the digestive tract. The two main types of IBD are Crohn's disease and ulcerative colitis. Crohn's disease can affect any part of the digestive tract, while ulcerative colitis affects only the colon and rectum. In addition to abdominal pain and changes in bowel movements, symptoms of IBD may include fever, fatigue, weight loss, and blood in the stool. IBD can cause inflammation and damage to the intestines, and it increases the risk of developing colon cancer.
The Differences Between IBS and IBD
While IBS and IBD share some symptoms, there are several key differences between the two conditions. One of the main differences is that IBS does not cause inflammation or damage to the intestines, while IBD does. Additionally, IBS does not increase the risk of developing colon cancer, while IBD does.
Another difference is that IBS is a functional disorder, meaning that it affects how the digestive tract functions, while IBD is an inflammatory disorder, meaning that it involves inflammation of the digestive tract.
Diagnosis and Treatment
Diagnosing IBS and IBD can be challenging, as symptoms can overlap and mimic other conditions. A healthcare provider may use a combination of physical exams, medical history, and tests such as colonoscopy or stool tests to diagnose the conditions.
Treatment for IBS and IBD also differs. While dietary modifications can be helpful for managing symptoms of both conditions, medication is often required for IBD to manage inflammation and prevent complications. Surgery may also be necessary for some individuals with IBD.
The Impact of IBS on IBD
While IBS and IBD are distinct conditions, they can coexist, and the presence of IBS can impact the course of IBD. In one study, researchers found that individuals with both IBS and IBD had more severe abdominal pain and bloating than those with IBD alone. Additionally, individuals with both conditions had lower quality of life and greater functional disability than those with IBD alone.
Another study found that the presence of IBS was associated with a higher risk of flares in individuals with Crohn's disease. The study also found that individuals with both conditions were more likely to require hospitalization and surgery than those with IBD alone.
Managing Symptoms When You Have Both Conditions
Managing symptoms when you have both IBS and IBD can be challenging, but there are strategies that can help. One strategy is to address common triggers such as stress and dietary triggers. Stress management techniques such as meditation, deep breathing, and progressive muscle relaxation can be helpful in reducing stress and alleviating symptoms.
Dietary modifications can also be an effective strategy for managing symptoms. A low-FODMAP diet, which restricts certain types of carbohydrates that can contribute to IBS symptoms, can be helpful for managing symptoms of both conditions.
In addition to dietary modifications, medication is often necessary for managing IBD symptoms.
The Difference Between IBS And IBD
Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are two conditions that can affect the gastrointestinal tract, but they have distinct differences. It is important to understand the differences between these conditions as the treatment and management approaches for each differ significantly. Below we will explore the differences between IBS and IBD.
What is IBS?
IBS is a functional gastrointestinal disorder that affects the large intestine. It is characterized by chronic abdominal pain, bloating, and changes in bowel habits such as diarrhea, constipation, or both. Other common symptoms of IBS include gas, mucus in the stool, and a feeling of incomplete bowel movement.
IBS is a chronic condition that can significantly affect a person's quality of life. However, IBS does not cause inflammation or damage to the intestines, and it is not associated with an increased risk of developing colon cancer.
What is IBD?
IBD is a group of chronic inflammatory conditions that affect the gastrointestinal tract. The two most common types of IBD are Crohn's disease and ulcerative colitis. Crohn's disease can affect any part of the gastrointestinal tract, from the mouth to the anus. In contrast, ulcerative colitis only affects the colon and rectum.
IBD causes inflammation and ulcers in the lining of the intestines, leading to symptoms such as chronic diarrhea, abdominal pain, rectal bleeding, weight loss, and fatigue. IBD is also associated with an increased risk of developing colon cancer.
The Differences Between IBS and IBD
While IBS and IBD can have some overlapping symptoms, there are several key differences between the two conditions.
Inflammation
IBS does not cause inflammation or damage to the intestines, whereas IBD does. The inflammation in IBD can lead to complications such as strictures (narrowing of the intestinal passage), abscesses, and fistulas.
