1,19 €
Mehr erfahren.
- Herausgeber: Dean Street Press
- Kategorie: Fachliteratur
- Sprache: Englisch
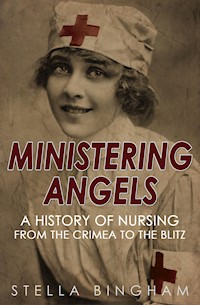
In the eighteenth century professional nurses were often written off as drunk, slovenly, or cruel. In the Crimea, under Florence Nightingale's direction, they had become known as 'Ministering Angels'. By the Second World War they wore battledress and worked on the front lines, on Hospital ships and in the bombed streets of London. They were universally regarded as a fundamental, dedicated, compassionate and disciplined component of the war effort. Ministering Angels elegantly traces the intervening history, and transformation, of the profession through war and peace. And it pays tribute to the tireless visionaries who helped change nursing, the professional sphere of women, and the world in the process. This new edition features a foreword by Yvonne McEwen, official historian of the British Army Nursing Service.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Veröffentlichungsjahr: 2015
Ähnliche
Stella BinghamMinistering AngelsA HISTORY OF NURSING FROM THE CRIMEA TO THE BLITZ
In the eighteenth century professional nurses were often written off as drunk, slovenly, or cruel. In the Crimea, under Florence Nightingale’s direction, they had become known as ‘Ministering Angels’. By the Second World War they wore battledress and worked on the front lines, on Hospital ships and in the bombed streets of London. They were universally regarded as a fundamental, dedicated, compassionate and disciplined component of the war effort.
Ministering Angels elegantly traces the intervening history, and transformation, of the profession through war and peace. And it pays tribute to the tireless visionaries who helped change nursing, the professional sphere of women, and the world in the process.
This new edition features a foreword by Yvonne McEwen, the official historian of the British Army Nursing Service since 2008.
Foreword
Forty years after her experiences in the Crimea, Florence Nightingale reflected on her achievements, and in particular on the establishment of a training school for nurses which opened on 15 June 1860 at St. Thomas’s Hospital in London. The ‘Lady with the Lamp’ had secured herself a place in the nation’s affections and, as a result, the training school had been established by public subscription. In 1892, she wrote:
There comes a crisis in the lives of all social movements. This has come in the case of nursing in about thirty years. For nursing was born about thirty years ago. Before it did not exist, though sickness was as old as the world.
Miss Nightingale was mistaken; men and women had been delivering care to the sick, injured and destitute for centuries. In times of warfare, there was a long established, though informal, practice of men and women supplying care and comfort for armies and navies. It was, perhaps, more a question of semantics as to what constituted ‘nursing’ and how it differed, if at all, from care-giving in the evolutionary practice of medical science and military medicine. Furthermore, the role of the nurse and military nursing did not evolve after the first salvo was fired in the Crimea – its origins date from antiquity.
One of the earliest references to the healing arts in warfare can be found in Homer’s epic poem The Iliad, where a detailed description is given of the physical and psychological consequences of warfare. Within the text, Homer cites in great detail at least 150 different types of wound inflicted by swords, spears and arrows. Throughout the poem, Homer refers to the medical and nursing care given to warriors. The poem also suggests that women had a role to play in caring for the battle casualties, referring to Agamede, daughter of Augeas, King of Epeans, who knew the healing power of every herb and who, in caring for the wounded at Troy, ‘prepared the gentle bath and washed their gory wounds’.
It was not the Greeks, however, who were the forerunners in the healing arts; the practice of healing had long been established in India, Ceylon, Egypt, Babylon and Assyria. In the ancient sacred text of India, the Vedas, the scriptures and folklore not only describe the healing arts but counsel caregivers on preventative medicine. Within the Vedas are discussions covering medicine, surgery, poisons, insanity, wounds, massage and the care of children.
From the information available about the ancient world, it can be seen that women practised nursing and the healing arts with a combination of skill, maternalism and mysticism. While not enjoying the same position in society as men, the female gods, as a conduit, gave women – priestesses, wise women, seers, healers and herbalists – an elevated status and acknowledgement of their ability to bring skill and succour to the health needs of both civilians and soldiers. James Stuart Blackie, the eminent Scottish Classicist, noted, ‘Nothing was more common in ancient times than the healing skills possessed by women.’
Those women were the architects of everything that followed in the development and practice of nursing, military nursing and care-giving.
