62,99 €
Mehr erfahren.
- Herausgeber: John Wiley & Sons
- Kategorie: Fachliteratur
- Sprache: Englisch
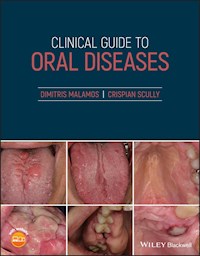
A quick reference and revision guide on the most common oral and perioral diseases seen in clinical practice Clinical Guide to Oral Diseases is a concise reference on the common diseases encountered in daily practice. Presenting a large selection of clinical cases, this user-friendly resource covers a range of oral and perioral lesions located in hard and soft tissues of the mouth and neck, as well as oral manifestations of various systemic diseases. Nearly 300 high-quality color images complement succinct descriptions of clinical cases seen in both community and hospital care settings. Divided into three parts, the text first covers oral lesions classified by their color, appearance, and symptomatology such as bleeding, disturbances of saliva, taste, and orofacial pain. Part two describes the most common oral lesions by location, including those in the buccal mucosae, floor of mouth, gingivae and jaws, lips, neck, palate, salivary glands, tongue, and teeth. The third part encompasses oral lesions that are normal variations or those common to specific age groups or associated with various clinical phenomena. * Provides nearly 300 high-quality clinical photos and relevant questions to help lead readers to the proper diagnosis of common oral diseases * Contains concise tables relevant to each chapter with a list of common oral lesions and conditions * Offers MCQs of varying levels of difficulty to help readers test their knowledge in Oral Medicine * Includes clinical flow charts according to the location and duration of oral lesions * Incorporates the ICD-10 Codes of oral lesions and diseases Clinical Guide to Oral Diseases is a valuable reference for general dental and medical practitioners, undergraduate dental students, and postgraduate trainees in oral and maxillofacial surgery, oral medicine, oral pathology, periodontology as well as general pathology, dermatology or head and neck oncology.
Sie lesen das E-Book in den Legimi-Apps auf:
Seitenzahl: 876
Veröffentlichungsjahr: 2021
Ähnliche
Table of Contents
Cover
Title Page
Copyright Page
Preface
Foreword
Acknowledgment
About the Companion Website
Section I
1 Bleeding
2 Blue and/or Black Lesions
3 Brown Lesions
4 Malodor
5 Muscle Deficits (Trismus/Paralysis)
6 Orofacial Pain
7 Red Lesions
8 Saliva Disturbances (Xerostomia/Sialorrhea)
9 Swellings (Diffuse/Lumps)
10 Taste Deficits
11 Ulcerations
12 Vesiculobullous Lesions
13 White Lesions
14 Yellow Lesions
Section II
15 Buccal Mucosa
16 Floor of the Mouth
17 Gingivae
18 Jaws
19 Lips
20 Neck
21 Palate
22 Salivary Glands (Minor/Major)
23 Teeth
23.1 Part A: Teeth Anomalies Related to their Number, Size, and Shape
23.2 Part B: Disorders of Teeth Structures
23.3 Part C: Diseases Affecting the Teeth's Components in Relation to the Adjacent Tissues
24 Tongue
Section III
25 Normal Variations
26 Oral Lesions According to Patient's Age
27 Clinical Tests, Signs and Phenomena
Abbreviations
Diagnostic Flow Charts According to the Location of Oral Lesions
Appendix: ICD‐10 Codes of Oral Diseases/Lesions
Index
End User License Agreement
List of Tables
Chapter 1
Table 1 Conditions related to oral bleeding.
Chapter 2
Table 2 The most common causes of blue and black lesions.
Chapter 3
Table 3 The most common oral brown lesions.
Chapter 4
Table 4 Common and important conditions associated with malodor
Chapter 5
Table 5 Common and important conditions related to muscle dysfunctions.
Chapter 6
Table 6 Common and important conditions in orofacial pain.
Chapter 7
Table 7 The common causes of oral red lesions.
Chapter 8
Table 8.1 Drooling and sialorrhea: Common and important conditions.
