18,49 €
Mehr erfahren.
- Herausgeber: Crowood
- Kategorie: Lebensstil
- Sprache: Englisch
The age-old practice of food fermentation is enjoying a well-earned renaissance. As knowledge around the importance of our gut microbiota has grown, so too has the evidence that fermented foods can help support a healthy gastrointestinal tract, boost the immune system and even improve mood. This is due to both the probiotic microbes they contain, and the enhanced nutritional value of fermented foods themselves. In this comprehensive guide, fermentation specialist Caroline Gilmartin delves into the processes and mechanisms involved in both wild and cultured fermentation, examining the microbes involved, parameters for optimal fermentation and what happens if you alter them. Topics covered include the importance of the microbiota; gut health; milk and water kefir; yoghurt; kombucha; vegetable fermentations; appetizing recipes; suggested flavour combinations and finally, safety measures and troubleshooting.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 331
Veröffentlichungsjahr: 2020
Ähnliche
FERMENTEDFOODS
A Practical Guide
FERMENTEDFOODS
A Practical Guide
Dr Caroline Gilmartin
First published in 2020by The Crowood Press LtdRamsbury, MarlboroughWiltshire SN8 2HR
www.crowood.com
This e-book first published in 2020
© Dr Caroline Gilmartin 2020
All rights reserved. This e-book is copyright material and must not be copied, reproduced, transferred, distributed, leased, licensed or publicly performed or used in any way except as specifically permitted in writing by the publishers, as allowed under the terms and conditions under which it was purchased or as strictly permitted by applicable copyright law. Any unauthorised distribution or use of this text may be a direct infringement of the author’s and publisher’s rights, and those responsible may be liable in law accordingly.
British Library Cataloguing-in-Publication DataA catalogue record for this book is available from the British Library.
ISBN 978 1 78500 758 3
CONTENTS
Preface
Acknowledgements
1 Introduction to the Microbiota and Gut Health
2 Fermentation: The Basics
3 Yoghurt
4 Milk Kefir
5 Water Kefir
6 Kombucha
7 Wild Fermentation
8 Brined Fermentation
9 Kimchi and Other Paste-Wrapped Ferments
Appendix: The Vege-Table
Glossary
Recommended Suppliers
References
Index
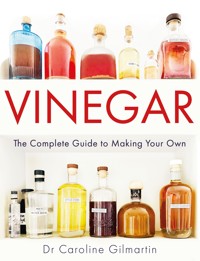
A fermenter’s shelf.
PREFACE
As a human it is tough to come to terms with the fact that we aren’t nearly as important as we think we are. We have always looked at the evolution from simple unicellular organism to complex multicellular being as progress; but what if it’s just bigger, not better?
The nineteenth-century microbiologist Louis Pasteur was on the right track, when he said, ‘C’est les microbes qui auront le dernier mot’ (‘the microbes will have the last word’). From the first sighting of tiny ‘animalcules’ by Antonie Van Leeuwenhoek in the 1680s, it has taken us 300 years to learn how to study them by examining their genetic code. We now know that microbes not only occupy every domain on earth, from the top of Everest to the bottom of the Mariana trench, but that there are probably billions of different species. So far, we have identified just a few thousand. We also know that our lives and theirs are closely, symbiotically intertwined – we are covered in them from head to toe and we have a trillion inside each of our gut microbiota.
And before we even knew of their existence, as far back as the Neolithic era, humans were unwittingly benefiting from microbial activity, as the first fermented drinks and foods were created. Fast forward several thousand years and, despite the seemingly endless development of convenience and ultra-processed foods, the tradition of consuming fermented drinks and foods still endures in many cultures, as an integral part of everyday life. Perhaps it is possible to combine progress with the past, by making some of our own food, enjoying the process and appreciating the results.
This book will explore two different mechanisms: cultured fermentation and wild fermentation. In cultured fermentation, the process is carried out by tangible sources of bacteria and yeast, such as kefir grains, yoghurt starters and kombucha SCOBYs (symbiotic cultures of bacteria and yeasts). Wild fermentation involves nothing more than the naturally occurring microbes on fruit and vegetables, using certain techniques to promote the growth of those that are most helpful to us. To put the use of the mechanisms into context, it will also examine current knowledge about both the gut microbiota and fermentation principles. Although this is not a recipe book as such, some recipes will be followed to show how the methods may be put into action. Then it will be up to you.