In Ministering Angels Stella Bingham has produced a well-written history of the evolution of civilian and military nursing. The book, while concentrating on the period between the Crimean War and World War II, charts the history of nursing and military nursing over a vast timeline from the 4th to the 20th century. Her sources are credible and impressive. The book was first published in 1979, and in 2015 it is still on recommended reading lists for anyone interested in the history of nursing.
Stella Bingham combines a wealth of information with well sourced anecdotes to produce a colourful, illuminating and engaging text, and she sustains her literary style throughout each chapter of the book. The book content is international in scope and, in addition to Britain, the book makes reference to the development of nursing in Europe and North America.
The sixteen-hundred-year convoluted, and at times torturous, journey from informal care-giving to the professionalisation of nursing is littered with conventions, restrictions, abuse and tyranny but the drive for professional recognition was part of a much larger social revolution that resulted in personal and professional liberation and emancipation for women. Nurses were quite often the advocates for and pioneers of change and their work is celebrated and respectfully remembered in Ministering Angels.
In the past ten years there has been a resurgence of interest in the history of nursing and the reprint of this book is to be welcomed. Stella Bingham is a natural communicator and it is hoped the book will reach a whole new readership and welcome back previous admirers of this fine and popular history of nursing.
Yvonne McEwen
The Centre for the Study of Modern Conflict, University of Edinburgh
Official Historian of the British Army Nursing Service, 2008-present
1. In The Beginning
Women have nursed since the first mother gave birth to the first baby. Nursing has always been a woman’s duty, as much her responsibility as cooking, sewing and sweeping the floors: a domestic chore. Christianity made caring for the sick poor a work of charity, a penance, one of the most unpleasant jobs women (and men) could do to show their love of God. Even with the introduction of paid nurses – one of the consequences of the Protestant Reformation, particularly in England – things did not improve. The work was unpleasant, the hours killing, food and accommodation often poor, and wages low, and the sick poor got the sort of care they might have expected in such circumstances. Only in the last century did it begin to dawn on a few of the more enlightened doctors and social reformers that, with a little training, nurses might do more than care for a patient: they might help to cure. Woman’s oldest duty became her first profession.
While many ancient civilizations developed quite advanced systems of medicine and surgery and, particularly, of public hygiene and sanitation, women had only a small part to play in them. In the earliest days, medicine was inseparable from religion and superstition: medicine was magic, the priests were physicians and disease was the work of evil spirits. The functions of priest and doctor gradually separated but women’s work was generally confined to midwifery and nursing at home.
Christianity made a sacred duty of loving your neighbour and caring for the sick, the old and the afflicted. Deaconesses, ordained by the laying on of hands, achieved a particularly important position in the Eastern Church. They had the same role as consecrated virgins and widows, who undertook specific functions within the church and devoted their lives to charitable work, which included sick visiting. In the early centuries such women lived and worked freely in society, but gradually they formed themselves in to communities and hence their spheres of activity were limited and curtailed. Care of the sick was a particular responsibility of the bishops who, from the 4th century A.D., built separate hospitals for their care. One of the earliest and most magnificent was built by Basil, Bishop of Caesarea, in A.D. 370. The Basilias, like such later foundations as the Hôtel Dieu at Lyons (542) and the Hôtel Dieu, Paris (about 650), combined the functions of hospital, almshouse, orphanage and hostel, as it was not thought necessary to make a distinction between the various objects of charity. The first hospital in Rome was founded in 390 by Fabiola, a wealthy widow who was converted to Christianity, and in expiation of her former life and an unhappy second marriage, lavished her fortune on the sick and the poor.
In 817, the Council of Aix declared the care of the poor to be the chief duty of monastic communities. However, a gradual transfer of part of this responsibility had been taking place since St. Benedict (born 480) had declared in his monastic Rule, ‘Before all things and above all things care must be taken of the sick.’ The monastic life was particularly attractive to women as an alternative to marriage. The early nuns led free lives, most of them not even wearing distinctive dress. They were given the opportunity to develop their own interests, and many nunneries became centres of learning. The great double communities of monks and nuns were usually led by an abbess, often of the highest rank and ability. Hilda, Abbess of Whitby in the 7th century, was a kinswoman of the King of Northumbria. She trained many eminent monks and was a woman of national importance. The monasteries had wards for their own sick and many, particularly those belonging to the Benedictine rule, had separate buildings for travellers and the needy. Well-born ladies visited the hospitals to help care for the sick. The quality of medical care was low, but the spiritual tone was excellent.