Colon Cancer Risk
IBS is not associated with an increased risk of developing colon cancer. In contrast, individuals with IBD are at an increased risk of developing colon cancer, particularly if they have had the disease for an extended period.
Severity
IBS symptoms can range from mild to severe, and they often come and go over time. In contrast, IBD is typically a more severe and chronic condition that requires ongoing medical management.
Diagnosis
Diagnosing IBS is based on the patient's symptoms, medical history, and physical exam. In contrast, diagnosing IBD requires a combination of tests, such as blood tests, stool tests, endoscopy, and imaging studies.
Treatment Differences Between IBS and IBD
While there are some similarities in the management of IBS and IBD, the treatment approaches differ significantly.
Medications
There is no cure for IBS, and treatment is focused on managing symptoms. Medications that may be used to treat IBS include antispasmodics, laxatives, and antidepressants. However, medication may not always be effective in managing symptoms.
In contrast, medications are a primary treatment for IBD. Anti-inflammatory medications such as corticosteroids, immunomodulators, and biologics are commonly used to reduce inflammation and prevent complications.
Surgery
Surgery may be necessary for individuals with IBD who do not respond to medication or who develop complications such as strictures or fistulas. Surgery is not typically used to treat IBS.
Dietary Modifications
Dietary modifications may be helpful in managing symptoms for both IBS and IBD. A low-FODMAP diet may be effective in reducing symptoms of IBS, while a low-residue diet may be helpful for individuals with IBD during flares.
Strategies For Managing IBS Symptoms When You Have IBD
Managing symptoms when you have both Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) can be challenging. Since IBS is a functional disorder while IBD is an inflammatory condition, there are differences in the management approaches for each. However, there are still some strategies that can help manage symptoms when you have both conditions. Below we will discuss some strategies for managing IBS symptoms when you have IBD.
Identify Trigger Foods
Dietary modifications may be helpful in managing symptoms of both IBS and IBD. Identifying trigger foods that can exacerbate symptoms is an essential step in managing both conditions. It is important to work with a registered dietitian to develop a personalized diet plan that meets your nutritional needs while avoiding trigger foods.
For individuals with IBS, a low-FODMAP diet may be effective in reducing symptoms such as bloating, gas, and abdominal pain. However, some foods that are high in FODMAPs may also be beneficial for individuals with IBD, such as prebiotics, which can improve gut health.
Manage Stress
Stress can trigger symptoms in both IBS and IBD. Therefore, managing stress is an important aspect of managing symptoms. Strategies such as mindfulness meditation, deep breathing exercises, and yoga can help reduce stress and improve overall well-being.
Exercise
Regular exercise can also be helpful in managing symptoms of both conditions. Exercise can help reduce stress, improve bowel function, and decrease inflammation. However, it is important to consult with a healthcare provider before starting a new exercise routine, particularly if you have IBD.
Medication
Medication may be necessary for individuals with IBD to reduce inflammation and prevent complications. However, some medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), can exacerbate symptoms in individuals with IBS. Therefore, it is important to work with a healthcare provider to determine the best medication regimen for managing both conditions.
Support
Having a support network can be beneficial for managing symptoms when you have both IBS and IBD. Support can come from family, friends, support groups, or healthcare providers. Having someone to talk to about your symptoms can help reduce stress and anxiety and provide emotional support.
Stay Hydrated
Staying hydrated is essential for managing both IBS and IBD. Dehydration can exacerbate symptoms such as constipation, bloating, and abdominal pain. Drinking enough water and other fluids can help maintain proper bowel function and prevent dehydration.
Avoid Triggers
Avoiding triggers that can exacerbate symptoms is an essential aspect of managing both conditions. Common triggers for IBS include fatty foods, caffeine, alcohol, and spicy foods. Common triggers for IBD include high-fiber foods, dairy products, and certain types of carbohydrates.
Get Enough Sleep
Getting enough sleep is essential for managing symptoms of both IBS and IBD. Lack of sleep can exacerbate symptoms such as fatigue, brain fog, and abdominal pain. Developing healthy sleep habits such as establishing a regular sleep schedule, avoiding caffeine before bedtime, and creating a comfortable sleep environment can help improve sleep quality.
