The Distracted Couple E-Book
Erhalten Sie Zugang zu diesem und mehr als 300000 Büchern ab EUR 5,99 monatlich.
- Herausgeber: Crown House Publishing
- Kategorie: Fachliteratur
- Sprache: Englisch
In total, this volume addresses many of the issues that couples face when either one or both partners has ADHD and the many ways that clinicians can help them in dealing with these issues.Although historically the diagnosis and treatment of ADHD have focused on children, more recently clinicians and researchers have explored the impact of ADHD on adults. Few, however, have focused on the effects of adult ADHD on relationships and marriages, which makes this a must-read for all of those interested in and working with adults with ADHD.
Sie lesen das E-Book in den Legimi-Apps auf:
Seitenzahl: 617
Veröffentlichungsjahr: 2014
Das E-Book (TTS) können Sie hören im Abo „Legimi Premium” in Legimi-Apps auf:
Ähnliche
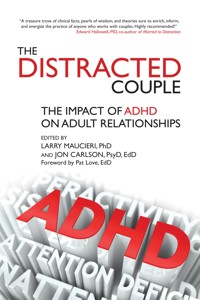
Advance Praise for The Distracted Couple
A treasure trove of clinical facts, pearls of wisdom, and theories sure to enrich, inform, and energize the practice of anyone who works with couples. Still vastly under-diagnosed, ADHD in adults can ruin a marriage and the lives involved in it. The rare therapist who can diagnose the adult ADHD can save that marriage and with it the lives it touches. A unique book, written by a wide range of gifted clinicians, The Distracted Couple is a gem, indispensable for all who work in the field. Highly recommended!
—Edward Hallowell, MD, co-author of Married to Distraction
Larry Maucieri and Jon Carlson have provided a vitally needed resource dealing with a crucial topic—a comprehensive guide to ADHD in couples. Chapters cogently describe such crucial topics as how to recognize ADHD, the role of executive functioning, ADHD in couples from diverse cultures, and ADHD in women, as well as how to work with ADHD in couple therapy. This book should be essential reading both for couple therapists and for those who work with those with attention deficit disorders.
—Jay Lebow, Ph.D., LMFT, ABPP, Clinical Professor, The Family Institute at Northwestern and Northwestern University
This book explores the fascinating crossroads between ADHD and romantic relationships. Whether you work with couples or are just curious about how ADHD symptoms play out in relationships, you’ll find Maucieri and Carlson’s edited volume both intellectually stimulating and highly practical. Most importantly, reading this book will give you greater empathic understanding of the struggles that ADHD symptoms can cause in couple relationships.
—John Sommers-Flanagan, Ph.D. Professor of Counselor Education, University of Montana, author of Clinical Interviewing and How to Listen so Parents Will Talk and Talk so Parents Will Listen
A refreshing and empathic look into how ADHD manifests itself into relationships. The editors take the “disorder” out of the distraction by providing messages of hope, as well as focusing on how couples can adapt and strengthen their relationships amidst overwhelming distractions. An invaluable resource for both clinicians and couples!
—Jill Duba Sauerheber, PhD, Associate Professor, Western Kentucky University; President-Elect, NASAP; author of The Role of Religion in Marriage and Family Therapy
The Distracted Couple is much more than a commentary on ADHD and couples. It is more a journey into our own potential signs of imperfection referred to as ADHD. This is not just a book on ADHD but is in so many ways cutting edge research on the topic and treatment strategies that could and can be used in a number of different settings including therapy, parenting, coaching, teaching, and for the reader’s personal growth. Congratulations to Drs. Maucieri and Carlson for carefully integrating science with application.
—Roy Kern EdD, Scientific Professor, Dept. of Theoretical Psychology, Vytatus Magnus University, Lithuania, Professor Emeritus, Dept. of Counseling and Psychological Services, Georgia State University, and Co-Editor of The Journal of Individual Psychology
Drs. Maucieri and Carlson have edited a volume that expands the understanding of ADHD. While other books have begun to discuss the relational issues confronting couples, this book covers every angle. The Distracted Couple starts with the DSM-5, and quickly moves into how adult ADHD is exhibited in treatment. Rather than concentrate only on the majority population, this volume clarifies the disorder with African-American couples and same sex couples. The specific issues that arise for women with ADHD are also beautifully connected to relational issues. Finally, this book rounds out its couple’s focus by directly discussing the effect of ADHD on financial management. Clearly, this book serves as a necessary reference for a comprehensive understanding of ADHD and its effect on the relationships.
—Scott Browning, PhD, Professor, Chestnut Hill College, Philadelphia, author of Stepfamily Therapy
As ADHD becomes increasingly common in adults and couples, clinicians of all stripes will need to increase their understanding of this condition to better treat or more appropriately refer for treatment. This is the “go to” book that I’ll highly recommend to my students and colleagues.
—Len Sperry, MD, PhD, Clinical Professor of Psychiatry, Medical College of Wisconsin, author of Handbook of Diagnosis & Treatment of DSM-5 Personality Disorders
A first-class treasury of articles for everyone interested in ADHD and couples counseling.
—William Knaus, EdD, author of the Cognitive-Behavioral Handbook for Depression; The Cognitive-Behavioral Handbook for Anxiety; and Do It Now.
Drs. Maucieri and Carlson provide much-needed guidance for professionals who work with ADHD individuals and couples. They have recruited an impressive group of experts, with an emphasis on effective intervention with couples, the unique focus of this book. They present sophisticated views on diagnosis and brain functioning, including current controversies, in a straightforward style that can be understood even without training in neuropsychology. The book is also unique in discussing populations impacted by ADHD but underserved, including African American couples, same sex couples, and women with ADHD. Hopefully this volume will enable clinicians to help combat the blame and self-blame that permeates the lives of those with ADHD, enabling couples to work together to cope with the many challenges and frustrations involved, and dispelling the myths about adult ADHD that have left the majority of individuals undiagnosed.
—Thomas Todd, PhD, Chicago Center for Family Health, AAMFT Approved Supervisor
The Distracted Couple
The Impact of ADHD on Adult Relationships
Edited by
Larry Maucieri, PhD & Jon Carlson, PsyD, EdD
Dedication
We dedicate this book to all those couples that are finding and maintaining love with the challenge of distraction.
“Attention Deficit Disorder is not a disease, and people who have it are in no way ‘sick.’ It is a difference—a big difference—in the way the brain handles information. While most people think in a one-thing-at-a-time way, the ADD person takes in everything at once. Sometimes they overlook the trees because they see the forest. This can be frustrating for a non-ADD partner who doesn’t understand the ADD thought process. However, communication is one area where people with ADD shine; it is well worth learning a few special skills so that you and your ADD spouse can understand each other.”