By the 12th century, hospitals specifically for the sick were emerging as separate institutions. At the same time a number of religious orders were founded with the principal duty of nursing. In about 1050 a group of merchants from Amalfi, moved by the plight of the pilgrims pouring into Jerusalem , founded two hospitals in the Holy City. The one for men was under the protection of St. John the Almoner, the women’s, St. Mary Magdalene. After the capture of Jerusalem by the Crusaders in 1099, the Order of St. John, which had devotedly nursed the soldiers during the Crusades, was endowed with generous gifts and lands from all over Europe. Under the second Grand Master of the Order the members took the Augustinian Rule and added military duties to their nursing work. The Hospitallers were divided into three grades: the knights who bore arms and held the important positions, the priests, and the serving brothers who probably did most of the nursing. The Order was rich and glamorous and membership eagerly sought after. Their hospitals were well equipped and run with a military discipline which strongly influenced later hospital management. When Jerusalem fell to the Saracens in 1187 and Acre followed in 1291 the Knights lost all their possessions in Palestine and the few left alive escaped to Cyprus. They took and held Rhodes from 1310 to l522 and then the Holy Roman Emperor Charles V gave them Malta, where they remained until the island was captured by Napoleon Bonaparte in 1798. The female branch of the Order, however, apparently gave up nursing after fleeing from Jerusalem. The German Teutonic Knights were formed to serve the sick and poor and defend the holy places. Their first hospital was destroyed when Jerusalem fell in l187, but they re-formed and nursed wounded Christian soldiers during the siege of Acre in 1190. After Acre’s capture, they built a church and hospital there – but retreated to Venice and then Marienbad when the city fell finally into Moslem hands. Many hospitals in Germany were given to them.
The Knights of St. Lazarus undertook military duties as well as the care of lepers in Jerusalem, and elsewhere.
The oldest purely nursing order of nuns were the Augustinian Sisters of the Hôtel Dieu in Paris. By the 13th century they were completely enclosed under the control of the clergy, and only allowed to leave the hospital for visiting nursing. In 1212 a decree by the Bishops in Council instructed hospitals in France to use as few nursing sisters as possible in order to economize on the expenditure of charitable gifts, so the hospital was understaffed, the Sisters untrained, ill-fed and dreadfully overworked. The standard of nursing was fairly low, though some visitors commented on the Sisters’ cheerful loving manner. Periods of overcrowding saw as many as five or six patients in one large bed.
For centuries the clerical and civil powers fought over the administration of the hospital. Investigations led to reforms, and then to decline. In the 14th century there were reports of insubordination, insolence and moral scandal. In the 17th century the Sisters were accused of disobeying orders, neglecting the sick in favour of religious meditation, and selling drugs. Visitors at the end of the 18th century reported overcrowding, bed bugs, filth and insanitary conditions. Throughout, the Sisters, with justification, pleaded overwork. With the French Revolution came suppression of the Augustinian Order, though conditions were improved and the Sisters were allowed to remain as lay nurses.
The increasing decadence of the monastic orders led to the growth of secular equivalents, many of whom devoted themselves to nursing. The most interesting of the women’s orders were the Beguines of Flanders, founded in 1180 as a protest against the more restrictive and artificial aspects of monastic life. They were vowed to chastity and obedience but could keep their own property and were free to leave the order and marry. The women lived together in threes and fours in small houses, grouped in a precinct, and nursed in hospitals and in the homes of the sick poor. The order spread to Germany, Switzerland and France and by 1300 it had about 200,000 members. Its independence made it unpopular with the Church, but the civil authorities and the people both gave it their support.
It was not until the 16th, 17th and 18th centuries that a further flowering of religious and secular nursing orders took place, many doing noble and self-sacrificing work. The members of one sisterhood, the Camellines, all died nursing in the last great plague of Barcelona, for instance. The most important of these later orders were the Sisters of Charity, founded by St. Vincent de Paul in 1630. St. Vincent was convinced that the work of visiting nurses was incompatible with enclosure and was determined that his Sisters should not become religious in the monastic sense. ‘My daughters,’ he said, ‘you are not nuns... for whoever says the word nun says cloister and the Sisters should go everywhere.’ He enlisted simple country girls with a basic education, clothed them in grey-blue rough gowns and handed them over to his associate Mlle. le Gras for practical nursing training. The girls were instructed to obey the doctors but also to watch and learn, so that they could be of use when no doctor was within call. They were to be willing and ready helpers, able to go anywhere and do any thing. In 1639 they took over the nursing of a hospital in Angers. In 1642 the first four Sisters took vows, which were to be renewed annually. In 1654, at Sedan, they undertook for the first time the military nursing for which they were to become well-known.