Table 8.2 Dryness: common and important conditions.
Chapter 9
Table 9 The most important causes of swellings and lumps.
Chapter 10
Table 10 The most important causes of taste changes.
Chapter 11
Table 11 Ulcers: Common and important causes.
Chapter 12
Table 12 Common and important vesiculobullous conditions.
Chapter 13
Table 13 Common and important conditions of white lesions.
Chapter 14
Table 14 Common and important conditions of yellow lesions.
Chapter 15
Table 15 Buccal mucosa: Common and important lesions.
Chapter 16
Table 16 Floor of the mouth: common and important lesions and conditions.
Chapter 17
Table 17 Gingivae lesions: common and important conditions.
Chapter 18
Table 18 Common and important conditions of occurring in the jaws.
Chapter 19
Table 19 Common and important conditions of the lips.
Chapter 20
Table 20 Neck: common and important lesions.
Chapter 21
Table 21 Palate lesions.
Chapter 22
Table 22 Common and important salivary gland lesions and diseases.
Chapter 23
Table 23 Teeth: common and important changes.
Chapter 24
Table 24 Common and important lesions of the tongue.
Chapter 25
Table 25 Normal oral variations according to location.
Chapter 26
Table 26 Common and important lesions according to patient's age.
Chapter 27
Table 27 Clinical tests, signs, and phenomena commonly seen in oral medicine ...
List of Illustrations
Chapter 1
Figure 1.0 Tongue hematoma in a woman with seizures.
Figure 1.1a
Figure 1.1b
Figure 1.2
Figure 1.3
Figure 1.4
Figure 1.5
Figure 1.6a
Figure 1.6b
Figure 1.7
Figure 1.8
Figure 1.9
Figure 1.10
Chapter 2
Figure 2.0a Blue lesion.
Figure 2.0b Black lesion.
Figure 2.1
Figure 2.2a
Figure 2.2b
Figure 2.3
Figure 2.4
Figure 2.5
Figure 2.6
Figure 2.7
Figure 2.8
Figure 2.9
Figure 2.10
Chapter 3
Figure 3.0a Brown discoloration of neck skin after radiation.
Figure 3.0b Hydroxyurea‐induced oral brown pigmentation.
Figure 3.1
Figure 3.2a
Figure 3.2b
Figure 3.3
Figure 3.4
Figure 3.5
Figure 3.6
Figure 3.7
Figure 3.8
Figure 3.9
Figure 3.10a
Figure 3.10b
Chapter 4
Figure 4.0a Halitosis from a patient with advanced oro‐nasal carcinoma.
Figure 4.0b Halitosis from a patient with a neglected mouth.
Figure 4.1
Figure 4.2
Figure 4.3
Figure 4.4
Figure 4.5
Figure 4.6
Figure 4.7
Figure 4.8
Figure 4.9
Figure 4.10
Chapter 5
Figure 5.0a Trismus.
Figure 5.0b Facial palsy.
Figure 5.1
Figure 5.2
Figure 5.3
Figure 5.4
Figure 5.5
Figure 5.6
Figure 5.7
Figure 5.8
Figure 5.9
Figure 5.10
Chapter 6
Figure 6.0 Pain from the ulcerated oral mucosa of a patient with graft‐versu...
Figure 6.1
Figure 6.2
Figure 6.3
Figure 6.4
Figure 6.5
Figure 6.6
Figure 6.7
Figure 6.8
Figure 6.9
Figure 6.10
Chapter 7
Figure 7.0 Erythematous candidiasis in the palate: induced by constant wear ...
Figure 7.1
Figure 7.2
Figure 7.3
Figure 7.4
Figure 7.5
Figure 7.6
Figure 7.7
Figure 7.8
Figure 7.9
Figure 7.10
Chapter 8
Figure 8.0a Increased saliva in a patient with graft versus host disease (Gv...
Figure 8.0b Xerostomia.
Figure 8.1
Figure 8.2
Figure 8.3
Figure 8.4
Figure 8.5
Figure 8.6
Figure 8.7
Figure 8.8
Figure 8.9
Figure 8.10
Chapter 9
Figure 9.0 Traumatic fibroma.