—RICK FOWLER1
“There isn’t any formula or method. You learn to love by loving—by paying attention and doing what one thereby discovers has to be done.”
—ALDOUS HUXLEY
1. Fowler, R. (2002). Honey Are You Listening? Attention Deficit/Hyperactivity Disorder and Your Marriage. Gainesville, TX: Thomas Nelson.
Contents
Contributors
Stephanie Brooks, PhD, LCSW, LMFT
Chair, Couple and Family Therapy Department
Director Master of Family Therapy, Post-Master’s Certificate and Medical Family Therapy Programs
Drexel University
Philadelphia, Pennsylvania
Jon Carlson, PsyD, EdD, ABPP
Distinguished Professor of Psychology and Counseling
Governors State University
University Park, Illinois
Psychologist
The Wellness Clinic
Lake Geneva, Wisconsin
Gerald Gluck, PhD, LMFT, PA
BCN-Senior Fellow
Center for Family Counseling and Biofeedback
Coral Springs, Florida
Jennifer Koretsky, BA, SCAC
Founder of ADD Management Group, LLC
Wallkill, New York
Larry Maucieri, PhD
Assistant Professor of Psychology and Counseling
Governor State University
University Park, Illinois
Affiliate Clinical Neuropsychologist
The Family Institute at Northwestern University
Evanston, Illinois
Melissa Orlov, AB
ADHD Marriage Consultant
Melissa Orlov, LLC
Wayland, Massachusetts
Linda Roggli, BAS, PCC
Professional Certified Coach
Founder
ADDiva Network
Raleigh-Durham, North Carolina
Vice President
Attention Deficit Disorder Association (ADDA)
Stephanie Moulton Sarkis, PhD, NCC, LMHC
Private Practice
Boca Raton, Florida
Adjunct Assistant Professor
Florida Atlantic University
Sub-investigator of Clinical Trials
Schmidt College of Medicine
Florida Atlantic University
Fort Lauderdale, Florida
Susan Tschudi, MA, LMFT
Private Practice
Westlake Village, California
Adjunct Faculty
Graduate School of Education and Psychology
Pepperdine University
Malibu, California
Ari Tuckman, PsyD, MBA
Private Practice
West Chester, Pennsylvania
Roberta Waite, EdD, APRN, CNS-BC, FAAN
Associate Professor of Nursing
Assistant Dean of Faculty Integration and Evaluation of Community Programs
The Josiah Macy Jr. Foundation, Macy Faculty Scholar
Drexel University, College of Nursing and Health Professions
Philadelphia, Pennsylvania
Foreword
The destructive nature of ADHD was made real to me years ago when a client shared his story:
I can tell you the day, the hour, the minute our marriage died. My wife had requested I take a walk with her so that she could try once again to get my attention and keep me focused on her concerns. As we set out walking I was doing my best to listen and be present while she poured out her heart. After a few minutes passed, feeling comforted by my attention she reached for my hand; but just as her fingers touched mine I spotted the “It’s a boy!” sign in our neighbor’s yard. With my wife’s heart bleeding and longing for connection I blurted, “Look, Jen and Jason had their baby!”
I’ve played that fatal moment over and over like a driver who looked away just before a disastrous crash. That was the end of our marriage. She had tried for years to hold my attention and get me to understand but her heart was irrevocably broken—and so was our marriage.
Over three decades of clinical practice I have heard a version of this story many times, and it makes sense. Attention is the fuel that powers relationships. When there is no intimate focus, no close connection, the relationship ceases to function.
It’s interesting that our pets often understand attunement and focus better than we do. Another client told me this story that illustrates a vital lesson:
We were having the same conflict we’d had hundreds of times. Roger was trying to get my attention but I was totally distracted. All of a sudden I was shocked into awareness by his uncontrollable sobs. He was just crying and crying and I just froze. Because I hadn’t been paying attention I didn’t know what to say or where to turn. I tried uttering words of comfort but I was so out of touch it just intensified his pain.
Then I got an object lesson that likely saved the relationship.
Hearing Roger’s cries, our beloved yellow lab, Buddy moved to his side, put his head on his knee and looked up at him with rapt attention. This simple act calmed Roger and averted a crisis.
In that moment, I got it.
At first I was humiliated that our dog knew more than I did but fortunately, I took a lesson instead of taking offense. I followed Buddy’s example and went over to Roger, sat beside him and focused my attention. I didn’t have to say anything; just being truly present was all he wanted.
The number-one cause of divorce cited by couples is “growing apart.” The number-one cause of growing apart is withdrawing your attention. When you no longer see, hear or feel your partner in a way that creates connection and that magical limbic resonance, the relationship withers away.
The couple cascades into crisis when attention is continually focused on activities outside the relationship or on experiences that do not reinforce the relational bond. Whether stimulation comes from the environment or inside the person’s head, lack of focus or lack of attunement can destroy the most robust relationship.
Any clinician working with couples has no doubt observed how difficult relationships are to maintain today, and that a big part of the strain comes from the multitude of temptations vying for our attention. ADHD is not only an individual and relationship issue, it’s a way of life.
I applaud Drs. Maucieri and Carlson for creating this most valuable book at a vital time. It will serve as a valuable resource for all of us behind the therapy door, counselors and clients alike!
Pat Love, EdD Austin, TX
Acknowledgements
We would like to thank our colleagues in the Division of Psychology and Counseling at Governors State University for their continued encouragement and support.
We thank Chelsea Devlin and Rachel Ursitti at Crown House Publishing for their editing assistance and help. We are especially appreciative of the support and belief in this project of our editor, Mark Tracten. Mark made many helpful suggestions that have been directly incorporated throughout this publication. He is truly an editor’s editor!
Larry wants to thank his parents, Rose and Larry, for their unwavering guidance, love and support, Lindy for her constant companionship, and Jiyong for all of the joy of life he has brought to the world.
Jon wants to thank the friends and family who have been so supportive during his two years of medical challenge. A special thanks is given to his wife, Laura, who has had to deal with a distracted partner for at least the past two of their forty-six years together.
Introduction
Larry Maucieri, PhD Jon Carlson, PsyD, EdD
We seem to have moved into what experts have referred to as an “attention deficit culture.” The technological revolution has brought about massive changes in lifestyle over a short period of time. The amount of anxiety, distraction, and stress are so prevalent in society that they seem to impact every relationship, increasing the reliance on devices such as phones and computers for connection. Many researchers have suggested that the more connected we are electronically, the more disconnected we are personally. Over-reliance on texts, tweets, and emails seems to draw couples apart.
The chapters in this book go beyond “normal disconnection.” They focus on how adult relationships are impacted when one or both partners have been diagnosed with ADHD or attention deficit hyperactivity disorder. This diagnosis that has received a lot of attention when applied to children and teenagers; however, it has only recently been accepted that this disorder carries over into adulthood for many people and becomes magnified in intimate relationships.