Take Breaks
Taking breaks throughout the day can be helpful in managing symptoms when you have both conditions. This can include taking short walks, stretching, or practicing relaxation techniques. Taking breaks can help reduce stress, improve bowel function, and increase overall well-being.
Work with Healthcare Providers
Working with healthcare providers is essential for managing both IBS and IBD. It is important to communicate any changes in symptoms or concerns with your healthcare provider. They can provide guidance on the best management approaches and make any necessary medication adjustments.
How do you get IBS
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that affects the large intestine. The exact cause of IBS is not known, but it is believed to be a combination of factors, including abnormalities in the muscles of the gut, changes in the gut microbiome, and psychological factors such as stress and anxiety.
One theory is that IBS is caused by abnormal muscle contractions in the gut, known as motility. These contractions can be either too strong or too weak, which can cause pain and discomfort. In addition, people with IBS may have a heightened sensitivity to certain stimuli, such as gas or pressure, which can worsen symptoms.
Another theory is that IBS is related to changes in the gut microbiome. The gut microbiome is the collection of microorganisms that live in the gut and play a role in digestion and overall health. Changes in the gut microbiome, such as an overgrowth of certain bacteria, can disrupt the balance of microorganisms and lead to symptoms of IBS.
Certain foods can also trigger IBS symptoms. Common trigger foods include:
High-FODMAP foods, which are high in certain sugars that can be difficult for some people to digest:
Gluten
Dairy products
Fried foods
Caffeine
Alcohol
Stress and anxiety can also play a role in the development of IBS. Stress can affect the muscles of the gut and disrupt the balance of microorganisms in the gut. In addition, people with IBS often experience a vicious cycle of stress, anxiety, and symptoms, which can make their condition worse.
IBS can also be diagnosed by ruling out other conditions such as inflammatory bowel disease, celiac disease, and colorectal cancer. A range of diagnostic tests such as colonoscopy, stool testing, blood tests, and imaging studies can be used to rule out these conditions.
In conclusion, the causes of IBS are not fully understood, but it is believed to be a combination of factors including abnormal muscle contractions in the gut, changes in the gut microbiome, and psychological factors such as stress and anxiety. Certain foods can also trigger IBS symptoms. It's important to see a doctor if you suspect you may have IBS, as other conditions need to be ruled out. A combination of dietary changes, medication, and stress management techniques may be used to manage symptoms.
What are the symptoms of IBS
IBS, or Irritable Bowel Syndrome, is a common gastrointestinal disorder characterized by a group of symptoms that can vary from person to person. The most common symptoms of IBS include:
Abdominal pain or discomfort: This is often described as a cramping, bloating, or gas-like feeling in the abdomen. The pain may be relieved by having a bowel movement.
Changes in bowel habits: People with IBS may experience constipation (difficulty having a bowel movement or passing hard stools) or diarrhea (frequent loose stools or urgent bowel movements). Some people may alternate between constipation and diarrhea.
Gas and bloating: Many people with IBS experience excessive gas and bloating, which can be uncomfortable and embarrassing.
Mucus in the stool: Some people with IBS may notice an increase in the amount of mucus in their stool, which can be clear or white.
Fatigue: People with IBS may experience fatigue or a lack of energy, which can be caused by a combination of factors such as poor sleep, pain, and stress.
Nausea: Some people with IBS may experience nausea, which can be caused by a variety of factors such as stomach pain, bloating, and changes in bowel habits.
Anxiety and Depression: Many people with IBS also experience anxiety and depression, which can be caused by a combination of factors such as chronic pain, fatigue, and the emotional impact of having a chronic illness.
Other symptoms that may be associated with IBS include:
Headaches: Some people with IBS may experience headaches, which can be caused by a combination of factors such as stress, poor sleep, and changes in bowel habits.
Back pain: Some people with IBS may experience back pain, which can be caused by a variety of factors such as muscle tension, poor posture, and changes in bowel habits.