When St. Vincent and Mlle. le Gras both died in 1660 there were 350 Sisters in seventy establishments in France and Poland and the Order continued to grow rapidly. However, the early 19th century saw its decline. While nursing education broadened generally, its own narrowed. Sisters were not allowed to be present during child birth or at gynaecological examinations and they were forbidden to nurse venereal cases or take full charge of men patients. For these reasons, they were not suited to the demands of general hospital work.
The early hospitals in England, as in the rest of Europe, were religious foundations. In 936, Athelstan established a hospital in York, nursed by eight Sisters. Archbishop Lanfranc opened two hospitals in Canterbury in the 11th century. In 1101, Queen Mathilda founded St. Giles in the Fields for lepers, served by Poor Clares, and, in 1148, St. Katharine’s, where noblewomen undertook nursing duties, was founded. St. Bartholomew’s – nowadays known as Barts – was founded in 1123, the Holy Cross, Winchester, in 1132 and in 1215 St. Thomas’s, founded as the infirmary of the Priory of St. Mary Overie, became a separate hospital. Brothers and Sisters of the Augustinian Order nursed at Bart’s and St. Thomas’s.
By the time of the Reformation, the care of patients at St. Thomas’s had fallen to an extremely low standard. In 1536, the parishioners complained that a woman in child birth was turned away to die at the church door; that infant baptism was refused until the Master received half a noble; that religious services were not held; that the Master kept a concubine within the hospital; and that he was in the habit of selling church plate and claiming it had been stolen. But any care was better than none. England had no secular nursing orders and no public hospital system so, with the dissolution of the monasteries in the 1530s, the plight of the sick poor became desperate. St. Bartholomew’s, however, was reconstituted by Henry VIII in 1544, and in 1547 the mayor and aldermen of the City of London petitioned Edward VI for leave to take over St. Thomas’s, St. Bartholomew’s, Bethlehem and other lesser institutions.
Stripped of its religious elements of loving care and self-sacrificing duty, nursing was revealed as little more than domestic work. The matron was in charge of all the women in the hospital and was responsible for seeing ‘that the said washers and nurses of this howse be alwaies well occupied and not idle’, but it was not felt necessary that she should have any nursing experience and her duties were mainly concerned with housekeeping : ‘You shal also in every quarter of the yeare examine the inventorie which shal be delivered unto you, of the implements of the howse; as of beddes, bolsters, mattrasses, blanquets, coverlets, shets, pallads, shirts, hosen, and such other.’ Nurses were instructed: ‘Ye shall also faithfully and charitably serve and help the poor in all their griefs and diseases as well as by keeping them sweet and clean as in giving them their meats and drinks after the most honest and comfortable manner.’ Their duties were to keep the wards and the patients clean, to distribute food and drink, and to administer any medicines and special food ordered by the doctor.
The monastic term Sister was retained and applied to the nurse in charge of a ward. Sometimes Sisters were appointed from among the nurses or attendants, sometimes from the upper domestic classes outside. At St. Bartholomew’s, each Sister had sole charge of nine or ten patients and was expected to use her free time to spin. In 1550, twenty-one pairs of sheets were delivered to the matron, cut from cloth woven and spun by the Sisters. Earliest staffing lists also include a ‘foole’ or ‘innocent’, presumably employed to keep the Sisters amused. A cosy picture emerges of the earliest lay nurses serenely weaving, laughing at the antics of the fool, and stopping occasionally to comfort a patient, shoo the hens into the yard or consume a substantial meal. Unfortunately this happy picture is marred by the evidence of the surviving hospital records. At St. Thomas’s the matron was brought before the court three times from 1572 to 1580 for drunkenness. In 1559, the matron of St. Bartholomew’s was forbidden to sell ale in her house. In 1563, a St. Thomas’s Sister was reported by the matron as ‘she wolde not do her dutie in the office but ronne to the taverne.’ In 1650, a Sister at Bart’s was rebuked for entertaining men all night and letting them play cards in her ward; six years later three Sisters who had disturbed patients by fighting were dismissed. The nursing itself was probably quite adequate though, and the matron of St. Bartholomew’s, for example, distinguished herself during the plague of l665, when some of the physicians had fled, and was commended and rewarded by the governors.