ACKNOWLEDGEMENTS
It is not every day that someone is asked to write down everything they know about their favourite subject, but this is what happened to me. It has been an honour, a privilege and at times a nightmare, and it could not have been achieved without the help and support of a lot of people. As this is a method book I shall start with my parents for having me in the first place, and my husband and children for being perfect. I must then thank Xanthe Clay for kicking me into action one day a few years ago when she insisted that I knew enough to do a fermentation demo, and Katie Venner, who kindly put my name forward as a potential author. A whole host of the UK’s growing band of fermenters shared their ideas, and gave me help and encouragement, most notably Rose Whitehouse, Alana at Fermented by LAB, Katie Venner, Jo Webster, Tara Clist, Lisa Cadd and Beth Osbourne.
I have to mention all my workshoppers who have attended Kefir School, Kimchi College and Kombucha Class, because I have learned so much by teaching this subject to such interested and inquisitive people. EveryGoodThing’s Instagram and Facebook friends everywhere deserve a mention too.
Thanks to Markas Gilmartin and Nicola Armstrong for making sure the chemical/nutritional bits were right, and the two Joannas – House and Webster – for helping me to get all the information I needed. A great deal of fun was had working with Eliza Moreland taking the photos (all the best ones are hers!) – thank you to Hugo the greengrocer, Lizzy Skirton and Sally for being very photogenic.
AWAKE! for morning in the bowl of nighthas flung the stone that puts the stars to flight.Rubiyat of Omar Kayam
CHAPTER 1
INTRODUCTION TO THE MICROBIOTA AND GUT HEALTH
FERMENTED FOODS
A Potted History of Fermentation
Imagine how excited our Anthropocene ancestors must have been when they discovered fermentation in action for the first time. Getting that warm fuzzy feeling from eating over-ripened fruit might have been where it all started. Recent investigations have identified what may have been the world’s first brewery, with 13,000-year-old residues of beer having been discovered in a cave near Haifa, Israel. The consumption of yoghurt may date back as far as 10,000 years, when the action of thermophilic bacteria in raw milk kept in goatskin bags produced a soured, thickened, creamy foodstuff, the heat of the African climate providing the perfect temperature for it to set. It must have been a revelation – a way of both preserving and extending the diet. Over subsequent years, sauerkraut, kimchi, kombucha, kefir and water kefir have all have had their moments of discovery.
Interestingly, these foods have endured for thousands of years, probably because they could be preserved for many months, and were also found to be beneficial to human health. It is even possible that these early diets influenced the formation of the human gut microbiota.
Residues of alcohol have been found in 13,000-year-old pot fragments.ADOBE STOCK
The heat of the desert – a perfect temperature for yoghurt to form in goatskins.ADOBE STOCK
What is ‘Fermentation’?
The word ‘fermentation’ means different things to different people. To the microbiologist or biochemist, it is the utilization of carbohydrates by microbes in the absence of oxygen. To the wine or beer maker, it is the action of, specifically, yeast upon sugar to make alcohol. For someone who is interested in fermented foods, however, the definition becomes much wider; it is not restricted to precise biochemical pathways and can include any food that is pleasantly or usefully altered by microbes:
Fermentation is a controlled process where microbes use carbohydrates to produce a range of useful end products, including lactic acid, alcohol and acetic acid, which can also preserve and enhance food and make new flavours.
One of the most curious things about fermentation is how it differs from decomposition – the process by which food rots. Both are carried out by microbes, but the two outcomes are poles apart. Consider a cabbage that has been left sitting in the vegetable basket for some time; the leaves start to yellow, bacteria and fungi start to feed upon it and after three or four weeks it will be a pile of black-brown mush. However, by removing the oxygen and adding a little salt – that is to say, controlling the conditions in which it finds itself – it is possible to supress the growth of the microbes associated with decay, while encouraging others to produce lactic acid. The result will be a perfectly preserved, nutritiously enhanced vegetable, sitting in a delicious tangy brine.
Doing It Yourself
Changing the humble cabbage into sauerkraut (and, indeed, milk into yoghurt or tea into kombucha) involves science, alchemy and a little magic, but it is essentially a simple process. However, making your own kimchi, fermented chilli sauce or preserved lemons will introduce you to a whole new range of flavours that you never knew existed. And you will have created them all on your own – well, you and just a few billion microbes!