Figure 9.1
Figure 9.2a
Figure 9.2b
Figure 9.3
Figure 9.4
Figure 9.5
Figure 9.6
Figure 9.7
Figure 9.8
Figure 9.9
Figure 9.10
Chapter 10
Figure 10.0 Testing sour taste with drops of lemon.
Figure 10.1
Figure 10.2
Figure 10.3
Figure 10.4
Figure 10.5
Figure 10.6
Figure 10.7
Figure 10.8
Figure 10.9
Figure 10.10
Chapter 11
Figure 11.0 Traumatic tongue ulcer in a healing process.
Figure 11.1
Figure 11.2
Figure 11.3
Figure 11.4
Figure 11.5
Figure 11.6
Figure 11.7
Figure 11.8
Figure 11.9
Figure 11.10a
Figure 11.10b
Chapter 12
Figure 12.0 Intact bulla on the inner surface of the lower lip in a patient ...
Figure 12.1
Figure 12.2a
Figure 12.2b
Figure 12.3
Figure 12.4
Figure 12.5
Figure 12.6a
Figure 12.6b
Figure 12.7a
Figure 12.7b
Figure 12.8a
Figure 12.8b
Figure 12.9a
Figure 12.9b
Figure 12.10
Chapter 13
Figure 13.0 White plaque on the dorsum and lateral left margin of the tongue...
Figure 13.1
Figure 13.2
Figure 13.3
Figure 13.4
Figure 13.5
Figure 13.6
Figure 13.7
Figure 13.8
Figure 13.9
Figure 13.10
Chapter 14
Figure 14.0 Aphtha.
Figure 14.1
Figure 14.2a
Figure 14.2b
Figure 14.3
Figure 14.4
Figure 14.5
Figure 14.6
Figure 14.7
Figure 14.8
Figure 14.9
Figure 14.10
Chapter 15
Figure 15.0a Leukoedema.
Figure 15.0b Oral carcinoma.
Figure 15.1
Figure 15.2
Figure 15.3
Figure 15.4
Figure 15.5
Chapter 16
Figure 16.0 Trauma of the duct of the right sublingual gland.
Figure 16.1
Figure 16.2
Figure 16.3
Figure 16.4
Figure 16.5
Chapter 17
Figure 17.0 Materia alba on the anterior lower gingivae of a patient receivi...
Figure 17.1a
Figure 17.1b
Figure 17.2
Figure 17.3
Figure 17.4
Figure 17.5
Chapter 18
Figure 18.0a Enlargement of the mandible from an odontogenic tumor (adenomat...
Figure 18.0b Enlargement of the mandible from non‐odontogenic tumor (multipl...
Figure 18.1
Figure 18.2
Figure 18.3
Figure 18.4a
Figure 18.4b
Figure 18.4c
Figure 18.4d
Figure 18.5a
Figure 18.5b
Chapter 19
Figure 19.0 Fordyce spots on the vermilion border of the upper lip.
Figure 19.1a
Figure 19.1b
Figure 19.2a
Figure 19.2b
Figure 19.3
Figure 19.4a
Figure 19.4b
Figure 19.5
Chapter 20
Figure 20.0 Lipoma of the neck.
Figure 20.1
Figure 20.2
Figure 20.3
Figure 20.4
Figure 20.5
Chapter 21
Figure 21.0 Hemangioma on the palate.
Figure 21.1
Figure 21.2a
Figure 21.2b
Figure 21.3
Figure 21.4
Figure 21.5
Chapter 22
Figure 22.0 Mucocele of the lower lip.
Figure 22.1a
Figure 22.1b
Figure 22.2
Figure 22.3a
Figure 22.3b
Figure 22.4a
Figure 22.4b
Figure 22.5
Chapter 23
Figure 23.A Teeth anomalies in a patient with pituitary dwarfism.