With the secularization of nursing, however, ladies almost ceased to regard the sick poor in hospitals as worthy objects of Christian charity, though nursing, and even a little surgery, continued to be numbered among the domestic arts. Women collected recipes for medicines as eagerly as those for potting meat, and wealthier ladies accepted responsibility for the health of their households and their less fortunate neighbours as one of their domestic duties. The diary of Lady Hoby (1599-1605) contains many entries like the following: ‘After I praied, then I dined, then I walked and did see a sicke man,’ and, ‘I dressed the hand of one of the servants that was verie sore Cutte.’ Lady Mildmay (died 1620) recorded in her journal: ‘Also every day I spent some time in the Herball and books of phisicking, and in ministering to one or other by directions of the best phisitions of myne acquaintance.’
In the 18th century, wealthy British philanthropists set an example to the rest of the world by throwing themselves into an orgy of hospital building: the London opened in 1740; the Middlesex in 1745; the Westminster in 1719; St. George’s in 1728; and Guy’s in 1725. Outside London, Manchester Royal Infirmary opened in 1753; Liverpool Royal Infirmary in 1749; Leeds General Infirmary in l767; and Edinburgh Royal Infirmary in 1729. Towards the end of the century, public fever hospitals were set up, and, in a first glimmering of organized sanitation and preventative medicine, whitewash was applied to hospital walls. Iron bedsteads replaced bug-infested wooden ones. The forceful criticisms of John Howard, a prison reformer who also investigated hospitals, stung many hospital managements in to spring-cleaning. Yet, during this period, the status of nurses and the standard of nursing actually declined.
The London Hospital opened with a man and wife to act as caretakers and look after the patients. A nurse was not appointed until a year or two later when it was decided that ‘Squire be contracted with by the Chairman of the Committee as Nurse for the Women’s wards at the rate of £14 a year.’ A night nurse was appointed at £9, but when both nurses became resident in 1743, their salaries were reduced to £6 and £4 respectively. The nurses slept off the wards and the watches (night nurses) in the attic. Day duty began at 6 am in summer and 7 am in winter and lasted until supper at 10pm. Nurses had to be in bed by 11 pm, had no holidays, no days off and no pension. In 1756, the list of their duties included the following: ‘To make the beds of the officers and servants, to clean the rooms, passages and stairs and the Court and Committee rooms.’ Records of most hospitals of the time report, with dreary regularity, nurses rebuked or dismissed for drinking, insolence, lack of discipline, absenteeism, thieving, or soliciting payment from the patients. One visitor recorded seeing an in-coming patient stopped at the door by a loud–mouthed virago – the Sister – who demanded her fee before he could enter.
The nurses seldom wore uniform, usually cooked their own food and ate it in the ward kitchens or sculleries. Their hours were long, their accommodation inadequate and insanitary, and night nurses often had to sleep in lobbies next to the racket of the wards. Most of the actual nursing was done by medical students. It was almost impossible to get respectable women to work in such conditions. One doctor reported, ‘We always take them without a character because no respectable woman would take such work.’ Another wrote, ‘I know that a respectable woman was declined the other day, as being too good for the situation. The only conditions that are made are... that they are not confirmed drunkards... In general they are not educated at all.’ The London Hospital decided to appoint only women who could read and write, but was forced to compromise when insufficient numbers of suitable candidates presented themselves. Instead, the hospital ordered ‘that only those nurses who could read and write were to administer medicine.’ In 1844 the Board of Leeds Infirmary rejected a proposal that ‘no nurse be engaged in the domestic duties of the House’. Guy’s finally relieved nurses of scrubbing floors as late as 1857, but ordered that, as a consequence, each nurse was to care for twice as many patients . Standards were not uniformly bad. Edinburgh Royal Infirmary maintained a reasonable level of nursing care and operated an excellent set of nursing regulations. Although formally untrained , some Sisters who worked for years on the same ward under the same physician picked up a useful amount of practical skill. In 1885, Sir James Paget spoke in their defence: ‘It is true that even fifty years ago there were some excellent nurses, especially among the Sisters on the medical wards, where everything was more gentle and orderly than in the surgical. They had none of the modern art: they could not have kept a chart or skilfully taken a temperature, but they had an admirable sagacity and a sort of rough practical knowledge which were nearly as good as an acquired skill.’ A correspondent to The Times in 1857 wrote with more understanding of the nurses’ position than was then usual, ‘Hospital nurses have been much abused – they have their faults, but most of them are due to the want of proper treatment. Lectured by committees, preached at by chaplains, scowled on by treasurers and stewards, scolded by matrons, sworn at by surgeons, bullied by dressers, grumbled at and abused by patients, insulted if old and ill-favoured, talked flippantly to if middle-aged and good humoured, tempted and seduced if young and well-looking – they are what any woman might be under the same circumstances.’