A plain white cabbage: decomposition on the left and fermentation on the right.E MORELAND
Of course, you could just pop to the shops for your kefir and sauerkraut, so what are the benefits of doing it yourself? First, when processes are industrialized, corners are cut, natural variation is eliminated, and products change. For example, many brands of shop kefir are made by reconstituting acid whey waste from commercial Greek yoghurt production with isolated milk proteins to make a base. Individual bacterial cultures are then added to the mix and a short fermentation conducted. This is a far cry from the kefiran-rich symbiosis of home-made milk kefir. Similarly, much commercially produced sauerkraut is pasteurized, so that it remains stable for transportation and storage. Often, starter cultures are introduced for reproducibility purposes, reducing the natural variety of strains involved.
Second, home fermentation is extremely economical. While artisanal fermented foods are comparatively expensive to purchase, because the processes are difficult to scale up, they are easy to do yourself in small quantities.
Fermentation can also be great as a collaborative experience – large-scale vegetable prep is best done with friends, with chatter and sharing of expertise and ideas. It is often better to be shown how to do something than to read about it, which is probably why fermentation workshops are so popular. Hopefully you will have the confidence to be one of the expertise sharers after using this book.
Fermentation is even better with friends.
THE HUMAN GUT
There is a growing body of evidence around the health benefits of fermented foods, but why exactly are they good for human health, both prebiotic and probiotic? During fermentation, microbes synthesize vitamins and minerals, increase the digestibility of proteins and carbohydrates, increase the bioavailability of phytochemicals (plant compounds) and produce bio-active compounds that have important health benefits. Many of the microbes involved are probiotic, probably leading to the prevention and improvement of many chronic and metabolic conditions.
The human gastrointestinal tract.
From a scientific perspective, it is an exciting time to be a human. Over the past 30 years, it has become clear that the human being as an ‘individual’ does not really exist. Within every large intestine resides the microbiota – an enormous 2kg population of about 40,000,000,000,000 (40 trillion) microbes, including around 400 known species of bacteria, plus fungi, protozoa, viruses and bacteriophages. They work together to play an essential role in almost all of the body’s daily functions. The microbiota is so integral to the body’s survival and development that it is considered a virtual organ, or sometimes even the second brain.1
The microbes in the microbiota contain many more genes than a human does, which make hundreds of thousands of metabolites. To date, over 100,000 different human metabolites have been listed on the Human Metabolome Database.
If it were stretched out, the gatrointestinaI (GI) tract would be about 9 metres or 30 feet long. It extracts nutrients from the food you eat, while leaving the waste products behind and protecting the internal environment of the body. As the lining of your gut is first-line defence against invasion from unwanted microbes and particles, 70% of your immune system can be found in its walls.
The gut microbiota resides in the colon and constitutes about 80% of your body’s microbes; the rest occupy your skin, mouth, urogenital and upper GI tracts. It does not sit there like an enormous lump: microbes occupy the inner folds of the lumen, are mixed up in the digesta (the mass of fibre that passes through your intestine) and also in the colon’s double mucous layer.2
The human body has just 23,000 genes that make proteins involved in growth and development. This may seem a low number for something as complex as a human – in fact, tomatoes have more genes than a human – but the microbes in the microbiota contain over 3,000,000 genes. (These genes in the gut are referred to as the ‘microbiome’ rather than the ‘microbiota’, which refers to the microbes themselves.) Humans have outsourced production of thousands of important compounds to the gut microbes. These ‘metabolites’ (products of metabolism) make up the ‘metabolome’. Some metabolites are produced by several different bacterial species, and it does not matter which makes it as long as you have the product. Others are made by specialized bacteria; these metabolites cannot be replaced if the microbes are lost.
It seems that the microbiota has shaped the development of Homo sapiens, gradually gaining additional advantages from the colonization of the gut by these ‘external’ yet essential microbes. One clue to this theory is the discovery, for example, that Japanese people can easily digest seaweed, because their microbiota have specific enzymes from marine bacteria.3 Another is that the microbiotal production of equol, which can reduce hot flushes in menopausal women, is produced in twice as many women in countries with high soy consumption.4
THE MICROBIOTA
The functions and role of the microbiota are immensely complex and diverse, but, at the top level, they break down plant fibres that the body cannot digest itself, and make vital metabolites.
Just a few of the most well-studied functions of the microbiota. There seems to be an axis with every organ: gut–brain, gut– kidney, gut–heart, and so on.