Figure 23.1
Figure 23.2a
Figure 23.2b
Figure 23.3a
Figure 23.3b
Figure 23.4
Figure 23.5
Figure 23.B Amelogenesis imperfecta in permanent teeth.
Figure 23.6
Figure 23.7
Figure 23.8
Figure 23.9
Figure 23.10
Figure 23.C Periapical cyst of a severed decayed upper molar.
Figure 23.11
Figure 23.12
Figure 23.13a
Figure 23.13b
Figure 23.14
Figure 23.15a
Figure 23.15b
Chapter 24
Figure 24.0a Hairy tongue (close‐up photo).
Figure 24.0b Geographic tongue (close‐up photo).
Figure 24.1
Figure 24.2
Figure 24.3
Figure 24.4
Figure 24.5
Chapter 25
Figure 25.0 Varicose veins of the ventral surface of the tongue.
Figure 25.1a
Figure 25.1b
Figure 25.2
Figure 25.3
Figure 25.4
Figure 25.5
Figure 25.6
Figure 25.7a
Figure 25.7b
Figure 25.8a
Figure 25.8b
Figure 25.9
Figure 25.10
Chapter 26
Figure 26.0a Licking cheilitis in a baby.
Figure 26.0b Tongue papillitis due to a viral infection in a child.
Figure 26.0c Traumatic lip ulceration in a teenager.
Figure 26.0d Multiple tongue aphthae in a lady with iron anemia.
Figure 26.0e Traumatic aphthous like ulceration of the lower anterior sulcus...
Figure 26.1
Figure 26.2
Figure 26.3
Figure 26.4
Figure 26.5
Figure 26.6
Figure 26.7a
Figure 26.7b
Figure 26.8
Figure 26.9
Figure 26.10
Chapter 27
Figure 27.0a Clinical sign of facial muscle palsy (incomplete smile).
Figure 27.0b Clinical (bleaching) test to confirm a vascular lesion.
Figure 27.0c Koebner phenomenon in bullous dermatoses.
Figure 27.1a
Figure 27.1b
Figure 27.2a
Figure 27.2b
Figure 27.2c
Figure 27.3a
Figure 27.3b
Figure 27.4a
Figure 27.4b
Figure 27.5
Figure 27.6a
Figure 27.6b
Figure 27.7a
Figure 27.7b
Figure 27.8
Figure 27.9a
Figure 27.9b
Figure 27.9c
Figure 27.10a
Figure 27.10b
Guide
Cover Page
Clinical Guide to Oral Diseases
Copyright
Preface
Foreword
Acknowledgment
Clinical Guide to Oral Diseases
Table of Contents
Begin Reading
Abbreviations
Diagnostic Flow Charts According to the Location of Oral Lesions
Appendix ICD‐10 Codes of Oral Diseases/Lesions
Index
WILEY END USER LICENSE AGREEMENT
Pages
iii
iv
vii
ix
xi
xiii
1
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
129
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
223
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248
249
251
252
253
254
255
256
257
258
259
261
262
263
264
265
266
267
268
269
271
272
273
274
275
276
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
297
298
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
321
322
323
324
325
326
327
328
329
331
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
369
370
371
372
373
374
375
376
377
378
379
380
381
382
383
384
385
386
387
389
390
391
392
393
394
395
396
397
398
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
Clinical Guide to Oral Diseases
Dimitris Malamos
DDS, MSC, PhD, Dip. O.M
Oral Medicine Specialist
Diplomat of the European Association of Oral Medicine
Head of the Oral Medicine Clinic at the National Organization for the Provision of Health Services
1st Health Region and at Iatrokosmos
Athens, Greece
Crispian Scully
CBE, DSc, DChD, DMed (HC), Dhc (Multi), MD, PhD, PhD (HC), FMedSci, MDS, MRCS, BSc, FDSRCS, FDSRCPS, FFDRCSI, FDSRCSEd FRCPath, FHEA
Emeritus Professor
University College
London, UK
Content EditorMárcio Diniz Freitas
Special Care Dentistry Unit
University of Santiago de Compostela
Spain
This edition first published 2021© 2021 John Wiley & Sons Ltd
All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by law. Advice on how to obtain permission to reuse material from this title is available at http://www.wiley.com/go/permissions.