This is an exciting time for clinicians working with adults and, specifically, couples impacted by attention deficit hyperactivity disorder (ADHD). After years of ADHD being understood as largely a disorder of childhood, we have come to understand that many of the difficulties and challenges of this disorder remain present in adulthood. As we begin to greater appreciate the impact of ADHD in the adult lifespan, it becomes evident that some of the tasks inherent to that phase of life are undoubtedly impacted as well. We are speaking predominately of work and love. The nature of work, which often involves internal organization, structured social etiquette, and multi-tasking, is at odds with the symptoms of adult ADHD. With love and relationships, the effects of ADHD can be equally tumultuous and challenging, even if the nature of the disorder is not as clearly evident.
There are many puzzling behavioral components or symptoms necessary for someone to meet a diagnosis of adult ADHD that undoubtedly create problems for intimate or couple relationships. Some of the symptoms highlighted by Hallowell and Hallowell (2010) include: unexplained underachievement; easy distractibility coupled with an ability to hyperfocus; trouble with time management; a tendency to be impulsive; seeks out high stimulation; tends to be impatient; tends to be stubborn; problems with organization, planning, and prioritizing; a tendency to self medicate with alcohol or drugs; mood instability; and the tendency to worry needlessly. The task at hand is to help our clients to avoid distractions and mental traps, manage their emotions, and organize their thinking in order to develop and maintain satisfying relationships.
There has been progress in recent decades in terms of managing ADHD in the workplace and with home life. In addition to medication, individual life coaching and cognitive-behavioral therapy (CBT) models (e.g., Safren, Perlman, Sprich, & Otto, 2005) have been employed for a range of behavioral issues commonly affected by adult ADHD at home and in the workplace. What has been less successfully addressed until now is the exploration and management of ADHD symptoms in close adult relationships.
In the past few years, popular press books by Melissa Orlov (2010), Gina Pera (2008), and others have started to tackle the effects of ADHD on adult relationships and couples. This book is an extension of their groundbreaking work. It aims to extend this area of work by providing a range of models, theories, and interventions geared largely toward those individuals who work professionally with clients impacted by ADHD in their adult relationships. This book is focused on the experiences and tools of helping professionals, such as counselors, psychologists, therapists, psychiatrists, physicians, nurses, coaches, and social workers. That said, there is also plenty to relate to in here on a personal level, such that individuals whose lives have been directly affected by adult ADHD in their relationships will also find it to be a helpful resource.
A number of exciting contributions and state-of-the art ideas are presented in this book. Melissa Orlov contributes two chapters (Chapters 2 and 8) that help readers recognize ADHD within relationships, and offers a detailed, three-stage recovery map to address these struggles within the relationship. Ari Tuckman presents a comprehensive and detailed description of the effects of ADHD on executive functions, including how these problems result in relationship concerns, and what to do about them (Chapters 3 and 9). Susan Tschudi devotes an entire chapter to the experience of the partner within a relationship who does not have ADHD, but who is nonetheless impacted by his/her partner’s ADHD (Chapter 10). This is an area that is not often explored or even mentioned in books on adult ADHD, and so it is thrilling to have a clinical expert help us understand and address the struggles relating to this largely unrecognized aspect of adult relationships affected by ADHD. Stephanie Sarkis describes the difficult financial situations that ADHD can cause in adult relationships, and the methods that help mitigate these challenges (Chapter 12).
While controversial among some mental health workers, the recently-released DSM-5 has been updated and modified to reflect changes in conceptualization about ADHD in the later adolescent and adult lifespan (APA, 2013). Although some changes to the definition and criteria were made, they were not as drastic overall as originally expected. In Chapter 1 of this book, Larry Maucieri provides a detailed summary of the most recent work and the science related to adult ADHD, involving the underpinnings and ultimate changes adapted from the DSM-IV-TR to the DSM-5 involving ADHD diagnostic criteria.
As our understanding of the influence of ADHD on adult relationships expands, largely neglected areas of concern become more evident. Gerald Gluck (Chapter 11) describes the application of neurofeedback and electroencephalography (EEG) as part of a treatment regimen for adults in relationships impacted by ADHD. While ADHD has traditionally been regarded as a disorder of boys, it impacts both genders more equally in adulthood. Linda Roggli (Chapter 6) offers an examination of the effects of ADHD on women, another area that has received little notice up until this time. In Chapters 4 and 5, Roberta Waite and Stephanie Brooks deliver a helpful description of the combined factors that influence African-American couples impacted by ADHD, and ways to work with these challenges. Finally, Jennifer Koretsky (Chapter 7) provides insight into the effects of ADHD on same-sex adult relationships, which happens now to strikingly coincide with the increased recognition and institutionalization of same-sex marriage in our country.
The sometimes daunting, often intractable nature of adult ADHD is so difficult to address without much guidance or a deep level of professional experience. With this book, clinicians who work with adult clients directly or indirectly impacted by ADHD in their close relationships now have an exciting volume to read and reference in terms of better understanding and working more effectively with their clients on these concerns! Further, this book helps to encapsulate the most recent knowledge and theory about adult ADHD and couples dynamics to help those involved with this work. The symptoms of ADHD, as they affect couples and relationships, can be addressed directly and efficiently, and, in this volume, a plethora of clinical and research wisdom, current science and practice, and astute intervention methods are available for professionals working in this as-yet largely uncharted territory.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Press.
Hallowell, E. M., & Hallowell, S. G. (2010). Married to distraction: Restoring intimacy and strengthening your marriage in an age of interruption. New York, NY: Ballantine Books.
Orlov, M. (2010). The ADHD effect on marriage: Understand and rebuild your relationship in six steps. North Branch, MN: Specialty Press.
Pera, G. (2008). Is it you, me, or adult ADD? Stopping the roller coaster when someone you love has attention deficit disorder. San Francisco, CA: 1201 Alarm Press.
Safren, S. A., Perlman, C. A., Sprich, S., & Otto, M. W. (2005). Mastering your adult ADHD: A cognitive-behavioral treatment program. New York, NY: Oxford.