Microbiota Development
Early Years
Colonization of the gut might begin even before birth, as it seems that the placenta and umbilical cord are not as sterile as first thought. However, for a normally delivered baby, it all starts upon contact with the vaginal microbiota and associated faecal organisms. Caesarean-born children have microbiotal differences, which are evident for some years afterwards.
Factors influencing the development of the gut microbiota from conception to age 3.
Breast milk plays the next crucial role, with Bifidobacterium infantis bacteria in the infant gut breaking down the oligosaccharides (sugars) it contains. Bottle-feeding can also affect microbiotal development.5
Infancy is the ‘window of opportunity’ that can shape the microbiota and also affect future susceptibility to conditions including allergies and asthma. By the age of 3, it is pretty stable (with good health/lifestyle) and remains so until old age, when some of the species are lost.
Genetics
Many of a person’s characteristics are determined by their genes. 99.9% of human DNA is the same in everyone but the 0.1% difference is what creates individuals. Some of the genes probably influence the types of bacteria that are in the microbiota. For example, more lactase-producing bacteria exist in the gut of some people who have a problem with the lactase-making gene.6 However, as even identical twins can have very different microbiota, the role of genetics is not clear-cut. Within families there does seems to be a ‘core’ microbiota7, although separating this as a genetic issue from the effects of cohabiting is tricky. There is gender-specific variance too, which might be because of disparities in male/female immune systems, which may allow different microbes to colonize the gut.8
Other Factors
Geographical location – city or countryside, island or inland – and lifestyle (westernized or hunter-gatherer, for example), all have an influence. The administration of antibiotics is also significant. Their over-use is not just bad for creating resistant microbes, it can also have a long-term effect on the microbiota, especially in early childhood.
Colonization
The adult microbiota consists of hundreds of species that exist nowhere else in nature. Other than via birth/ breastfeeding, they need other routes of entry. Some microbes are strict anaerobes, which cannot survive in the presence of oxygen, so they have elaborate strategies for survival. Faecal transmission plays a role in this: organisms leave the host in faecal matter and survive in an environment – people, food, animals, objects, surroundings, especially bathrooms – until ingested by a new host. They then need a colonization strategy to avoid host defences and to survive in the gut.
The immune system is so highly specialized it can tell the difference between pathogens and these useful bacteria. People who live in the same house share more species than non-cohabiters; shaking hands, hugging, kissing and having sex are all ways of transmitting microbes. Other routes for less specialized species that can survive outside of the gut include raw fruit and vegetables, water, the environment and animals, especially pets.
The Perfect Microbiota?
The perfect microbiota probably does not exist. It is believed that there are about 5,000 microbiotal species in total, but many have not yet been characterized. Although there is a core of microbes present in most people, there is no single optimal gut composition; each one is as individual to its host as a fingerprint. A healthy microbiota is ‘highly diverse’, with between 600,000 and 3 million bacterial genes and probably at least 400 different species.
Once established, the microbiota can vary, but the same core species endure. Some types of bacteria are particularly associated with good health, for example, Christensenella and Akkermansia sp. are rare in overweight people, yet common in the lean and/ or physically fit. More microbial diversity is better for health and wellbeing, and that diversity is heavily influenced by diet.
DYSBIOSIS
The microbiota can adapt to a degree of change, but sometimes things go too far. This is called dysbiosis (the opposite of the usual symbiotic relationship a body has with its microbiota) and is linked to a huge list of about 70 health problems, including bowel disorders, inflammatory bowel disease, allergies, coeliac disease, obesity and diabetes, neurodegenerative conditions and several types of cancer. It is not clear which comes first, the disease or the dysbiosis. In fact, it probably varies, or one may exacerbate the other. There are several different ways in which the microbiota can be off balance.
Examples of dysbiosis include loss of beneficial bacteria (people who are deficient in Coprococcus sp. and Dialister sp. have been found to be more susceptible to depression9), and overgrowth of pathobionts (in which bacteria that are not usually harmful can take over and have negative effects; this may be a factor in colorectal cancer10).
General Symptoms
Dysbiosis as an underlying cause for illness is generally not yet recognized by the medical profession; it is always seen as a symptom of something else. Because it could be cause or effect and there is an enormous range of symptoms, including bloating, abdominal cramping, unusual bowel behaviour, indigestion, food intolerances, fatigue, moodiness, depression, joint pain, skin conditions, it can be hard to identify. Alternatively, a patient might present with specific symptoms of one of the conditions mentioned. Faecal sample analysis is likely to be used more commonly in the future to see whether there is an issue.