The right of Dimitris Malamos and Crispian Scully to be identified as the authors of this work has been asserted in accordance with law.
Registered OfficesJohn Wiley & Sons, Inc., 111 River Street, Hoboken, NJ 07030, USAJohn Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK
Editorial Office9600 Garsington Road, Oxford, OX4 2DQ, UK
For details of our global editorial offices, customer services, and more information about Wiley products visit us at www.wiley.com.
Wiley also publishes its books in a variety of electronic formats and by print‐on‐demand. Some content that appears in standard print versions of this book may not be available in other formats.
Limit of Liability/Disclaimer of WarrantyThe contents of this work are intended to further general scientific research, understanding, and discussion only and are not intended and should not be relied upon as recommending or promoting scientific method, diagnosis, or treatment by physicians for any particular patient. In view of ongoing research, equipment modifications, changes in governmental regulations, and the constant flow of information relating to the use of medicines, equipment, and devices, the reader is urged to review and evaluate the information provided in the package insert or instructions for each medicine, equipment, or device for, among other things, any changes in the instructions or indication of usage and for added warnings and precautions. While the publisher and authors have used their best efforts in preparing this work, they make no representations or warranties with respect to the accuracy or completeness of the contents of this work and specifically disclaim all warranties, including without limitation any implied warranties of merchantability or fitness for a particular purpose. No warranty may be created or extended by sales representatives, written sales materials or promotional statements for this work. The fact that an organization, website, or product is referred to in this work as a citation and/or potential source of further information does not mean that the publisher and authors endorse the information or services the organization, website, or product may provide or recommendations it may make. This work is sold with the understanding that the publisher is not engaged in rendering professional services. The advice and strategies contained herein may not be suitable for your situation. You should consult with a specialist where appropriate. Further, readers should be aware that websites listed in this work may have changed or disappeared between when this work was written and when it is read. Neither the publisher nor authors shall be liable for any loss of profit or any other commercial damages, including but not limited to special, incidental, consequential, or other damages.
Library of Congress Cataloging‐in‐Publication Data
Names: Malamos, Dimitris, author. | Scully, Crispian, author. Title: Clinical guide to oral diseases / Dimitris Malamos, Crispian Scully. Description: Hoboken, NJ : Wiley‐Blackwell, 2021. | Includes index. Identifiers: LCCN 2020032170 (print) | LCCN 2020032171 (ebook) | ISBN 9781119328117 (paperback) | ISBN 9781119328131 (adobe pdf) | ISBN 9781119328155 (epub) Subjects: MESH: Mouth Diseases–diagnosis | Diagnosis, Oral | Case Reports Classification: LCC RK60.7 (print) | LCC RK60.7 (ebook) | NLM WU 140 | DDC 617.6/01–dc23 LC record available at https://lccn.loc.gov/2020032170LC ebook record available at https://lccn.loc.gov/2020032171
Cover Design: WileyCover Image: courtesy of Dimitris Malamos
Preface
The idea of writing this book was born one Sunday afternoon three years ago, when Professor Scully and I discussed some interesting and intriguing clinical cases for diagnosis. We thought it would be a good idea to provide various clinical photos, and respond to relevant questions in a way that the readers could be led to the proper diagnosis. Professor Scully wanted this new book to be reader‐friendly and hoped to approach the common oral diseases in a different way. This book would not be compared to any of the other outstanding and well‐written textbooks on oral medicine, as it would not be a complete review of oral diseases or rare syndromes.
This guide aims to present a large selection of clinical cases that are representative of the majority of oral common diseases that are seen in a daily clinical practice, and it is recommended to all physicians and oral health providers, including dental and medical undergraduate and postgraduate students, dentists and medical practitioners, especially dermatologists, as well as ear, nose and throat specialists, internists, and oncologists.