Part I
Effects of ADHD on Couples
Chapter One
ADD, ADHD, & Adults: Sorting It All Out
Larry Maucieri, PhD
ADD, ADHD and Adults: Sorting it All Out
The evolving science and practice exploring attention deficit hyperactivity disorder (ADHD) have yielded a number of interesting and exciting findings that directly impact our understanding and knowledge of the disorder. In recent decades, the notion of ADHD as strictly a disorder of childhood has been challenged, such that it is now also reliably identified and treated in adults (Safren, Perlman, Sprich, & Otto, 2005). The focus of this book is on the impact of adult lifespan ADHD on interpersonal relationships, specifically marriages and romantic partnerships. Before addressing the patterns, challenges, and range of interventions for couples impacted by adult ADHD, however, it is helpful to summarize the most recent literature involving adult ADHD. This summary of the current science and practice is intended to provide readers with a brief but solid foundation on which to understand the phenomenon of adult ADHD. It should provide the reader with a helpful context within which the interventions that follow may be practiced and understood. As we in mental health care transition from using the DSM-IV-TR to DSM-5, part of this chapter will focus on the evolution of ADHD as a diagnostic entity in these diagnostic manuals.
To provide readers with a solid background, recent work involving a number of aspects of ADHD is presented here. This includes the evolving diagnosis and conceptualization of ADHD; the DSM‑IV-TR and expected DSM-5 criteria for the disorder (American Psychiatric Association, 2000; 2013); the prevalence of adult ADHD; the biological bases of the disorder; issues and concerns that frequently occur with adult ADHD; and contemporary treatment approaches for the disorder. We mention some of the earliest theories involving what has come to be known as ADHD, before focusing for the remainder of the chapter on the most recent work and concepts related to the disorder.
The Evolving Diagnosis of ADHD
While not always recognized by its current name, the syndrome that is attention deficit hyperactivity disorder (ADHD) has been written about, debated, and discussed for at least 100 years. Consistent with the science of the times, in the early 1900s it was characterized as resulting from “a lack of moral control and the failure of the individual to conform to the environmental expectations for behavior” (Wadsworth & Harper, 2007, p. 101). The disorder was later conceptualized as other diagnostic entities such as hyperkinesis disorder of childhood and minimal brain dysfunction before it gradually evolved into the syndrome recognized today as ADHD (Wadsworth & Harper, 2007).
Similar to the medical and biological bases empirically discovered for other psychiatric disorders (e.g., schizophrenia, bipolar disorder), in recent decades, ADHD has also been conceptualized as having a significant neurobiological component. Some of the most recent work in this area is detailed below. As Waite and Brooks (2013) note in this text, however, ADHD is not a purely biological disorder and socio-cultural factors are quite germane in the development and symptom manifestation of ADHD in children, adolescents, and adults. We begin with a cutting-edge theory from eminent ADHD expert Russell Barkley who posits a concept relating to and possibly explaining some of the characteristics of ADHD.
Sluggish Cognitive Tempo
Independent of the DSM-related criteria developed for ADHD which are explored below (APA, 2000), a number of other recent theories and concepts related to the disorder have emerged in the last few years, and it may be beneficial for clinicians and providers to have some knowledge of them. Barkley (2012), for instance, recently described a correlate of ADHD called sluggish cognitive tempo (SCT). Individuals with SCT are described as exhibiting reduced activity, a tendency to daydream, confusion, and lethargy. These symptoms might occur not only in the context of ADHD, but in other well-established disorders (e.g., depression). Barkley (2012) argues, though, that among those who meet criteria for ADHD, a subset of them distinctly exhibit SCT. It should be noted that within his model SCT may also occur in individuals who do not meet the diagnostic criteria of ADHD, such that SCT and ADHD may be related, but they are separable entities. Barkley (2012) suggests that the concept of SCT is distinct from ADHD as supported by factor analyses of parent and teacher ratings of children, and that SCT is associated with executive impairments and psychosocial deficits in adult participants beyond what could be explained by ADHD alone.
While this investigation might imply some overlap between SCT and (in DSM-IV-TR conceptualization consistent with the time of his publication) the predominantly inattentive type of ADHD, the combined type of ADHD, and to a lesser extent the hyperactive-impulsive type of ADHD, Barkley (2012) does not suggest that SCT is redundant with and fully captured by the inattentive aspects of ADHD. Rather, he argues that there is a high degree of overlap between SCT and ADHD. In this regard, some diagnoses that have been made as ADHD predominately inattentive type might actually reflect a case of high SCT along with other elements of ADHD present, rather than an actual case of ADHD itself. Finally, Barkley (2012) stated that SCT might be considered a distinct diagnosis in the forthcoming DSM-5, although this was not the case in the final formulation of the DSM-5 (APA, 2013). Still, the introduction of SCT within the conceptualization of ADHD may indicate a transition toward a more spectrum-oriented conceptualization of ADHD.
Revisiting Criteria for ADHD: Recent Developments
Before considering the evolving DSM criteria for ADHD below, it is interesting to note some of the recent work on what ADHD entails, and how well this has or has not been captured within the DSM criteria that are so often used to define ADHD. Barkley (2012), for instance, reports that some authors wonder if the DSM-IV-TR types of ADHD (defined below) might represent not so much distinct subtypes of the disorder as variable levels of severity on an ADHD spectrum.
A fair number of critics note that the DSM-IV and DSM-IV-TR criteria for ADHD are heavily skewed toward the experiences and behaviors of children (Weisler & Goodman, 2008). This might naturally reflect that the disorder was long considered an exclusive syndrome of childhood and adolescence. However, there is increased awareness that for many individuals, at least some of the symptoms of ADHD endure into adulthood. Some of these symptoms may even evolve in presentation. For example, one study suggested that a validated computerized measure of sustained attention often used to help diagnose ADHD may be optimally administered for this purpose with children in morning hours, but would be valid during both morning and afternoon times for young adults (Hunt, Bienstock, & Qiang, 2012). An important area of interest for clinicians is the mounting evidence in support of ADHD symptoms persisting into adulthood and the need to better understand its presentation so that it may be effectively remediated.
Executive Impairments and ADHD
As the name suggests, attentional deficits are a core feature of ADHD. However, recent empirical work has also strongly implicated executive impairments as well. For instance, a recent study by Boonstra, Kooij, Oosterlaan, Sergeant, and Buitelaar (2010) comparing adults with ADHD matched with controls on age and gender found that the executive functions of inhibition and set shifting were particular areas of deficit for adults with ADHD. As of yet, these difficulties have not been well codified in the DSM criteria or conceptualization of ADHD, but it had been hoped that the criteria in the DSM-5 may do so. In reality, the DSM-5 did not drastically alter the criteria from the DSM-IV-TR, such that an executive impairment became a core diagnostic feature of the disorder (APA 2000, 2013). This change would have been helpful and important as clinicians working with ADHD need to be fully aware of all related issues and problems that reliably occur as part of the disorder. A detailed exploration of executive impairments in adult ADHD is nonetheless provided within this text by Tuckman (2013).
Executive impairment as a central feature of ADHD is supported by other recent work. Fedele, Hartung, Canu, and Wilkowski (2010) concluded in their work that two core factors of ADHD involve cognitive flexibility and disinhibition. While these features are well-established in the clinical and research literature on ADHD, they were not clearly reflected in the core criteria of the DSM-IV-TR for ADHD.