Leaky Gut
One of the internal effects of dysbiosis is increased intestinal permeability or ‘leaky’ gut. Although a little leakiness is normal, if the microbiota is not making the right components for the gut lining, it can become severe. Gaps can appear between the cells forming the gut wall, and tiny fragments of food or microbes can end up in the tissue outside the gut. This can trigger an immune response, leading to inflammation of the gut lining. Maintenance of the mucous layer and the tight junctions between cells is pivotal to gut health.
The cells lining the gut are linked together by tight junctions. Failing to make the right components to maintain these junctions can cause the gut to become ‘leaky’. Channels can open up, and tiny particles may reach the lower layers of the gut lining, setting off inflammation.
When the microbiota ferments the fibre in the colon that the body cannot process, some of the most important end products are short chain fatty acids (SCFAs). (They may also be referred to by their specific names, such as butyrate, acetate or propionate.) They are extremely important in strengthening the gut barrier and regulating the immune system, in order to keep inflammation at bay.
EATING FOR GUT HEALTH
Everybody has a fair amount of control over the state of their microbiota, as lifestyle choices can impact gut, physical and mental health. With every mouthful, you never eat alone – what you eat, your microbiota eats. Changes to the microbiota can happen extremely quickly. Just a couple of weeks of ‘holiday eating’ – burgers and chips with a few glasses of wine, puddings and ice creams – are enough to cause loss of diversity and alterations to immunological and metabolic functions.
The good news is that, if you have a healthy microbiota, and the diet change is temporary, bacteria hidden in the crypts of your guts, and your appendix if you have one, are able to restore the balance. The bad news is that no one really knows how long it is possible to eat like that before dysbiosis begins to play a role in the development of a metabolic disorder. It is probably best to switch to a healthy diet as soon as possible.
You are how you live: there are many factors that may have a negative influence upon the diversity of the microbiota. Smoking and the contraceptive pill have also been implicated.
Prebiotics
Simply put, prebiotics are foods for the microbiota. The better nourished the gut microbes are, the greater diversity there will be and the more useful end products of metabolism will be produced.
Fibre
Dietary fibre is found only in plant-based foods. One of the major roles of gut microbes is to digest it for the body, as it cannot be assimilated otherwise, unlike the proteins, fats and sugars, for which the body has the enzymes. There are different types of fibre. Some act as bulking agents for the stool, while others, such as inulin, resistant starch and fermentable oligosaccharides, provide energy for the microbiota. These are usually referred to as ‘microbe available carbohydrates’, or MACs.
When MACs reach the large intestine, the microbes ferment them (just like in sauerkraut!), producing SCFAs. In the presence of a low-fibre diet, or a very high-fat one, the microbes are under-nourished. The result is that they eat too much of the top mucus layer, and work their way into the lower layer, where they should not be. They start making the wrong sort of products from their metabolism, which can be harmful. When the microbes or products get this far, they are sensed by the immune system, which can cause an immune, inflammatory response.
Polyphenols
Polyphenols are a huge class of phytochemicals that contain the compounds that colour fruit and vegetables. They are also found in dark chocolate, coffee and red wine, which is why these seemingly indulgent products can be included in a healthy diet. Most polyphenols reach the colon where they become a delicious nutrient source for the microbiota, which releases beneficial metabolites from them. Polyphenols also help to maintain microbiota balance, inhibiting potential pathogens and stimulating proliferation of beneficial species with their breakdown products.
The Hadza tribe in Tanzania: as near as possible to a perfect microbiota?ADOBE STOCK
Thirty Plants a Week
The Hadza tribe of hunter-gatherers in Tanzania have the most diverse microbiota in the world today. Their ancient and largely unaltered diet comprises a huge range of foraged plant-based foods, with occasional helpings of meat. They regularly eat over 30 varieties of plant each week, providing their microbiota with many different types of MACs and polyphenols. After just three days of eating with the tribe, professor of genetics Tim Spector saw his microbiota increase in detectable species by 20% (shown by stool sample analysis). Unfortunately, however, this change was not sustainable and within days of the professor returning home it had returned to its former state.9
Spector’s research has led a team at King’s College London to propose that one of the best ways of improving gut heath is to consistently eat an extremely varied diet, based on 30 different plant-based foods a week. The reasons for this are that each of the different types of microbe in the microbiota (there may be as many as 400) have slightly different nutritional requirements, which can be met by eating a vast range of foods all containing slightly different MACs and phytonutrients. This does not imply a need to become vegan or vegetarian; it is not necessary to exclude either dairy or a modest amount of meat.