Efforts to improve the quality of nursing were generally limited to pious hopes, stern injunctions and envious glances across the English Channel to the religious orders who at least gave loving care ( though by then most of the nursing in the major public institutions was done by lay attendants, as much practical nursing was banned to the Sisters on the grounds of impropriety). It did not seem to have occurred to hospital managers and doctors that they got what they paid for and that respectable, even educated, women might be drawn to nursing by higher salaries and improved conditions. Unable to visualize good nursing outside the confines of a sisterhood, all they could do was to vainly ask, ‘Where are our Sisters of Charity?’
The conditions in the great voluntary hospitals affected only a minority of the sick. The rich employed private nurses at home, though as most of these were of the Mrs. Gamp stamp vividly described by Charles Dickens, the quality of care was no better than in hospital. The remainder of the population stayed at home for as long as their family and friends could cope with them. Most who were forced to seek institutional care ended up in the workhouse infirmaries, either because there was no voluntary hospital in their area or because the voluntary hospitals would not accept them. When the great union workhouses were built following the Poor Law Amendment Act of 1834, they undertook to provide medical attention and in-patient facilities to all who were both destitute and in need of them. But, such was the deterrent effect of the grim buildings, the penal restrictions and the comfortless diet and accommodation, that the able-bodied preferred almost any fate to incarceration within their walls. Most workhouse inmates were incapacitated in some way – by age or youth, chronic illness or disability, pregnancy or idiocy, drunkenness or madness. As little or no distinction was made between the grades of inmates, the sick had to face the same punishing regime as the so-called idle or evil. Sadly, it was only too easy for a respectable and hard-working man or woman to end their days in the workhouse simply because they had nowhere else to go.
Some workhouses were, within the restrictions of the Act, admirable institutions. In 1841, the retiring Board of Guardians of Manchester Workhouse described with justifiable pride their ‘ample and convenient’ sick wards, a lying-in ward, and the ‘commodious and conveniently situated’ surgery. Unfortunately, in most cases, the guardians were uninterested and neglectful, or even corrupt, while the matron and master could be at best uncaring and at worst, unkind to the point of cruelty. The outside world, supposing all inmates to be getting no more than they deserved, were pleased by a system which, they believed, kept the cost down. Only when the early lady visitors and the more sensitive medical officers and chaplains started investigating and, shocked, published what they discovered, did the real picture emerge.
Dr. Joseph Rogers, medical officer at the Strand Workhouse, one of the worst in London, described conditions as he first found them in 1855. The Guardians received £400 a year from carpet beating which the inmates carried out just outside the male wards, so that the noise deprived the sick of sleep and the dust made it impossible to open the windows. The ‘foul’ ward was separated from the tinker’s shop only by an eight-foot partition. The female insane ward was just under the lying-in ward. But the worst scandal was the nursing. ‘There was no paid nurse. Such nursing as we had and continued to have for the first nine years I was there, was performed by more or less infirm paupers, with the occasional aid of some strong woman who had been admitted temporarily and was on pass.’ In the 1850s, there were only seventy paid nurses (all untrained) in the whole of London, compared with 500 pauper nurses of whom half were over 50, a quarter over 60, many over 70 and some over 80. ‘The responsible duties they had to perform were remunerated by an amended dietary and a pint of beer,’ Dr. Rogers wrote. He continued ‘... I had not been the medical officer for many months before I found that my pauper nurses were frequently under the influence of drink, and that, too, in the forenoon. On inquiring, I heard to my surprise that the master was in the habit of giving out the stimulants at 7 am, and, as many of the inmates sold their allowances, the nurses had become partly or wholly intoxicated when I reached the House in the morning.’ Not the least of the deterrents to good medical care was the fact that the doctors had to pay for medicines and drugs out of their own salaries – which, in Dr. Rogers’s case, amounted to £50 a year.