Tuckman (2013) argues that executive impairments are a hallmark of ADHD that persist from childhood into adulthood. In support of this idea, Miller, Ho, and Hinshaw (2012) found that executive dysfunction continued into young adulthood among females who had been diagnosed with ADHD in childhood, even in those individuals whose other ADHD symptoms remitted. Clearly, then, a greater awareness of executive impairment as part of adult ADHD is needed.
As we have already seen, while the DSM criteria are not perfect in their characterization of the ADHD experience, they are used pervasively and are quite influential in the clinical understanding of this disorder. A review of the established DSM-IV-TR criteria for ADHD is helpful in this regard, with a particular emphasis on how these criteria have evolved in the DSM-5, and how closely aligned these documents are to some of the more current developments in ADHD research and clinical work.
ADHD: DSM Conceptualizations
An exploration of the ADHD symptom criteria in recent decades and the recent changes in the criteria are highly useful. These standards in mental health care are presented and deconstructed for a deeper understanding of their strengths and limitations. We focus here on the DSM criteria as these are the most widely used in the USA. While these criteria apply to all individuals who might meet a diagnosis of ADHD, the literature demonstrates that these criteria are not an equally good fit for all ethnic and gender groups (Waite & Brooks, 2013). From a broader sociocultural perspective, ADHD conceptualization, diagnosis, and treatment plans may be specifically suited for Caucasian males, resulting in suboptimal recognition and treatment of the disorder in women and individuals from diverse backgrounds (Waite & Ivey, 2009).
An Assessment of ADHD in the DSM-IV-TR
Although the DSM criteria changed slightly in May of 2013, it is worthwhile to briefly review the DSM-IV-TR criteria for ADHD that had been used since 2000. Doing so will allow a better understanding of how the disorder has been understood and conceptualized in recent years, and how it might differ from the extant contemporary literature involving ADHD. Furthermore, this knowledge provides a solid foundation for understanding and critiquing the new DSM-5 criteria for this disorder released in May 2013.
The DSM-IV-TR configuration of ADHD involved two broad dimensions of the syndrome: inattention and hyperactivity-impulsivity (APA, 2000). Note that in the latter grouping both hyperactivity and impulsivity were represented in one set of symptoms, rather than as separate areas of concern. To formally meet this diagnosis per DSM-IV-TR specifications, one would have needed to manifest a minimum of six of the criterion symptoms in one or both of these broad categories. This would have then yielded three possible types of ADHD by DSM-IV-TR criteria: 1) the predominately inattentive type, 2) the predominately hyperactive-impulsive type, or 3) the combined type (APA, 2000; Safren et al., 2005). The combined type of ADHD meant that criteria had been met for not only inattention, but also for the hyperactive and impulsive cluster of symptoms.
Contrary to popular belief, the DSM-IV-TR and DSM-5 criteria do not include what has been referred to as “ADD,” or “attention deficit disorder.” That concept had been included in prior versions of the DSM and is meant to describe a variant of the disorder in which there are disproportionate issues with attention in the presence of less severe problems involving hyperactivity and impulsivity. The former concept of ADD would most closely equate to the DSM-IV-TR diagnosis of the predominately inattentive type of ADHD and the DSM-5 diagnosis of ADHD, predominantly inattentive presentation.
In addition to the symptom profiles described above, these diagnostic signs of ADHD must have been present in at least two different settings, have caused a significant impairment, and at least some of them must have occurred by age 7 in the DSM-IV-TR (APA, 2000; Coghill & Seth, 2011). The justification for these stipulations were to assist clinicians in ruling out situation-related stress reactions, instances of idiosyncratic characteristics that are not causing problems or impairments for the individual or others around him/her, and to better rule out other causes for the symptoms which might be related for instance to mood or acquired causes (e.g., traumatic brain injury), rather than being of developmental origin, as ADHD was presumed to be (APA, 2000).
Criticism of the DSM-IV-TR
Criticism of the symptom criteria for ADHD in the DSM-IV-TR had been mixed and directed toward a number of different concerns. First, some experts questioned if the three types of ADHD accurately reflected the disorder itself. Barkley (2012), for instance, reported that some authors suggested that the hyperactive-impulsive type of ADHD might have actually represented a milder or prodromal stage of the combined type of ADHD, rather than a separate type of the disorder.
Second, symptom frequency was somewhat subjective in these criteria, in that they consistently used the term “often” to denote frequency, but provided no behavioral anchors for what this meant (APA, 2000). For instance, a hyperactive-impulsive criterion for ADHD, “Often talks excessively,” relied almost exclusively on the interpretation of the reporter for how frequently the behavior occurs and if it should be considered “often” or not. This was an issue to some extent for all 18 of the DSM-IV-TR criteria of ADHD.
Third, others have noted that the DSM-IV-TR criteria overwhelmingly reflected the origins of the disorder conceptually as having been limited to childhood, and thereby under-representing symptoms of ADHD that might endure and continue to be problematic into adulthood (Coghill & Seth, 2011). Possible examples of ADHD criteria that illustrate this concern might include items such as, “Often fidgets with hands or feet or squirms in seat,” and, “Often has difficulty sustaining attention in tasks or play activities” (APA, 2000; Safren et al., 2005).
At a more macroscopic level, some authors opined that the DSM-IV-TR criteria for ADHD were too restrictive for adults, such that only five of the nine criteria (rather than six, as was the case for the DSM-IV-TR) for both the hyperactive-impulsive and inattentive aspects should be used as cutoffs to identify ADHD in adults. This argument is nested in the theory that fewer symptoms in adulthood may lead to more observable deficits (Boonstra et al., 2010). By strict application of the DSM-IV-TR criteria, an adult having only five symptoms in one or both categories could not have been diagnosed with ADHD, but still might have qualified for a variant diagnosis relating to the disorder, such as perhaps a diagnosis of ADHD, not otherwise specified (APA, 2000).
Overdiagnosis by Mental Health Care Providers
Conversely, Bruchmüller, Margraf, and Schneider (2012) suggest that ADHD might be over-diagnosed because, despite the strengths and limitations of the DSM-IV-TR and ICD-10 criteria for the disorder, mental health care providers may rarely follow the criteria as they were intended to be used. Rather, a more impressionistic or partial application of these symptom criteria may be used in making a diagnosis, leading to lower inter-rater levels of agreement. Using vignettes of children meeting full or partial criteria for ADHD, as well as other diagnoses (e.g., Generalized Anxiety Disorder), this group demonstrated that on average, 16.7 percent of participant therapists in Germany made diagnoses of ADHD when there were not full criteria met for that diagnosis. Interestingly, they were even more likely to make a diagnosis of ADHD in situations where full criteria were not met when the client was identified as being a male child. In this particular study, the gender of the therapist was a significant factor in the disparity of ADHD diagnoses, such that male therapists were more likely to make a diagnosis of ADHD across vignettes than female therapists were (Bruchmüller et al., 2012).
