9,59 €
Mehr erfahren.
- Herausgeber: Salt
- Kategorie: Fachliteratur
- Sprache: Englisch
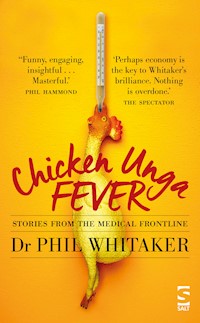
Is it a new strain of bird flu? A strange neurological condition characterised by an irresistible urge to eat poultry-based foods? No, Chicken Unga Fever is a collection of the very best of Dr Phil Whitaker's 'Health Matters' columns – much loved by readers of the New Statesman magazine, where they have appeared fortnightly for the past five years. Funny, touching, informative, and often profoundly poignant, Chicken Unga Fever paints a vivid portrait of the working life of a West Country GP. From the overweight anorexic to the rash-stricken Kylie fan, from the curious case of Top-of-the-Ear Disease to the equally mysterious Pool Toe, Phil's humanely written vignettes illuminate every aspect of modern medicine, and cast light on the state of our beleaguered NHS and the glorious variety of people it serves. This collection will delight both interested lay readers and those who work in healthcare. And, to cap it all, somewhere in these pages the true nature of Chicken Unga Fever will be revealed.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Veröffentlichungsjahr: 2018
Ähnliche
CHICKEN UNGA FEVER
by
DR PHIL WHITAKER
SYNOPSIS
Is it a new strain of bird flu? A strange neurological condition characterised by an irresistible urge to eat poultry-based foods?
No,Chicken Unga Feveris a collection of the very best of Dr Phil Whitaker’s ‘Health Matters’ columns – much loved by readers of theNew Statesmanmagazine, where they have appeared fortnightly for the past five years.
Funny, touching, informative, and often profoundly poignant,Chicken Unga Feverpaints a vivid portrait of the working life of a West Country GP.
From the overweight anorexic to the rash-stricken Kylie fan, from the curious case of Top-of-the-Ear Disease to the equally mysterious Pool Toe, Phil’s humanely written vignettes illuminate every aspect of modern medicine, and cast light on the state of our beleaguered NHS and the glorious variety of people it serves.
This collection will delight both interested lay readers and those who work in healthcare. And, to cap it all, somewhere in these pages the true nature ofChicken Unga Feverwill be revealed.
PRAISE FOR PREVIOUS WORK
‘Funny, engaging, insightful … Masterful.’ —PHIL HAMMOND
‘Perhaps economy is key to Whitaker’s brilliance. Nothing is overdone.’ —The Spectator
Chicken Unga Fever
phil whitakeris a writer and practising doctor. His ‘Health Matters’ column appears fortnightly in theNew Statesman. As well as his writing on medical matters, he is the award-winning author of six novels, most recentlySister Sebastian’s Library(2016) andYou(2018), both published by Salt.
Published by Salt Publishing Ltd
12 Norwich Road, Cromer, Norfolk NR27 0AX
All rights reserved
Copyright © Phil Whitaker,2018
The right ofPhil Whitakerto be identified as the author of this work has been asserted by him in accordance with Section 77 of the Copyright, Designs and Patents Act 1988.
This book is in copyright. Subject to statutory exception and to provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of Salt Publishing.
Salt Publishing 2018
Created by Salt Publishing Ltd
This book is sold subject to the conditions that it shall not, by way of trade or otherwise, be lent, re-sold, hired out,or otherwise circulated without the publisher’s prior consent in any form of binding or cover other than that in which it is published and without a similar condition including this condition being imposed on the subsequent purchaser.
ISBN 978-1-78463-155-0 electronic
For my sister, Sue, and my brother, Mike
The articles in this collection first appeared as ‘Health Matters’ columns in the New Statesman, and are reproduced with kind permission. I am very grateful to the editor, Jason Cowley, for commissioning the column back in 2013, and to the arts editor, Kate Mossman, for shepherding the column over the ensuing five years with good humour and an unfailingly keen editorial eye.
IN HOURS
Buzzers and meeters
GPs can bedivided into two distinct groups: ‘buzzers’ and ‘meeters’. The former stay put in their consulting rooms, employing a variety of devices such as buzzers or intercoms to call their patients through. ‘Meeters’, on the other hand, walk along to collect each patient from the waiting room in person.
We are ‘meeters’ in my practice. I like the brief interlude of physical activity, which helps clear the mind in readiness for the next consultation. Equally important is the opportunity to begin putting patients at ease, greeting them with a smile and making small talk as we walk the corridor together. The rapport-building helps the consultation get off to a good start, rather than the patient arriving ‘cold’ at my consulting room door.