Urgency: Some people with IBS may experience a feeling of urgency to have a bowel movement, which can be caused by a variety of factors such as changes in bowel habits, gas and bloating, and abdominal pain.
It's worth noting that the symptoms can vary from person to person and can be different from one episode to another. Additionally, some people with IBS may have fewer symptoms, while others may have more severe symptoms.
It's also worth mentioning that IBS is a functional disorder, which means that there is no structural or biochemical abnormalities found in the gut. It's diagnosed based on symptoms and ruling out other possible causes of the symptoms.
It's important to note that while the symptoms of IBS can be uncomfortable and disruptive, they are not typically dangerous or life-threatening. However, if you experience severe symptoms, such as rectal bleeding, weight loss, or persistent fever, it's important to seek medical attention, as these symptoms may be caused by a more serious condition.
If you are experiencing symptoms of IBS, it's important to talk to your doctor to get an accurate diagnosis and to develop an effective treatment plan. The treatment for IBS can include lifestyle changes such as improving diet, stress management, and regular exercise. Medications such as antispasmodics and laxatives can also be used to help relieve symptoms. In some cases, psychological therapy may be helpful in managing the emotional impact of living with a chronic illness.
IBS And Chronic Fatigue Syndrome
Irritable Bowel Syndrome (IBS) and Chronic Fatigue Syndrome (CFS) are two chronic conditions that can significantly impact an individual's quality of life. Below we will explore the link between IBS and CFS and discuss strategies for managing symptoms to improve quality of life.
The Link Between IBS and CFS
IBS and CFS share many common symptoms, including fatigue, abdominal pain, and sleep disturbances. Additionally, both conditions are associated with changes in the immune system, which can contribute to the development of symptoms.
Research suggests that there may be a bidirectional relationship between IBS and CFS, meaning that individuals with one condition are more likely to develop the other. It is thought that the chronic stress associated with IBS can contribute to the development of CFS, and vice versa.
Physical Symptoms
The physical symptoms of IBS and CFS can significantly impact quality of life. Fatigue, abdominal pain, and sleep disturbances can interfere with daily activities such as work, exercise, and socializing.
In addition, individuals with these conditions may experience other physical symptoms related to aging, such as joint pain, which can further exacerbate the impact of symptoms.
Emotional Health
IBS and CFS can also have a significant impact on emotional health. The chronic nature of these conditions can lead to feelings of frustration, anxiety, and depression, particularly if symptoms are severe or difficult to manage.
Furthermore, individuals with IBS and CFS may feel embarrassed or ashamed to discuss their symptoms, which can lead to social isolation and a reduced quality of life.
Social Isolation
Social isolation can be a significant problem for individuals with IBS and CFS. Individuals with these conditions may avoid social situations or activities due to fear of embarrassment or discomfort related to their symptoms.
This can lead to feelings of loneliness and isolation, which can further exacerbate emotional health issues and impact quality of life.
Strategies for Managing IBS and CFS Symptoms
Diet
Dietary modifications can be an effective strategy for managing symptoms of IBS and CFS. A low-FODMAP diet, which restricts certain types of carbohydrates that can contribute to IBS symptoms, can be particularly helpful for managing symptoms.
Additionally, it is important for individuals with CFS to eat a well-balanced diet to ensure they are getting the nutrients they need to manage symptoms and maintain overall health.
It is important for individuals with IBS and CFS to work closely with a healthcare provider or a registered dietitian to develop a personalized dietary plan that takes into account their medical history, medications, and other dietary restrictions.
Exercise
Regular exercise can help regulate bowel movements and reduce stress, which can alleviate symptoms of IBS and CFS. However, it is important to start slowly and gradually increase activity levels to avoid exacerbating symptoms.
Individuals with CFS may need to engage in low-impact exercises such as walking or yoga to avoid overexertion.
It is important for individuals with IBS and CFS to consult with a healthcare provider before starting any new exercise program to ensure safety and efficacy.
Medication
Medications can be used to manage symptoms of IBS and CFS. Over-the-counter medications such as antidiarrheals and laxatives can be used to manage specific symptoms.