While incorrect diagnoses are themselves problematic, Bruchmüller et al. (2012) further noted that these lead to potentially inaccurate or unwarranted interventions. Recommendations and treatment plans involving medication, for instance, were more likely to be mentioned for the children in the vignette who did not meet full criteria for ADHD but who were judged to have had ADHD by the therapists involved in the study (Bruchmüller et al., 2012).
As mentioned previously, the DSM-IV-TR criteria for diagnosing ADHD required not only that six of nine symptoms in one or both categories are met, but also that the symptoms occurred across multiple settings, and that at least some of them must have first manifested in childhood. The latter stipulation was an attempt to rule out the possibility of ADHD first occurring in adolescence or adulthood. DSM-IV-TR criteria proscribed a cutoff age of six or seven years for at least some of the symptoms being noticed and present in the individual (APA, 2000). Not all six symptoms in a category needed to be present by age six or seven (APA, 2000). While this might have represented a laudable effort to use an age cut-off to help establish ADHD as a primarily neurodevelopmental disorder, issues involving unreliable memory, biased symptom endorsement, and even demand characteristics may have all undermined this method as a reliable and valid indicator of ADHD as a nascent issue in early development (Barkley, Knouse, & Murphy, 2011).
In fact, establishing both early and recent symptoms and histories in the formal diagnosis of ADHD can be quite challenging and rather subjective. The use of collateral information from significant others, parents, and teachers has become a common practice in an attempt to minimize some of these concerns. In their evaluation of a collateral method to attempt to minimize rater bias and inaccuracy, Barkley et al. (2011) reported moderate to strong positive levels of symptom endorsement agreement (range between 0.59-0.80) in recent adult functioning and retrospective child functioning between participants and collateral sources on symptoms of ADHD.
In addition to collateral content to specify symptoms endorsed in the assessment of possible ADHD, other clinicians rely on available external documents (e.g., report cards from childhood, prior evaluation reports, home visit records) to provide external supportive evidence particularly in childhood to help establish the severity and timing of possible ADHD symptoms. While a review of the DSM-IV-TR criteria is useful and helpful for readers, perhaps of greater interest is an examination of the newly-released DSM-5criteria that will be in use in the present and future.
ADHD in the DSM-5
Like many changes made in consecutive versions of the DSM, the criteria for ADHD reflect an attempt to address some of the concerns and criticisms raised by the previous version of the manual’s criteria. Additionally, the changes often attempt to mirror, at least to some extent, the newer information and current science on the disorder itself from the scholarly literature. The development for this particular version of the DSM (the DSM-5) has been met with numerous questions regarding reliability of diagnoses and the empirical foundations for some of the changes being proposed (Coghill & Seth, 2011). Just weeks before its scheduled release, for instance, a director from the National Institutes of Mental Health (NIMH) announced that the agency would be distancing itself from the use of DSM-5 diagnostic categories in favor of as-yet undefined researchbased criteria involving genetic, cognitive, and medical data in its funding of research projects (Horgan, 2013). Seemingly a significant blow to the DSM-5, the longer-term ramifications of this decision for care providers and for the manual itself have yet to be determined.
The proposed changes to the definition of ADHD in the DSM-5 were expected to include a reference to the disorder having both cognitive and behavioral functional elements, an indication that symptoms may present differently in different environments or situations, and allowance for comorbidity with an autistic-spectrum disorder (Coghill & Seth, 2011). The DSM-5 proposed criteria for ADHD were also presumed to exclude mood changes lasting greater than four days, and explicitly suggest input and collateral information from parents and teachers for children and from knowledgeable third parties for older adolescents and adults (Coghill & Seth, 2011). Among the more substantial changes to the ADHD criteria, the DSM-5 symptom onset was expected to be adjusted upward from age seven to twelve. This might reflect a greater level of flexibility in terms of recognizing the onset of the disorder, while still maintaining the recognition of ADHD as a neurodevelopmental disorder beginning in childhood. Probably in reflection to the greater appreciation and awareness of executive impairments as a core feature of ADHD, the DSM-5 was expected to include four additional symptoms of impulsivity to more fully represent this element of the ADHD experience (Coghill & Seth, 2011).
In reality the DSM-5 made fewer adjustments to the ADHD criteria than were predicted. The three subtypes of the disorder were kept intact with slightly modified labels of: Combined presentation, Predominantly Inattentive presentation, and Predominantly Hyperactive/Impulsive presentation (APA, 2013). As expected the age of symptom onset was increased from six or seven years to twelve years, but the number of symptoms required to meet criteria in each category in the past six months for individuals ages seventeen and older was changed to five rather than four as expected (APA, 2013).
A few additional codes have been added in the DSM-5 which were not discussed much in the proposed changes involving severity and remission. The severity level is based on the number of ADHD symptoms met, using a mild-moderate-severe spectrum. Moreover, the DSM-5 criteria now allow for an indication of “in partial remission” for individuals who previously met full criteria for ADHD, have not met full criteria in the past six months, but still experience impairment in social, occupational, and/or academic functioning (APA, 2013).
Finally, the authors of the DSM-5 ultimately decided to made few significant changes to the individual criteria for each of the ADHD categories, and did not include the newly-proposed criteria involving executive impairments (APA, 2013). Their reasons for not including these new criteria are not known, but perhaps they felt that it would expand the conceptualization of ADHD too broadly. Empirical evidence for the inclusion of these newly proposed criteria was mixed in one recent study.
To assess the inclusion of these newly proposed symptoms and the ADHD subtypes suggested for the DSM-5 relative to the DSM-IV-TR, Ghanizadeh (2012) completed a confirmatory factor analysis using the four new impulsivity criteria mentioned above along with the DSM-IV criteria for ADHD. The author found that all of these symptoms fit within a two-factor configuration of ADHD involving inattention and hyperactivity-impulsivity, but that a better fitting model actually involved a three factor solution. In the latter empirically-derived conceptualization of ADHD, Ghanizadeh’s (2012) three factors of ADHD would include inattention, hyperactivity-impulsivity, and then a third factor of the four new impulsivity items themselves. This finding does not necessarily support the new items being easily subsumed or synthesized into the previous DSM-IV/DSM-IV-TR definition of ADHD, although the study may have limited generalizability for such broad implications. The author’s data were collected from 106 children in Iran. The generalizability of this sample to USA populations is not completely clear, and the sample size is a bit small for a methodologically complex statistical model such as factor analysis. Ultimately, they were not adopted for use in the DSM-5 and so the individual criteria more closely resemble those of the DSM-IV-TR than had been expected.