As unachievable as this may sound on paper, a 30-a-week plan does not require fixed portion sizes, and includes herbs, spices, seeds, nuts, pulses, whole grains, fruit and vegetables. Easy wins are buying ready-mixed dried rice/grain mixtures for cooking, mixed bags of salad, and mixed nuts and seeds to sprinkle on top of things.
Probiotics
Probiotics are ‘live bacteria and yeasts that, when administrated in adequate amounts, are beneficial to human health’. The word ‘probiotic’ meaning ‘for life’ is derived from Greek – the opposite to ‘antibiotic’ in fact. The first inkling that certain bacteria were beneficial was reported by microbiologist Eli Metchnikov over 100 years ago, in his text Studies on Optimism: ‘With various foods undergoing lactic acid fermentation and consumed raw (sour milk, kefir, sauerkraut, pickles) humans introduced huge amounts of proliferating lactic acid bacteria to their alimentary tracts.’10
These days, in order to be designated as probiotic, a microbe must have passed rigorous lab tests, and have been shown to be non-pathogenic, able to survive the GI-tract journey to the colon, and to have a proven effect. Probiotics are available in liquid capsule form and as dried supplements, but it is also possible to take a more natural approach, as exactly the same kind of microbes are found in fermented foods. Some examples of known probiotics include:
•Lactobacillus rhamnosus GG
•Lactobacillus acidophilus CL1285
•Saccharomyces boulardii CNCM 1-745
•Bifidobacterium bifidum W23
Some might say that the advantage of having supplements with probiotics is that it is easy to identify exactly what you are consuming. I would counter that with a list of why functional foods can beat a capsule:
•Variety. Functional foods contain myriad species of LAB and also functional yeasts, which can all have positive effects on the microbiota. In some cases, this could be more beneficial than a huge influx of a very limited number of species.
•Health. Functional foods are so much more than a capsule. They are nutrient-rich sources of vitamins, minerals, short chain peptides, phytonutrients, organic acids, fibre. Food is not just for nutrition. It also protects the microbes from conditions in the GI tract, increasing their chances of arriving unscathed.
•Prebiotic. Fermented vegetables are prebiotic too, containing a range of phytonutrients such as polyphenols and MACs.
•Sustainable. Probiotic capsules are big business, produced in large quantities in busy factories. On the other hand, fermented foods are economical and sustainable, with no ultra-processing required.
•Functional. It is possible that the natural symbiosis of strains that grow together is more beneficial than those artificially grouped in probiotic capsules.
Although probiotics seem to be mentioned in the general media almost daily, the mechanisms for their action are not well understood. It seems that they communicate with the existing gut microbiota by some kind of ‘cross-talk’, sending chemical messengers using complex pathways. In the most basic sense, they kick the gut microbiota into action, and fight off the pathogens, via some of the following actions:
•Attaching to sites on the gut mucosa, preventing pathogens from adhering.
•Stimulating the immune system, by sending chemical messengers across the membranes.
•Fermenting MACs to produce the ever-helpful SCFAs.11
•Altering patterns of gene expression for immune and mucosal genes (turning them up, a bit like a dimmer switch).
•Encouraging the proliferation of beneficial species perhaps by the production of growth factors, or substrates for commensals to use.
There is some debate about whether probiotic organisms ‘colonize’ – become permanent residents of – the gut or not. The answer in most cases is generally not, or certainly not permanently. They are rather like tourists, who come to visit a city, stay for a couple of weeks, buoy up the local economy and then go home!
There are various complicated mechanisms involving surface molecules, by which they could attach, but one thing is certain – they are not recognized as pathogens and the body does not raise an immune response against them. They are not competitively excluded from attaching to the mucosal surface by the existing microbiota either.