Prescription medications such as antidepressants and antispasmodics can be used to manage overall symptoms. However, medication use should be closely monitored by a healthcare provider to ensure safety and efficacy.
Stress Management
Stress management techniques such as meditation, deep breathing, and progressive muscle relaxation can help reduce stress and alleviate symptoms of IBS and CFS.
The Link Between IBS And Chronic Fatigue Syndrome
Irritable Bowel Syndrome (IBS) and Chronic Fatigue Syndrome (CFS) are two chronic conditions that share many common symptoms and often coexist in the same individual. Below we will explore the link between IBS and CFS and discuss strategies for managing symptoms to improve quality of life.
The Link Between IBS and CFS
IBS and CFS share many common symptoms, including fatigue, abdominal pain, and sleep disturbances. Additionally, both conditions are associated with changes in the immune system, which can contribute to the development of symptoms.
Research suggests that there may be a bidirectional relationship between IBS and CFS, meaning that individuals with one condition are more likely to develop the other. It is thought that the chronic stress associated with IBS can contribute to the development of CFS, and vice versa.
Physical Symptoms
The physical symptoms of IBS and CFS can significantly impact quality of life. Fatigue, abdominal pain, and sleep disturbances can interfere with daily activities such as work, exercise, and socializing.
In addition, individuals with these conditions may experience other physical symptoms related to aging, such as joint pain, which can further exacerbate the impact of symptoms.
Emotional Health
IBS and CFS can also have a significant impact on emotional health. The chronic nature of these conditions can lead to feelings of frustration, anxiety, and depression, particularly if symptoms are severe or difficult to manage.
Furthermore, individuals with IBS and CFS may feel embarrassed or ashamed to discuss their symptoms, which can lead to social isolation and a reduced quality of life.
Social Isolation
Social isolation can be a significant problem for individuals with IBS and CFS. Individuals with these conditions may avoid social situations or activities due to fear of embarrassment or discomfort related to their symptoms.
This can lead to feelings of loneliness and isolation, which can further exacerbate emotional health issues and impact quality of life.
Strategies for Managing IBS and CFS Symptoms
Diet
Dietary modifications can be an effective strategy for managing symptoms of IBS and CFS. A low-FODMAP diet, which restricts certain types of carbohydrates that can contribute to IBS symptoms, can be particularly helpful for managing symptoms.
Additionally, it is important for individuals with CFS to eat a well-balanced diet to ensure they are getting the nutrients they need to manage symptoms and maintain overall health.
It is important for individuals with IBS and CFS to work closely with a healthcare provider or a registered dietitian to develop a personalized dietary plan that takes into account their medical history, medications, and other dietary restrictions.
Exercise
Regular exercise can help regulate bowel movements and reduce stress, which can alleviate symptoms of IBS and CFS. However, it is important to start slowly and gradually increase activity levels to avoid exacerbating symptoms.
Individuals with CFS may need to engage in low-impact exercises such as walking or yoga to avoid overexertion.
It is important for individuals with IBS and CFS to consult with a healthcare provider before starting any new exercise program to ensure safety and efficacy.
Medication
Medications can be used to manage symptoms of IBS and CFS. Over-the-counter medications such as antidiarrheals and laxatives can be used to manage specific symptoms.
Prescription medications such as antidepressants and antispasmodics can be used to manage overall symptoms. However, medication use should be closely monitored by a healthcare provider to ensure safety and efficacy.
Stress Management
Stress management techniques such as meditation, deep breathing, and progressive muscle relaxation can help reduce stress and alleviate symptoms of IBS and CFS. Additionally, seeking professional help from a therapist or counselor can provide support
Strategies For Managing Symptoms When You Have Both Conditions
Managing symptoms when you have both Irritable Bowel Syndrome (IBS) and Chronic Fatigue Syndrome (CFS) can be challenging. The overlap of symptoms and the complexity of managing multiple chronic conditions can make it difficult to find effective strategies for improving quality of life. Below we will explore strategies for managing symptoms when you have both IBS and CFS.