Louisa Twining, who devoted her life to the cause of workhouse reform, had her interest in infirmaries aroused by a visit to an old crossing sweeper in St. Giles Workhouse in 1856. ‘He was in the basement ward, nearly dark, and with a stone floor; beds, sheets, and shirts were all equally grey with dirt... The sick in the so-called infirmary, a miserable building, long since destroyed, were indeed a sad sight, with their wretched pauper nurses in black caps and workhouse dress. One poor young man there, who had lain on a miserable flock bed for fourteen years with a spine complaint, was blind, and his case would have moved a heart of stone; yet no alleviation of food or comforts were ever granted him.’ In 1858 she outlined her findings in a letter to The Times and appealed for improvements in the nursing. ‘There is generally one nurse and a helper to each ward, sometimes containing twenty or thirty patients. The nurse sleeps in it and lives in it, whether the patients are men or women, in cases under my own knowledge. She may be said to be at work almost equally during the twenty–four hours for who else is to tend the sick and dying sufferers by night?’ In the wards, ‘Here are all those, in short, both young and old... who have no homes where they can be nursed. I have known such sufferers who never left their beds for years, I have known them tended at their deaths by drunken nurses. The women who are set over wards full of helpless sufferers drink whenever they can obtain the means, for they came not to this, the lowest office which a worn out woman can fill, till all other chances of subsistence are gone.’
Frances Power Cobbe, who was particularly interested in improving conditions for ‘destitute incurables’, started workhouse visiting in 1859, ‘and this is what I saw. The sick lay on wretched beds, fit only for able-bodied tramps, and were nursed mainly by old pauper women of the very lowest class. The infirm wards were very frequently placed in the worst possible positions. I remember one (in London) which resounded all day long with din from the iron-foundry just beneath.... On one occasion I visited an enormous workhouse in a provincial town where there were nearly 500 sick and infirm patients. The Matron told me she had but lately been appointed to her post. I said, “It is a tremendously heavy charge for you, especially with only these pauper nurses. No doubt you have gone through a course of Hospital training, and know how to direct everything?” “O, dear No! Madam!” replied the lady with a toss of her cap-strings; “I never nursed anybody I can assure you, except my ’usband , before I came here. It was misfortune brought me to this!”’
Conditions in American hospitals rivalled those in Britain. Most big cities had almshouses which, like British workhouses, included infirmaries for the sick poor, and where the nursing, such as it was, was undertaken by other inmates. The origins of Bellevue Hospital, New York, lay in a small hospital built by the West India Company in 1658. In 1736, the new building was called the ‘Publick Workhouse and House of Correction of New York’ and by 1816 it contained almshouse quarters, a penitentiary and wards for the sick and insane. There was shocking overcrowding, insanitary conditions, and constant epidemics, while the doctors were cruelly overworked and the nurses detailed from the prison. In 1837, a committee of investigation reported filth, no ventilation, no clothing, patients with high fever lying naked under coarse blankets, jail fever rife, overcrowding, no supplies, putrefaction and vermin. As a result of the report, male and female prisoners were removed and smallpox cases and the insane were taken to separate infirmaries.
Blockley Hospital, Philadelphia, started life as an almshouse in 1731. An investigation in 1793 found shocking abuses and spoke of ‘an abandoned, profligate set of nurses and attendants’. All work, including the nursing, was done by the inmates. In the cholera epidemic of 1832, the attendants demanded and received more wages which they at once spent on drink, then fought each other or lay in a drunken stupor in the wards. Sisters of Charity were summoned from Emmitsburgh. They restored order, but refused to stay. In 1856, a further report revealed scandalous conditions.
Not all hospitals were as bad. The Pennsylvania Hospital, which opened in 1751 and was the first in the United States devoted solely to the curative care of the sick, had a better history, and its records mention ‘experienced and trustworthy persons’ who did the nursing. New York Hospital, which was granted its charter in 1771, was, like the Pennsylvania, a wealthy foundation and probably employed a superior class of attendants. It was these standards that the reformers were determined to achieve for all.
2. Where are Our Sisters of Charity?
By the early 19th century a number of compassionate and humanitarian ladies and gentlemen had woken up to the fact that care for the poor and the sick left much to be desired.
Inspired with charitable zeal, they led a crusade to alleviate the lot of these, the least of God’s creatures. At the same time the germ of a revolutionary idea was born in medical minds. Concerned at the shocking state of nursing and hospital conditions generally, it occurred to doctors that good nursing might actually contribute to the cure of patients. These two trends led eventually to the establishment of the nursing profession.