Changes to Symptom Requirements in the DSM-5
Perhaps the most significant and controversial change in the ADHD criteria in the DSM-5 involves the number of endorsed symptoms required to attain a diagnosis in the disorder. In the DSM-5 criteria for ADHD, the two factor symptom breakdown (inattention and hyperactivity-impulsivity) has been retained. Children require six or more symptoms of inattention and/or six or more symptoms of hyperactivity and impulsivity to meet the criteria for ADHD (APA, 2013; Kooij et al., 2010). This is unchanged from the symptom endorsement level in the DSM-IV-TR (APA, 2000). However, in the proposed DSM-5 criteria, adolescents and adults older than age seventeen would have only required four symptoms in either or both of these categories to meet the proposed new symptoms for ADHD. Along with other changes, this has been among the most heavily criticized features considered for the revision of the manual. In the final version of the DSM-5 the number of symptoms required for adults and older adolescents was reduced from six in each category, but it was set at five rather four as predicted (APA, 2013). This might have been done to balance the need to recognize a less severe overall presentation in adults compared to children with concerns among mental health professionals about overdiagnosis. Even with this change, the criteria remain categorical in nature, despite the suggestion of some authors (e.g., Das et al., 2012) that a more dimensional or spectrum-based conceptualization of ADHD might be preferable.
In support of this alteration, Kooij et al. (2010) argue that the reduction in DSM-5 criteria for adult lifespan ADHD symptoms is appropriate, because it reflects the natural course of the disorder as a function of age. This is based on the notion that ADHD symptoms are more pronounced and obvious in children, and then become more subtle as these individuals become adults. That being said, even with fewer symptoms to meet the full criteria for ADHD, the proposed DSM-5 definition of the disorder would still require an impaired level of functioning for the individual in his/her adult lifespan. To the degree that diagnosing clinicians strictly follow all of these criteria, it is assumed that the identification of ADHD in adults would still represent an accurate and valid diagnosis, leading to appropriate and helpful treatment.
From this author’s perspective however, it is not totally evident how the criteria for ADHD in the DSM-5 completely safeguard a clinician from confusing the signs of inattention and impulsivity due to other causes (e.g., toxic exposure, traumatic brain injury, thyroid dysfunction, anxiety, depression) as being misinterpreted as ADHD. While the DSM-IV-TR and DSM-5 both include language in this and other disorders forbidding the diagnosis of a syndrome when symptoms appear to be caused by another issue, both anecdotal and empirical evidence suggest that these precautions may not be consistently followed or noticed by a number of diagnosing clinicians (e.g., Bruchmüller et al., 2012). Moreover, some diagnosing clinicians may not be aware of the dozens of other medical and psychiatric disorders that can cause inattention, reduced processing speed, impulsivity, and/or hyperactivity. Therefore, ADHD might be diagnosed because the other differential diagnoses are not known and therefore not salient in the individual’s clinical conceptualization.
In addition to the distinction between inattentive and hyperactiveimpulsive symptom constellations, the proposed criteria for ADHD had indicated a possible subtype called inattentive presentation (restrictive) for individuals who met the inattentive criteria for ADHD and who had two or less hyperactive-impulsive symptoms of ADHD (Coghill & Seth, 2011). This would have essentially been a subtype of the inattentive ADHD in which hyperactivity and impulsivity played a minimal role. Like some of the other proposed changes in the DSM-5, however (including not only ADHD but other psychiatric disorders), there did not appear to be strong empirical evidence to support or justify this proposed change and it was ultimately not adopted into the DSM-5 (APA, 2013; Coghill & Seth, 2011).
Thus, a number of proposed changes had been considered, and some of them accepted, in the clinical conceptualization of ADHD in the DSM-5. Future clinical and research work will help us to assess how beneficial these adjustments will be in our recognition and treatment of ADHD in adults, and specifically here how much they will assist us in the work we do with couples impacted by the effects of adult ADHD.
Prevalence of Adult ADHD
A recent area of increasing interest involves the prevalence of ADHD in adults. Looking back to the DSM-5 discussion, some critics have voiced concern that the lowered symptom threshold to achieve a diagnosis of ADHD in older adolescents and adults might artificially increase the reported prevalence rate of this disorder. To date the frequency and prevalence of adult ADHD is based on the previous (e.g., DSM-IV or DSM-IV-TR) conceptualizations of the disorder.
An increased awareness of ADHD has obviously contributed to its identification and treatment in adults in recent decades (Meyer, 2009). Until relatively recently the disorder was generally regarded as exclusively a childhood and adolescent phenomenon (Weisler & Goodman, 2008). This notion has been challenged in recent decades not with the conceptualization of a new onset of ADHD occurring in the adult lifespan, but with the understanding that residual symptoms of ADHD might persist into adulthood for a number of children and adolescents who had the disorder. One recent source estimates that about 8 million American adults probably qualify for a diagnosis of ADHD (Adler et al., 2010).
Perhaps because of the presumed more subtle nature of ADHD in adults relative to children, the recognition and treatment of ADHD in adults lags behind that of children. Weisler and Goodman (2008) cited data that only 10.9 percent of adults with ADHD may be treated in any format for the disorder. Some adults with ADHD may only begin to recognize that they might have ADHD after their own children are assessed and/or diagnosed with the disorder (Waite & Ramsay, 2010). This is particularly likely for higher functioning individuals who do not exhibit problematic enough symptoms to warrant notice in school or work settings. Such individuals may have also developed their own compensatory techniques by early adulthood that may conversely act to mask the nature of their struggles. Attempting to effectively parent with unrecognized ADHD is a daunting task; moreover, it is often compounded by one’s child also having the disorder because of the genetic bases of ADHD. Finally, the phenomenon of adult ADHD has not been well studied or understood in parents with unrecognized ADHD from diverse backgrounds (Waite & Ramsay, 2010). The particular challenges involving the identification and treatment of ADHD in African-American adults are explored in Chapters 4 and 5 of this text (Waite & Brooks, 2013).
As previously noted, while ADHD often persists from childhood into adulthood, its presentation usually becomes more subtle as the individual ages. Frequently, there are fewer overt symptoms of hyperactivity or impulsivity, but challenges with restlessness, inattention, and disorganization remain (Kooij et al., 2010). These latter concerns tend to be the elements of ADHD that so negatively impact interpersonal and close relationships.