Keep a Symptom Diary
Keeping a symptom diary can be helpful in identifying triggers and patterns of symptoms. Record your symptoms, the time of day they occur, and any other factors that may be contributing to your symptoms, such as diet or stress. This can help you identify triggers and develop strategies for managing symptoms.
Practice Stress Management Techniques
Stress can be a significant trigger for both IBS and CFS symptoms. Practicing stress management techniques such as meditation, deep breathing, and progressive muscle relaxation can help reduce stress and alleviate symptoms.
Adjust Your Diet
Dietary modifications can be an effective strategy for managing symptoms of both IBS and CFS. A low-FODMAP diet, which restricts certain types of carbohydrates that can contribute to IBS symptoms, can be particularly helpful for managing symptoms.
Additionally, it is important to eat a well-balanced diet to ensure you are getting the nutrients you need to manage symptoms and maintain overall health. It is important to work closely with a healthcare provider or a registered dietitian to develop a personalized dietary plan that takes into account your medical history, medications, and other dietary restrictions.
Engage in Regular Exercise
Regular exercise can help regulate bowel movements and reduce stress, which can alleviate symptoms of both IBS and CFS. However, it is important to start slowly and gradually increase activity levels to avoid exacerbating symptoms.
Individuals with CFS may need to engage in low-impact exercises such as walking or yoga to avoid overexertion. It is important to consult with a healthcare provider before starting any new exercise program to ensure safety and efficacy.
Get Adequate Sleep
Sleep disturbances can be a significant problem for individuals with both IBS and CFS. Getting adequate sleep can help alleviate symptoms and improve overall quality of life. Establishing a regular sleep schedule, avoiding caffeine and alcohol before bedtime, and creating a relaxing sleep environment can all help improve sleep quality.
Seek Professional Help
Managing multiple chronic conditions can be challenging, and it may be necessary to seek professional help. A healthcare provider can help develop a personalized treatment plan that takes into account both conditions and any medications or treatments that may interact.
Additionally, seeking professional help from a therapist or counselor can provide support for managing the emotional toll of living with both conditions.
Build a Support Network
Building a support network can be helpful for managing symptoms and reducing social isolation. Connecting with others who have similar experiences can provide a sense of community and support. Support groups or online forums can be a helpful resource for finding others who understand what you are going through.
Be Kind to Yourself
Living with chronic conditions can be challenging, and it is important to be kind to yourself. Practice self-care and prioritize activities that bring you joy and relaxation. Recognize that managing symptoms is a process, and it may take time to find effective strategies for managing both conditions.
In conclusion, managing symptoms when you have both IBS and CFS requires a multifaceted approach that addresses both physical and emotional health. Strategies such as stress management techniques, dietary modifications, regular exercise, and seeking professional help can all be effective in managing symptoms and improving quality of life.
The Impact Of Chronic Fatigue Syndrome On IBS Symptom Severity
Chronic Fatigue Syndrome (CFS) and Irritable Bowel Syndrome (IBS) are two chronic conditions that can have a significant impact on a person's quality of life. While these conditions are distinct, they often co-occur and can have a synergistic effect on symptom severity. Below we will explore the impact of CFS on IBS symptom severity.
What is Chronic Fatigue Syndrome?
Chronic Fatigue Syndrome is a complex disorder characterized by persistent fatigue that is not alleviated by rest and cannot be attributed to an underlying medical condition. In addition to fatigue, individuals with CFS may experience other symptoms such as cognitive difficulties, sleep disturbances, and joint pain.
What is Irritable Bowel Syndrome?
Irritable Bowel Syndrome is a common gastrointestinal disorder characterized by abdominal pain and changes in bowel movements such as diarrhea, constipation, or a combination of the two. Other symptoms may include bloating, gas, and nausea.
The Link Between CFS and IBS
There is a high prevalence of co-occurring CFS and IBS. In fact, research has shown that up to 50% of individuals with CFS also meet criteria for a diagnosis of IBS.