THE PERSONALIZED DIET
As each person’s microbiota is as individual as that person, researchers have been studying the body’s individual responses to food. The ‘Predict’ study has looked at the responses of identical twins to the same foods. Even identical twins have different microbiota, and they do not have the same response to food; their glucose, insulin and dietary fat levels (which may be used as metabolic markers) were found to vary significantly after the consumption of the same foods.12 Another study has shown the same sort of results with people’s individual responses to bread.13 However, even with this knowledge, the next step – what to do with it, in order to give personalized dietary advice – is complicated. It is thought that only a fraction of the responses were due to the fat, sugar or protein content of the food. The rest was probably to do with the micronutrients, or even additives from ultra-processed food.
HOW TO EAT FERMENTED FOODS
Can fermented foods change your life? Possibly, especially if you have previously been a sickly person, seemingly susceptible to every passing germ. Although not everyone will see immediate benefits, as it depends on the status of their own particular gut, in preventive terms, the impact of fermented foods could be significant. There is a possibility that metabolic and autoimmune disorders or even cancers could be avoided by maintenance of good gut health, but a major retrospective cohort study will be required before this can be asserted.
Eat fermented foods little and often; they are nutrient-dense, and fermented vegetables have always been salted. Aim for diversity, with several different types on the go at the same time!
All fermented foods are extremely nutrient dense and the additive effects of too much of a good thing are unknown. Apart from purchased yoghurt cultures, it is not possible to know what probiotic microbes they contain or what microbes are in your own microbiota and how they might interact. As a result, it is necessary to start eating fermented foods in small quantities – a spoonful of sauerkraut, a couple of sips of kefir – and then see how you feel. Any gastrointestinal gurgling is likely to pass as the microbes are usually transient gut visitors. The amount can then be increased gradually over a few days. This is especially important if you have IBS/IBD, as individual responses can differ hugely.
Fermented foods are suitable for almost everyone, but there are caveats. You should start eating them when you are well, not when you are in the middle of any kind of serious illness, especially any form of cancer, or any other condition where you may be immuno-compromised. If you have had recent gastric, hepatic or dental surgery, you must check with your consultant first. Occasional infections have arisen post-surgery in chronically ill patients; almost all caused by large doses of just one type of microbe from probiotic capsules. In this regard, the natural symbiotic interactions of fermented foods may be preferable to capsule monocultures. Some researchers are concerned that antibiotic resistance genes present in the environment could transfer to probiotic bacteria. To be honest, they probably already have, and into lots of your gut microbes.
Fermented vegetables have a 2% salt content, so you should be aware of this if you need to watch your intake. All fermented foods also contain the biogenic amine histamine to varying degrees, which can cause allergic reactions in intolerant individuals. Remember, though, even if you cannot tolerate fermented foods, you can still improve your gut health through the prebiotics route: diet, fibre intake and exercise.
CHAPTER 2
FERMENTATION: THE BASICS
FOOD-FERMENTING MICROBES
Microbes are organisms that are so small they are only visible (singly) under a microscope. However, although they may be small, they are not simple! Consisting of just a single cell, they are like a factory with everything in one place – electrical wiring, gas supply, windows and doors, a sewage system, machinery for manufacturing, food and water. In reality, this translates to a cell envelope that allows transport in and out, which contains cytoplasm, where a mixture of water, genetic material, nutrients, protein synthesizing machinery and enzymes are all suspended.
The unwitting father of microbiology, Antonie Van Leeuwenhoek (1632–1723), was a textile manufacturer in the Netherlands. He was the first person to see microbes, when he developed lenses used for the inspection of fabric fibres to create a microscope.ADOBE STOCK
The basic structure of a prokaryotic bacterium. The colours are imagined; it can only be seen at this level with an electron microscope.
The basic structure of a yeast cell. Like humans, they are eukaryotes, sharing features such as mitochondria and a nucleus.
The number of different microbial species on the planet is the subject of much hot debate, but there may be as many as a few trillion. So far, just a few thousand have been identified and named.
There are two types of food-fermenting microbes: bacteria and yeasts. They are fundamentally very different. Yeasts are eukaryotes with their DNA inside a cell nucleus – just like humans, in fact. In prokaryotic bacteria, the DNA floats around the cytoplasm in a clump. What unites the two types is that they are all unicellular and contain all the machinery they require for growth and reproduction within their own selves. Their ability to ferment food is not deliberate, but comes as a by-product of their metabolism, which is then harnessed to produce the beneficial foodstuffs.
The microbes use different fermenting pathways: lactic acid fermentation, acetic acid and alcohol fermentation.