Despite Professor Scully's sudden death, the composition of the book writing took place as an effort to follow his idea. The book is designed to provide a short revision of oral medicine by using three different groups of multiple choice questions (MCQs) and answers based on clinical colored photos. Each group of questions has different degrees of difficulty in answering. The first group of questions is adequate for undergraduate students and is related to diagnosis; the second is addressed to medical and dental practitioners; while the last and more difficult is for postgraduate students.
This book is divided into three parts. The first part includes Chapters 1–14 and refers to the classification of oral lesions by appearance and symptomatology; the second part comprises Chapters 15–24 and encompasses the most common oral lesions by location; while the third part consists of Chapters 25–27 and refers to the oral lesions that are normal variations, or have an age predilection, or are part of various clinical phenomena. Parts I and III are composed of 10 cases in each chapter, while the Part II has five cases in each chapter. Additionally, a concise table and a short text relevant to each chapter and containing a list of the common oral lesions/conditions is provided before cases presentation.
This book is based on more than 260 good quality, colored clinical photos, making this guide a brief practical atlas of common oral diseases. These clinical images come from my personal records, and I am deeply grateful to my patients who gave their permission, and to my publication team for plotting these images carefully. Their help was unique, and without it, this book would not be feasible.
Dimitris MalamosAthens, 2020
Foreword
It is an honor and an immense satisfaction for me to provide the prologue for this book for two main reasons: the experience of its authors and the originality of this proposed editorial. When reviewing this ‘’Clinical Guide to Oral Diseases”, one is surprised by the practical perspective with which its authors have imbued it, combining basic principles of problem‐based learning with excellent images and an accurate and essential critical overview for arguing the differential diagnosis of each injury. Throughout the 27 chapters, the authors conduct an exhaustive review of the most common oral injuries based on the discussion of case studies. This approach perfectly combines Dimitris Malamos’ clinical experience and Crispian Scully’s academic rigor.
All of these features make this book a cross‐sectional work, which can be useful both for undergraduate students, general dentists and specialists in the setting of medical‐surgical dentistry. In the end, the success of the clinical activity is not based on academic titles but rather on the knowledge and expertise of the observer. In some manner, Professor Scully had already promulgated this idea during his final years, because he tended to end his emails with a phrase attributed to Goethe, “One only sees what one looks for. One only looks for what one knows.”
Pedro Diz DiosMD, DDS, PHD, EDOM, FRCSED ad hominemProfessor of Special Care DentistrySantiago de Compostela University, Spain
Acknowledgment
I would like to thank the individuals whose help made this Clinical Guide possible; particularly Mrs J. Saiprasad for being so helpful and co‐operative in determination to overcome delays in publication Mrs Carolyn Holleyman for checking the flowcharts and webcases, Mrs Susan Engelken for the cover of the book and especially Mr Vincent Rajan as Production Editor organizing and resolving problems before the publication and Mrs A. Argyropouloy for revising the text. I am grateful to my mentors Professor G. Laskaris (Greece) and Professor C. Scully (United Kingdom) as I truly appreciated their teaching and encouragement to me, to become seriously involved in Oral Medicine. Professor Scully's friendship, advice and expertise is still a part that I miss, and this book was written in his memory.
I wish also to express my sincere gratitude to Dr Pedro Diz Dios and to Dr Marcio Diniz Freitas for their help and advice throughout the preparation of this book. The participation of Dr Marcio Diniz Freitas as Content editor is precious.
Finally, I am especially indebted to my wife Vasiliki and my children Panagiotis and Katerina for their continuous love and support for all those years of my involvement in Oral Medicine, and during the preparation of this guide.
About the Companion Website
Don't forget to visit the companion website for this book:
www.wiley.com/go/malamos/clinical_guide
There you will find valuable material designed to enhance your learning, including:
Clinical cases
Further reading
Scan this QR code to visit the companion website
Section I
1 Bleeding
Bleeding in the mouth may be a sign of various conditions related to the structure of blood vessels, the number or function of white blood cells and especially platelets, the deficiency or dysfunction of clotting factors or even interaction of various drugs. Some of these bleeding disorders appear at a very young age; some are also found among close relatives (inherited) while others are noticed later with a negative family history (acquired). The severity of the bleeding ranges from minor hemorrhages from gingivae and other parts of the oral mucosa with the formation of petechiae or ecchymosis (Figure 1.0), to extensive bleeding in other parts of the body, causing severe blood loss, even jeopardizing the patient's life.