The link between these two conditions is not well understood, but there are several theories. One theory is that the two conditions share common underlying pathophysiology, such as inflammation and dysregulation of the immune system. Additionally, stress is a known trigger for both conditions and may contribute to symptom exacerbation.
Impact of CFS on IBS Symptom Severity
The presence of CFS in individuals with IBS can significantly impact symptom severity. In one study, researchers found that individuals with both CFS and IBS had more severe abdominal pain and diarrhea symptoms than those with IBS alone. Additionally, individuals with both conditions had higher levels of anxiety and depression.
Another study found that individuals with both CFS and IBS had more severe gastrointestinal symptoms, greater disability, and poorer quality of life than those with IBS alone. The study also found that the severity of CFS symptoms was a significant predictor of the severity of IBS symptoms.
Managing Symptoms When You Have Both Conditions
Managing symptoms when you have both CFS and IBS can be challenging. The overlap of symptoms and the complexity of managing multiple chronic conditions can make it difficult to find effective strategies for improving quality of life.
One strategy for managing symptoms is to address common triggers. For example, stress is a known trigger for both conditions, and stress management techniques such as meditation, deep breathing, and progressive muscle relaxation can be helpful in reducing stress and alleviating symptoms.
Dietary modifications can also be an effective strategy for managing symptoms of both conditions. A low-FODMAP diet, which restricts certain types of carbohydrates that can contribute to IBS symptoms, can be particularly helpful for managing symptoms.
Additionally, engaging in regular exercise can help regulate bowel movements and reduce stress, which can alleviate symptoms of both conditions. However, it is important to start slowly and gradually increase activity levels to avoid exacerbating symptoms.
Individuals with CFS may need to engage in low-impact exercises such as walking or yoga to avoid overexertion. It is important to consult with a healthcare provider before starting any new exercise program to ensure safety and efficacy.
Sleep disturbances can be a significant problem for individuals with both IBS and CFS. Getting adequate sleep can help alleviate symptoms and improve overall quality of life. Establishing a regular sleep schedule, avoiding caffeine and alcohol before bedtime, and creating a relaxing sleep environment can all help improve sleep quality.
Seeking professional help from a healthcare provider or therapist can provide support for managing symptoms and improving quality of life. A healthcare provider can help develop a personalized treatment plan that takes into account both conditions and any medications that could help.
IBS And Chronic Pain
One of the most common symptoms experienced by people with IBS is chronic pain, which can be debilitating and have a significant impact on their quality of life. Below we will explore the link between IBS and chronic pain, as well as strategies for managing pain associated with IBS.
The exact cause of IBS is still not fully understood, but research has shown that it is a complex condition that involves multiple factors. It is thought to be caused by a combination of genetic, environmental, and psychological factors. One of the hallmarks of IBS is abdominal pain or discomfort that is associated with changes in bowel movements. This pain can be crampy, sharp, or dull, and it can be constant or come and go. In some cases, the pain is so severe that it can be disabling.
Chronic pain is a common symptom of IBS, and it can have a significant impact on a person's quality of life. In addition to abdominal pain, people with IBS may experience pain in other parts of the body, such as the back, joints, and muscles. This pain can be caused by the stress and anxiety associated with living with a chronic condition like IBS, as well as by the physical changes that occur in the body as a result of the condition.
Managing chronic pain associated with IBS can be challenging, but there are a number of strategies that can be effective. One of the most important things that people with IBS can do is to develop a good understanding of their condition and the factors that can trigger symptoms. This can help them to identify the things that make their pain worse and to develop a plan for managing their symptoms.
One of the most effective strategies for managing chronic pain associated with IBS is to make lifestyle changes. This may include things like reducing stress, getting regular exercise, and eating a healthy diet. These changes can help to reduce inflammation in the body and promote healing, which can help to reduce pain and discomfort associated with IBS.
In addition to lifestyle changes, there are a number of medications that can be effective for managing chronic pain associated with IBS. These include antispasmodics, which help to reduce muscle spasms in the intestines, and antidepressants, which can help to reduce pain and improve mood. Other medications that may be helpful include pain relievers, laxatives, and fiber supplements.