Electron micrograph showing the rod shape of Lactobacillus plantarum, a type of LAB.ADOBE
Lactic Acid Fermentation
Lactic acid is an organic acid with the formula CH3CH(OH)CO2H. It is similar to acetic acid or vinegar, although actually volume for volume it is about 10 times more acidic. It acts as a preservative for fermented foods.
Lactic acid bacteria (LAB) produce lactic acid (among other things) from carbohydrates including glucose, fructose or galactose. Many different types of bacteria have this property, including Lactobacillus, Lactococcus, Streptococcus, Weisella, Leuconostoc and Enterococcus species, but they may be referred to collectively as LAB. They are not just important in home fermentation; they are also major players in the food and biotechnology industries, used for the natural processing of chocolate, vanilla, olives, coffee and honey, and for the production of food additives such as dextran, and also now in the production of probiotics.
The different pathways for heterolactic and homolactic fermentation by LAB.
LAB can be divided into two main groups, depending upon which pathway they use to make lactic acid, for which they need a lot of sugar and little oxygen:
1.Homofermenters produce just lactic acid. Examples include Streptococcus thermophilus, Streptococcus lactis, Lactobacillus lactis, Lactobacillus bulgarius. Many of these are yoghurt cultures as their production of just this with a few additional flavour compounds gives the characteristic tang.
2.Heterofermenters produce lactic acid and, in addition, carbon dioxide and ethanol or acetate. Examples include species of Leuconostocmesenteroides, Leuconostoc lactis and Weisella sp. This is why one of the first signs of activity in vegetable fermentation is the formation of bubbles of carbon dioxide by heterofermentative L. mesenteroides.
Of course, nothing is that simple in science, so some microbes can be both homo- and heterofermenters, depending on their environment, including Lactobacillus casei, Lactobacillus rhamnosus and Lactococcus lactis.
LAB also contain enzymes that can break down proteins (via proteolysis) into smaller peptides and free amino acids. The amino acids can be further converted into flavour compounds including the various alcohols, acid and aldehydes that give fermented foods their distinctive flavours.
Some strains of LAB, such as L. delbrueckii, L.bulgaricus. L. casei, and L. plantarum, are able to break down fats (via lipolysis) if present, for example, in milk. This releases free fatty acids, glycerol and mono and di-acylglycerides. These compounds naturally emulsify other food components, which aid in the texture development of the final product.14
WHAT HAPPENS IN A MICROBE: HOW LACTIC ACID FERMENTATION OCCURS
Imagine a lone lactobacillus sitting in a jar of milk. Transporters in its cell wall recognize the lactose molecule and selectively let it in, acting like doormen. Once inside, the lactose molecule is recognized by beta-galactosidase, an enzyme that splits it into its component glucose and galactose parts. Some LAB can utilize the galactose but if they cannot, it is excreted back outside the cell (or thrown out by the doorman!).
Next, the glucose enters a complex cycle of reactions that extract its energy, resulting in the production of lactic acid. If the acid concentration is too high, it will become toxic to the cell, so it is excreted into the medium – in this example, milk kefir – where it acidifies it. This is just one of many simultaneous mechanisms in one microbe of billions in milk kefir.
Inside an LAB.
Acetic Acid Fermentation
Acetic acid bacteria (AAB) produce acetic acid from alcohol. This group includes Acetobacter, Gluconobacter and the inconveniently named Komagataeibacter sp. As well as having important roles in fermented foods, especially kombucha, vinegar and to a lesser extent milk and water kefir, they are used industrially for the production of vinegar. All are strict aerobes.
Acetic acid bacteria have peritrichous flagella – they are covered in them. These structures make them motile.
The enzymes required and the pathway that changes alcohol into acetic acid. This is performed by AAB.
Alcoholic Fermentation
Louis Pasteur first identified yeasts as the agents of fermentation in 1875, realizing that alcohol was produced anaerobically in the absence of oxygen. It is now known that many species of yeast also carry out the process in the presence of oxygen, as long as there is lots of sugar present. Examples include Saccharomyces sp., Brettanomyces sp., Candida sp. and Kluyveromyces sp.
Yeasts also produce invertase, an enzyme that breaks down complex sugars (for example, sucrose) into simple sugars such as glucose and fructose, which it can use to make alcohol. In water kefir and kombucha, these sugars also become available to LAB. Some bacteria, such as Zymomonas sp., can also produce alcohol from sugars, using a slightly different pathway. These bacteria may be present in water kefir grains or kombucha.