‘Meeting’ also provides valuable advance information. Musculoskeletal problems are the most obvious: back pain is instantly recognisable from the way someone gets out of their chair. Hip, knee, and ankle pathology produce characteristic gaits. The severity of respiratory problems can be gauged by the degree of breathlessness with exertion. Eye contact, body posture, and facial expression when crossing the waiting room give clues as to the patient’s state of mind – depression, acute anxiety, or frustration and anger all transmit themselves clearly, and one can prepare oneself for the likely tenor of the consultation.
‘Waiting room diagnoses’ are sometimes memorable, as in the case of Simon, a 45-year-old I went to collect a little while ago. His notes had already revealed him to be an infrequent attender, making it more likely that he would be coming about something significant. When I called his name, his wife got up to accompany him – often a sign of high levels of concern; sometimes indicative of a reluctant male being frogmarched to the doctor by a spouse who’s decided enough-is-enough. Both their faces were taut with worry. By the time Simon reached me I had the full picture. He was noticeably out of breath after walking just those dozen yards. A glance told me the reason: he was strikingly pale, a sign of gross anaemia. The amount of the oxygen-carrying red pigment (haemoglobin) in his blood was very low.
As we made our way along the corridor, I thought ahead. There are several types of anaemia, but by far the commonest is iron-deficiency. This arises either because of inadequate iron in the diet (rare in the UK), failure to absorb iron from food (coeliac disease is the most frequent culprit), or – most often – sustained loss of blood. Women of reproductive age quite commonly become anaemic from excessive menstrual bleeding. In a male of Simon’s age, however, a marked iron-deficiency anaemia is unusual and worrying – it is a typical presentation of gastrointestinal cancer, an otherwise unsuspected tumour leaking small amounts of blood into the bowel day after day until haemoglobin levels fall sufficient to cause symptoms. By the time Simon, his wife, and I had seated ourselves in my consulting room, I was braced for a delicate discussion. And once Simon had admitted that he’d been keeping quiet about periodic blood in his stools for some months, the path ahead was clear.
Since 2000, GPs have been able to refer suspected cancer cases under the ‘two week wait’ (2WW) rule, ensuring that investigations are undertaken speedily. The only proviso is the patient must be made aware that cancer is a distinct possibility, both to ensure they attend the urgent appointment slot and to prepare the ground for any discussion that may be needed at the hospital. In Simon’s case, he required direct inspection of his lower digestive tract. Colonoscopy is a fairly unpleasant procedure, not least because endoscopic inspection of the lower bowel is only possible after a purge with powerful laxatives. Simon was going to have to spend a couple of days staying very close to a loo.
There was a lot to explain and prepare him for, not least the fact that, were a bowel cancer to be discovered, there was a reasonable prospect of cure. Survival rates in the UK have more than doubled over the past thirty years, with at least half of patients being disease-free after ten years, rising to a 90% cure rate if the tumour is detected at an early stage. Even though the outlook is far from gloomy, and even though the 2WW rule has dramatically shortened the time spent in limbo waiting for results, the uncertainty can be very difficult to cope with. Simon and his wife were understandably anxious, but I was impressed by the phlegmatic way in which they greeted each new piece of information, all the more so because they have a young family. Simon’s comments stayed with me: about how they would remain calm, and square up to whatever they needed to deal with.
A couple of weeks later, a fax brought the good news: Simon was clear of cancer. The bleeding was from an unusual blood vessel anomaly in the bowel wall, readily treatable by laser. He and his wife made an appointment a few days later to discuss the next steps. It was a genuine pleasure to see the smiles on their faces as they came across the waiting room towards me, a sight I would have missed were I a ‘buzzer’ rather than a ‘greeter’.
Bites
Erica was atthe end of her tether. ‘I’ve had the council round several times, they’ve fumigated the whole place twice, and still I’m getting bitten.’
I peered at her lower legs. There were scattered red lumps, and lots of scratch marks. The environmental health department’s pest control officer, having exhausted his insecticidal repertoire, had apparently sent Erica along to me.
The commonest reason for someone being eaten alive in their own home is the death of a cat. Fleas live in carpets, hopping on to the resident pet when in need of food. As long as Tiddles remains hale and hearty, humans are bitten only sporadically. But a few weeks after a feline departure, the now-starving fleas start to feast on the grieving owner, leaping on to their legs as they walk past. Erica, however, denied any previous pet ownership. And flea bites are typically clustered around the ankles and lower shins, whereas Erica said she was affected all over.