The more important causes of oral bleeding are seen in Table 1.
Figure 1.0 Tongue hematoma in a woman with seizures.
Table 1 Conditions related to oral bleeding.
Common and important conditions
Local conditions
Gingivitis/periodontitis
Granuloma pyogenic/giant cell
Jaw fracture
Trauma
Tumors invading blood vessels
Systemic conditions
Congenital
Hemophilia A or B
Von Willebrand's disease
Other factor deficiencies
Glanzman thrombasthenia
Acquired
related to coagulation
Liver disease
Vit. K deficiency, warfarin drug use
Disseminated intravascular coagulation
related to thrombocytopenia
Idiopathic
Drug‐induced
Collagen vascular disease
Sarcoidosis
Hemolytic anemia
Leukemia
Myeloma
Waldestmom
related to platelet dysregulation
Alcoholism
Chronic renal failure
Drugs
Liver disease
related to vascular disorders
Angina bullosa hemorrhagica
Angiomas
Ehrler‐Danlos syndrome
Hereditary hemorrhagic telangiectasia
Infections from Ebola, HIV, HSV; EBV, Rubella
Marfan syndrome
Purpura
Scurvy
related to fibrinolysis
Amyloidosis
Streptokinase treatment
Case 1.1
Figure 1.1a
Figure 1.1b
CO: A 62‐year‐old woman was referred by her family doctor for evaluation of several red spots on her lips, mouth, and the skin of her fingers.
HPC: The red spots had been present since childhood, but had become greater on the surface of her face over the last five years causing cosmetic problems and patient’s concern.
PMH: Her medical history revealed a chronic iron deficiency anemia which still remained despite the fact that the patient was in the post‐menopause phase and had been treated occasionally with iron tablets. No other serious medical problems were recorded except for a few episodes of nose and gut bleeding which had caused her to ask for medical advice. She was a non‐smoker and non‐drinker.
OE: The examination revealed numerous red vascular papules, variable in size, ranging from pin head‐like lesions to small red plaques at the vermilion border of her lips, and on the tongue and buccal mucosae (Figure 1.1a). A few asteroid‐like red lesions, were also seen on the skin of her fingers (Figure 1.1b) and inside her nose which were responsible for her episodes of epistaxis.
Q1 Which is the possible cause of her red spots?
Crest syndrome
Sjogren syndrome
Rendu‐Osler‐Weber syndrome
Rosacea
Ataxia‐telangiectasia
Answers:
No
No
Rendu‐Osler‐Weber syndrome or
hereditary hemorrhagic telangiectasia
(
HHT
) is a rare autosomal dominant condition that affects blood vessels throughout the body (telangiectasia; arteriovenous malformations) with a tendency for bleeding. This vascular dysplasia is commonly seen in oral, nasopharynx, lung, liver, spleen, gastrointestinal and urinary tracts, conjunctiva and the skin of arms and fingers.
No
No
Comments: Skin telangiectasias are also seen in patients with ataxia telangiectasia, Crest and Sjogren syndromes. In rosacea, main vascular lesions are the broken vessels that are located exclusively on the skin predominantly on the middle of the face, as in ataxia telangiectasia. In ataxia telangectasia, the vascular lesions are associated with poor coordination, and in Crest syndrome with calcinosis and sclerodactyly and Raynaud phenomenon. Sjogren's syndrome affects the mouth, eyes, nose and other organs causing dryness, swelling of the salivary glands and facial telangiectases.
Q2 Which are the main complications of this condition?
Anemia
Pulmonary hemorrhage
Ischemic stroke
Skin photosensitivity
Mental retardation
Answers:
Iron deficiency anemia is a very common complication induced by a series of episodes of blood loss through the nose (epistaxis) and gastrointestinal tract (melena stools) from telangiectic lesions.