Earlier conceptualizations of ADHD characterized it as a childhood disorder, with little impact beyond young adulthood (Kooij et al., 2010). However these authors noted that as early as 1976, reports appeared in the scholarly clinical literature that challenged this notion (Kooij et al., 2010). Since then there has been growing consensus that at least some elements of ADHD tend to persist into adulthood for many individuals. Several authors reported that ADHD symptoms continued for about two-thirds of children into their adult life spans (Adler et al., 2010; Dowson, 2008). Fedele et al. (2010) similarly estimated that ADHD was still evident in adulthood among children who had the disorder in about 70 percent of the cases they studied. Thus, the trend from these studies might place adult ADHD persistence rates at about 60-70 percent.
Conversely, Chao et al. (2008) places this number of persistence for full ADHD symptoms from childhood into adulthood at only 33 percent in their study of young men with ADHD, with comorbid mood and anxiety concerns. Finally, while in children there may be a disproportionate number of males identified as having ADHD compared to females, the gender disparity in adult ADHD diagnosis may be far less, with a more even ratio of males and females exhibiting enduring symptoms of the disorder (Babinski et al., 2011).
When discussing the prevalence of ADHD in adults, however, it is important to contextualize that rates of diagnosis vary by nation. In the USA, Biederman et al. (2007) estimated that about 4 percent of adults (i.e., 1 in 25 adults) were impacted by ADHD. This finding concurs with Cumyn, French, and Hechtman’s (2009) prevalence of ADHD in the USA at 4.4 percent of the adult population. ADHD diagnosis appears to be more common in higher-income nations, such as the USA and France, than in lower-income nations, such as Colombia and Mexico (Rösler et al., 2010). Whether this finding reflects greater levels of awareness, specific environmental influences in the development of ADHD, and/or diagnostic biases in certain countries is uncertain.
Biological Roots of ADHD
In addition to the possible environmental influences of adult ADHD, a strong line of research in recent decades has supported a neurobiological foundation for ADHD. In this regard the disorder is not considered to have an exclusively or nearly exclusively determined genetic basis, as in the case of Huntington’s disease or certain types of breast cancer, but rather a complex set of biological and environmental factors which in certain combinations and mutual interactions likely yield the eventual emergence of ADHD in the early lifespan. This is not unlike the diathesis-stress model which has been developed to conceptualize the etiology of schizophrenia and depression (Ingram & Luxton, 2005).
Adler et al. (2010) characterizes ADHD as a chronic neuropsychiatric condition involving deficits in sustained attention and/or impulse regulation. The biological vulnerabilities for ADHD might also be common to other disorders and difficulties. It is known, for instance, that ADHD is frequently comorbid with a number of other psychiatric conditions, including bipolar disorder, anxiety, learning disorders, and depression (Agarwal et al., 2012; Wadsworth & Harper, 2007). Chao et al. (2008) found that after controlling for age, young men with ADHD in the Taiwanese military experienced higher levels of depression and anxiety symptoms than non-ADHD controls. These researchers also suggested that the presence of the latter two comorbid conditions might accentuate certain deficits characteristic of ADHD, such as problems with working memory and executive functioning. One potential limitation of the study however was that an ADHD diagnosis was not actually established by a clinical interview, but suggested by a sum score on a self-report symptoms inventory, leading to potentially greater misclassification and potential bias.
Comorbid Conditions with ADHD
In a study examining the possible link between ADHD and conduct disorder, another frequently comorbid condition, Dowson (2008) suggested that ADHD comorbid with conduct disorder in adolescents may comprise a distinct subtype of ADHD as it occurs later in adulthood. The links between common comorbid conditions, or even common biological pathways of symptom expression involving ADHD and other disorders, are still quite preliminary, and will probably be an area of significant growth in the understanding of ADHD.
Another condition possibly linked with ADHD that is worth mentioning is a non-Alzheimer’s form of progressive dementia, called dementia with Lewy bodies (DLB). This condition is sometimes difficult to clinically recognize early on, but can be distinguished from Alzheimer’s disease by its relative initial integrity of anterograde memory functions, early presence of florid visual hallucinations with limited awareness, early periods of cognitive impairment alternating with phases of relatively intact cognitive functioning, and Parkinsonian motor symptoms (Blumenfeld, 2010; Mesulam, 2000).
With respect to DLB, a study by Golimstok et al. (2011) documented a higher number of participants presenting with the symptoms of DLB later in life who had previous histories of ADHD than in participants who developed symptoms of Alzheimer’s disease or in healthy controls. While the writers could not identify a specific link between ADHD and DLB that might clearly explain this, they postulated that a common association between both disorders involved neurotransmitter levels. Specifically, both DLB and ADHD involve decreased cortical levels of dopamine and norepinephrine (Golimstock et al., 2011).
One final area of study potentially supporting a biological basis for ADHD comes from the study of brain structure and real-time brain functioning. Using these methods, certain areas of the brain are potentially implicated to play a role in the symptoms of ADHD. Because of the extreme complexity of the brain and its extensive reliance on white-matter connections and wide-spanning circuits, simply identifying an area of the brain that seems to be shaped differently or that functions differently among individuals who have ADHD does not equate to it being a brain structure that necessarily causes an ADHD symptom.
That being said, structural neuroimaging (e.g., MRI and CT scans) and functional neuroimaging (e.g., PET scans and fMRI) have implicated reduced physical size and decreased metabolism in several regions of the brain that are associated with some of the common cognitive deficits of ADHD, such as working memory, divided attention, and executive functioning. These include the prefrontal cortex, anterior cingulate gyrus, and certain subcortical structures such as the globus pallidus and putamen (Arnsten, 2009; Rösler et al., 2010; Sato et al., 2012). The findings suggest a possible pathway by which some of the noted deficits and challenges of ADHD might occur at a physiological level. Again, they are linked with these deficits but are not necessarily the cause of these problems, as they may be part of a wider circuit that is aberrant due to ADHD, or perhaps indirectly impacted by another brain structure that is functioning sub-optimally in the brains of individuals with ADHD (Afifi & Bergman, 2005; Blumenfeld, 2010).
Genetics
Another area of recent interest in terms of the biological bases of ADHD involves the exploration of genetics. The technical aspects of this work are beyond the scope of this chapter, but some of the newer findings may be helpful to mention.
As part of a wider discussion on ADHD, Kooij et al. (2010) reported that adoption, twin, and family studies have all suggested a substantial degree of probable genetic influence in the development of ADHD. These authors note that there is an increased familial risk for ADHD among relatives of an individual with the disorder, and that this finding cannot be explained by environmental factors alone. ADHD has been linked with the latrophilin 3 gene, which is present in some of brain structures mentioned above, including the caudate nucleus, cerebellum, and amygdala (Agarwal et al., 2012).
While genetics and other biological factors are known to play a significant role in the development and symptom expression of ADHD, very few would argue that ADHD is caused by biological sources alone. Rather, the scholarly literature has linked ADHD and specific environmental conditions, including prenatal exposure to alcohol





