‘May I?’ I asked, taking her hand. I scrutinised the skin of her wrist, and the web spaces between her fingers. Infestation with scabies is surprisingly common, and those are favourite locations for the mites. There was nothing to see, though, and nor did any of the red lumps on her forearms display the hairline tracks that scabies mites make when burrowing through the skin.
It wasn’t just Erica’s hands that were spared involvement. While most of her torso was scratched and bump-strewn, her mid-back was blemish-free. This pattern suggests something called prurigo. Incessant scratching of normal skin results in the development of raised red prurigo lumps, which can easily be mistaken for insect bites. The area between the shoulder-blades remains unaffected, though, because it is impossible concertedly to scratch there.
‘I think we’d better check some blood tests,’ I told Erica. There’s a host of medical conditions that can cause generalised itch, from iron-deficiency through to underactive thyroid. I gave her prescription for a large bottle of Eurax to be going on with – a fantastic lotion which will suppress itch whatever the cause.
A week later and all the tests were back and normal. Erica was back, too. And this time she’d brought specimens of the offending insects to show me.
‘There!’ she announced, handing me a little glass jar. I held it up to the light. Inside were a couple of wisps of dark fluff, and some indeterminate bits of debris such as might be found on anyone’s floor. Not even tapping the contents on to my palm for a sift-through could produce any evidence of life forms.
Something about the little glass jar rang a bell. The ‘matchbox sign’ describes the tendency of a particular sort of patient to bring spurious evidence in a small container to show the doctor. I looked at Erica afresh. In her late 50s, a trifle eccentric but absolutely no history or indication of any mental or physical illness. I wondered if she might represent a case of Ekbom’s syndrome, or delusional parasitosis.
Delusional parasitosis is a fixed but false belief that one is infested with some sort of parasite, usually an insect. In all other respects, the patient is functioning entirely normally, so presents a convincing account of their troubles to pest control personnel, doctors and veterinarians. As in Erica’s case, only when all usual avenues have been exhausted does the truth begin to emerge. A big problem with Ekbom’s is the characteristic refusal of the sufferer to accept that they are suffering from a mental illness – they’re absolutely convinced they’re infested. Antipsychotic drugs, usually employed in schizophrenia, can be very effective, but most Ekbom’s patients reject them out of hand, and indeed can become quite irate at the suggestion that there’s anything wrong with their mind.
‘I’d like you to try these tablets,’ I told Erica. ‘If you read the leaflet you’ll find they’re usually used to treat schizophrenia, but bizarrely enough they’re also quite likely to reduce the itch and the rash you’re experiencing.’ I smiled, hoping she wouldn’t probe my explanation. I wasn’t lying as such; just being very careful which bits of the picture I painted.
She returned a month later and, to my relief, had taken the tablets. ‘It’s amazing,’ she told me, ‘it’s completely better.’ She showed me a few areas of pristine skin and we exchanged words of relief that her ordeal was at an end. Then she fell silent for a few moments. When she spoke again her voice was lowered, embarrassed. ‘Doctor, was I psychotic?’
‘Well, yes,’ I told her, and explained about Ekbom’s syndrome. With recovery had come full insight, and she recounted, with something akin to awe, how she now looked at the specimens she’d collected and could see they were nothing but fluff, but could clearly remember perceiving them as dead insects at the time. And the persistent sensation of things crawling over her skin had been utterly real to her.
Ekbom’s is fascinating and relatively rare – I doubt I’ll see another case. It strikes me that pest control officers, given the nature of their job, must encounter it more often. I imagine they have a cut-off – perhaps two failed fumigations, or when the homeowner starts to present them with bits of debris in a matchbox – when they suggest that a doctor might be better placed to help with this particular infestation.
Needles and hay
According to oneadage, general practice is like looking for a needle in a haystack. The needle is ‘proper pathology’ – the stuff you’ll find in medical textbooks. The haystack is the bewildering array of nebulous complaints that people bring to their doctors: aches, fatigue, palpitations, nausea, rashes, dizziness, numbness ... the list goes on. These symptoms could all signify something serious, yet much of the time they don’t amount to anything that could be given a diagnostic label.
I don’t agree with the adage, though. It implies that a GP’s raison d’être is to find needles, whereas helping people make sense of their particular haystack is just as important. Nevertheless, every now and then we will come across a sharp-pointed steel sliver. We need to be continuously alert to spot it before it pricks our metaphorical fingers.