The first attempt to train hospital attendants was made by Dr. Valentine Seaman of the New York Hospital. In 1798, he organized a course of twenty-four lectures which included the outlines of anatomy, physiology and child care, the course being run in connection with the maternity department. But most early attempts at nursing reform centred naturally on the idea of nursing sisterhoods. In Germany the deaconess movement had never wholly died out and after several false starts elsewhere it was successfully revived at Kaiserswerth on the Rhine. The village pastor, Theodor Fliedner, had been impressed, during his travels through Europe, with the need for better nurses. ‘Would not our young Christian women be able and willing to do Christian nursing?’ he wrote. ‘... Ought we to delay in bringing back consecrated women into the service of the Lord?’
Fliedner’s hospital opened in 1836. The deaconesses, with Pastor Fliedner’s wife, Friederike, as superintendent, led simple and frugal lives, undertaking the cooking and cleaning as well as the nursing of the sick poor both in the hospital and at home. They were given theoretical and clinical instruction and studied for the state examination in pharmacy. A probationary period was introduced, and after five years of service the deaconesses were free to leave and marry. The cheerful loving spirit which inspired their work impressed many visitors, including the British reformer Elizabeth Fry on her visit in 1840.
Gradually the work and influence of the deaconesses expanded. They were invited to take over the nursing in other hospitals. New motherhouses were established and in 1849 Pastor Fliedner took a party of deaconesses across the Atlantic to Pittsburgh to start a house there.
Visitors came to Germany from many other countries to learn from Fliedner’s example. Among them was Florence Nightingale, who spent three months there in 1851. Looking back on her time at Kaiserswerth, she wrote: ‘The nursing there was nil, the hygiene horrible. The hospital was certainly the worst part of Kaiserswerth.’ However, Miss Nightingale continued: ‘But never have I met with a higher tone, a purer devotion than there. There was no neglect. It was the more remarkable because many of the Deaconesses had been only peasants – none were gentlewomen (when I was there).’ Although far from ideal, the nursing at Kaiserswerth was far in advance of all other nursing at the time. The deaconesses served bravely and devotedly in epidemics and wars – they worked in sixty military hospitals in the Franco-Prussian War.
During the latter part of the 19th century the institution went into a decline. The freshness and reforming zeal melted away. Pastor Fliedner had placed a great emphasis on the movement’s independence from church or state control, but gradually the pastors took over the control of the nurses from the matrons and restricted their intellectual freedom and spheres of work. The need to earn money meant that nurses were sent out to take on hospital work with little or no training, probationers were accepted at younger and younger ages, and the deaconesses were often cruelly overworked.
The movement’s influence was widespread, however. In England the cry went up, ‘Let all serious Christians join, and found an order of women like the Sisters of Charity.’ Good nurses must be ‘animated by religion,’ the men insisted, ‘science and mere humanity cannot be relied on’ – though no one seems to have suggested that doctors should be similarly hemmed in by a religious Rule. Elizabeth Fry, fresh from Kaiserswerth, was the first to answer the appeal, though the secular nature of her Institute of Nursing, founded in 1840, roused suspicions in some clerical quarters. Her Sisters were carefully chosen, mainly from the higher domestic or small farm and trading classes, and they had to be able to read and write. They received a limited practical training at Guy’s Hospital in London, wore plain clothes, were maintained by the Institute and were forbidden to accept money and gifts. They were employed mainly in private nursing, but, between jobs, they lived in the Home and undertook nursing the poor. The Institute had limited influence – by 1857 only ninety nurses had been trained but it proved that such an experiment could work. It was also popular with its customers. William Thackeray wrote to the Lady Superintendent in 1860, ‘I have the pleasure of sending you ten guineas for the five weeks service of the excellent nurse I had from your institution, and beg it to accept the other five pounds.’
A similar body to Mrs. Fry’s Institute was founded in Philadelphia in 1839. There, a group of young ladies banded together to organize the Nurse Society for the purpose of ‘providing, sustaining, and causing to be instructed as far as possible, pious and prudent women’ to nurse poor females during and after child birth. The nurses were given lectures, and practised on a manikin. After attending six cases satisfactorily they were awarded a certificate and could work as home nurses. In 1850 a Home and School were opened and teaching improved, even though the course’s duration was not extended to a year until 1897.
The first Church of England Sisterhood, the Park Village Community, opened under Dr. Pusey’s guidance in 1845. The Sisters of Mercy had no hospital training and devoted themselves chiefly to welfare visits to the sick and poor. A similar group, also known as the Sisters of Mercy, was founded by Miss Sellon in Devonport in 1848. In the beginning, they also had no hospital experience but worked energetically through several cholera epidemics. By 1866 the two communities had merged.