Another strategy for managing chronic pain associated with IBS is to work with a healthcare professional or therapist. These professionals can provide support and guidance for managing symptoms, as well as help people with IBS to develop coping strategies for dealing with pain and other symptoms. This may include things like relaxation techniques, mindfulness meditation, and cognitive-behavioral therapy.
It is important for people with IBS to remember that chronic pain is a common symptom of the condition, and that it can be managed with the right strategies and support. It is also important to be patient and persistent in seeking relief, as it may take some time to find the right combination of strategies and treatments that work best for you.
In conclusion, chronic pain is a common symptom of IBS that can have a significant impact on a person's quality of life. However, there are a number of strategies that can be effective for managing pain associated with IBS. These include lifestyle changes, medications, working with healthcare professionals or therapists, and developing coping strategies for dealing with pain and other symptoms. With the right strategies and support, people with IBS can manage their symptoms and lead full, healthy lives.
The Link Between IBS And Chronic Pain
Irritable Bowel Syndrome (IBS) is a condition that affects millions of people around the world. It is characterized by chronic gastrointestinal symptoms such as abdominal pain, bloating, and altered bowel habits. Chronic pain is one of the most common symptoms of IBS, and it can significantly impact a person's quality of life. Below we will explore the link between IBS and chronic pain, as well as strategies for managing chronic pain in IBS patients.
IBS is a functional gastrointestinal disorder, which means that it is a condition in which the digestive system does not function properly, even though there are no visible signs of disease or damage. It is thought to be caused by a combination of factors, including genetics, diet, stress, and abnormalities in the gut microbiome. One of the most common symptoms of IBS is chronic pain, which can be severe and debilitating for some patients.
Chronic pain is defined as pain that persists for more than 3 months and interferes with daily activities. IBS-related pain can occur anywhere in the abdomen and can be sharp, dull, or crampy. It can also be associated with other symptoms such as bloating, nausea, and changes in bowel habits. Chronic pain can significantly impact a person's quality of life, leading to sleep disturbances, anxiety, depression, and decreased productivity.
The link between IBS and chronic pain is not fully understood, but it is thought to be related to the hypersensitivity of the gut. In IBS patients, the nerves in the gut may be more sensitive to stimulation, leading to the perception of pain at lower thresholds. In addition, chronic pain can lead to changes in the brain and nervous system, which can further exacerbate pain perception.
Managing chronic pain in IBS patients can be challenging, as traditional pain management strategies may not be effective for this population. Over-the-counter pain relievers such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) may be ineffective or even exacerbate symptoms in some IBS patients. Opioids, while effective for pain management, are not recommended for the treatment of IBS-related pain due to the risk of addiction and dependence.
Fortunately, there are a number of strategies that can be effective in managing chronic pain in IBS patients. These include:
1. Dietary changes: Certain foods and beverages, such as caffeine, alcohol, and spicy foods, can trigger IBS symptoms and exacerbate pain. Avoiding these triggers and following a low FODMAP diet may be helpful in reducing pain and other IBS symptoms.
2. Stress management: Stress and anxiety can exacerbate pain and other IBS symptoms. Relaxation techniques such as deep breathing, meditation, and yoga may be effective in reducing stress and pain.
3. Exercise: Exercise has been shown to be effective in reducing chronic pain in many conditions, including IBS. Low-impact activities such as walking, swimming, and cycling may be effective in reducing pain and improving overall health.
4. Gut-directed hypnotherapy: This is a type of therapy that focuses on changing the brain-gut connection through relaxation and visualization techniques. It has been shown to be effective in reducing pain and other IBS symptoms.
5. Cognitive-behavioral therapy: This is a type of therapy that focuses on changing negative thought patterns and behaviors that can exacerbate pain and other symptoms. It has been shown to be effective in reducing pain and improving quality of life in IBS patients.
6. Medications: There are a number of medications that may be effective in managing chronic pain in IBS patients, including antispasmodics, tricyclic antidepressants, and selective serotonin reuptake inhibitors (SSRIs).