Tim was one of my registrars – a younger doctor I was training. Cheryl was a patient he’d seen on several occasions. She had just turned forty, yet she had markedly raised blood pressure and, try as he might, Tim couldn’t get it under control. I joined him for the next consultation – he wanted advice about what to add to the cocktail of medications Cheryl was already taking – and the longer it went on the more intrigued I became.
It was mid-October and, even though we’d had a fine English summer, most people were once again pale. Not so Cheryl. Of course, sun is never more than an EasyJet flight away, but on closer inspection there was an unusual grey tinge to Cheryl’s tan. I scrutinised her more carefully. Her forearms, visible below rolled-up sleeves, were hirsute. Conversely, her head hair was subtly thinning in a ‘male pattern’ – at crown and at temples. And even though it fitted with her cheerful manner, her facial complexion was distinctly ruddy. As Tim closed the consultation I asked Cheryl if she would mind undertaking some tests.
The pituitary gland is a pea-sized organ buried deep within the brain. It releases a variety of hormones that orchestrate our growth, metabolism, and reproduction. When a benign tumour (adenoma) arises, its cells pump out far too much of their particular hormone. One, ACTH (adrenocorticotropic hormone), stimulates the production of steroids in the adrenal glands. An ACTH-secreting adenoma sends the adrenals into overdrive, the excess steroids eventually wrecking havoc – thinning bones, provoking cataracts, elevating blood pressure, precipitating diabetes, and causing heart disease – something called Cushing’s Disease.
Cushing’s Disease affects just ten in every million people in the UK each year, so the majority of doctors will never encounter a case in their entire working lives. The secondary conditions it presents with – high blood pressure, diabetes, and so on – are, on the other hand, as common as muck. Rarely do they have an underlying cause. All this means that Cushing’s is extremely difficult to diagnose. What had rung a bell for me was a fascinating fact I’d learned decades before at medical school. As well as driving the adrenals, ACTH has the side-effect of stimulating pigment cells in the skin. People with Cushing’s Disease have unaccountable tans.
I explained my suspicions to Tim after Cheryl had left. He wasn’t convinced. Cheryl’s unusual tan could easily have been induced by a sun bed, or come from a bottle. And he hadn’t spotted the hair and facial signs that were also suggestive. Laboratory confirmation takes weeks. Finally, the biochemistry consultant rang to say, yes, Cushing’s it was. Most doctors get a thrill when they pull off a rare diagnosis. And most other doctors are slightly envious of a colleague who performs such a feat – the consultant wanted to hear the whole story of how I’d come to suspect it.
As for the doctor who has been sifting through the hay and who failed to spot the needle, it can be painful. Things look so neat and so obvious when viewed through the retrospectoscope. Of course it was Cushing’s: that explains why her blood pressure was so difficult to treat. It was a textbook case.
An experience like that could have undermined Tim’s confidence. As well as imparting factual knowledge, one of my roles as a trainer is to prepare my registrars to cope with the ups and downs of medical life. To that end, I told Tim the story of a GP who’d been consulted by a male patient with marriage-threatening snoring – another haystack symptom. For over a year the GP had tried in vain to help; even the Ear Nose & Throat specialists had eventually drawn a blank. In desperation, the patient was referred to a sleep clinic. There, a fresh pair of eyes took one look and diagnosed acromegaly, another vanishingly rare condition caused by a pituitary adenoma – this one secreting growth hormone, which enlarges the extremities, including the tongue and jaw, resulting in intractable snoring. The GP who’d failed to spot the (retrospectively) blindingly obvious diagnosis was me.
Both acromegaly and Cushing’s Disease can be arrested by surgery to remove the adenoma. For doctors involved in their diagnosis there are lessons to be learned. When we pick one out we should feel pleased but not proud. When we miss one we should evaluate our performance honestly, but we should not unduly run ourselves down. Occasional needles will always be fiendishly difficult to detect when buried amidst a shed-load of hay.
Section
According to medicalfolklore, most mental health crises occur on Friday afternoons. I’m not sure that’s actually the case, but I couldn’t help noticing it was exactly one minute past twelve on the day before the weekend when the call from the approved social worker was put through.
‘It’s about your patient, Maggie Halliwell,’ he explained. ‘I’m convening a section assessment. What time might you be available?’
Committal under a section of the Mental Health Act (MHA) is one of the most weighty responsibilities a doctor can have: admitting someone, against their will, to a psychiatric hospital, where they will be detained – potentially for months – while their condition is evaluated and/or treated. The deprivation of liberty, and the power to enforce treatment, is subject to numerous safeguards, beginning with the obligation that two independent doctors – one an experienced psychiatrist; the other, whenever possible, the patient’s own GP – recommend committal.