Pulmonary hemorrhage is mainly found in patients older than 40 years old and with multiple visceral involvements, causing breathing problems, portal hypertension and liver cirrhosis.
Ischemic stroke is a rare yet serious complication in patients with HHT, and requires special care.
No
No
Comments: The vascular lesions on facial skin sometimes cause cosmetic problems, but never skin photosensitivity, while the brain lesions of HHT may cause neuro‐psychiatric complications with various pathways which have not been related to mental illness before.
Which genes are linked with this condition?
Endoglin gene
(
ENG
)
Fibroblast growth factor receptor 3
(
FGFR3
)
Activin receptor like kinase (ALK‐1)
Collagen type I alpha 1 chain(COL1A1)
Dentin sialophosphoprotein
(
DSPP
)
Answers:
Engoglin gene mutations have been isolated in HHT families (type 1)
No
Activin receptor like kinase (ALK‐1)mutations have been found in HHT (type 2)
Comments: Mutations in the COL1A1 and COL1A2 genes are related to the development of the majority of osteogenesis imperfecta (>90%), while FGFR3 is associated with fibrous dysplasia and DSPP with dentinogenesis imperfecta.
The following abbreviations are used throughout the book – CO: Complains of; HPC: History of present complaint; PMH: Past medical history; OE: oral examination.
Case 1.2
Figure 1.2
CO: A six‐year‐old boy was admitted with bleeding of his mouth.
HPC: The patient sustained a facial injury during a football match half an hour before the bleeding.
PMH: He was a healthy child with no serious medical problems. He was very sociable, and used to take part in all activities at his kindergarten.
OE: He is a very young child, feeling stress and fear because of the bleeding in his mouth, especially from the area of deciduous central right incisor. This tooth had been pushed into its hemorrhagic and swollen gingivae (Figure 1.2). No other problems with the rest of his teeth, jaws, and oral mucosa were noticed.
Q1 What is the possible cause of the hemorrhage of this child?
Trauma
Self‐induced
Infections
Children abuse
Bleeding disorders
Answers:
Facial trauma is commonly noticed among children and characterized by soft tissue injuries (lips, oral mucosae, face) or deep ones into the maxilla or mandibular bone and their associated teeth. Facial trauma is responsible for the “impressive” bleeding due to the high vascularity of this area.
No
No
No
No
Comments: The absence of multiple bruises and hematomas alone, or with the different ages of lesions combined with the history of the accident and type of injuries in a child's body is an easy way to exclude bleeding disorders or child abuse from the diagnosis. The absence of fever, swelling and erythema in the lesion rules out infections (bacterial, viral, or fungal). In addition to this, the lack of similar lesions in the past together with the child's good healthy social life reinforces the idea that the lesion was not self‐induced.
Q2 Which is/are the difference(s) of facial trauma between children and adolescents?
Etiology
Bone involvement
Symptomatology
Complications
Recovery rate
Answers:
Facial trauma is caused by falling in children and by assault or altercation in adolescents.
Fractures of nose bones or jaws are more common in adolescents rather than in children.
The symptomatology in children does not fit with the severity of the lesions and is more remarkable than in adolescents.
The facial trauma in children is more superficial than in adolescents and their complications seem to be minimal.
The younger the children, the easier their recovery.
Q3 Which is the clinician's first priority when faced with a patient with facial injury?
Calm patient and his parents
Retain the airway open
Check for broken or dislocated teeth
Stop bleeding
Treat facial wound (cleaning and suturing)
Answers:
No
Retaining child's airway open is the first priority as the mucosal edema is disproportional with the patient's airway tract. The clinician should remove obstacles like debris, clots and foreign bodies from the oropharynx, control the location of patient's tongue while in severe cases an orotracheal intubation could be mandatory.
No
No
No
Comments: The second priority for the clinicians is to control bleeding by putting direct pressure on the facial injury. Having bleeding under control, clinicians are then able to properly examine the soft tissue injury, investigate for possible teeth and jaws fractures and then go further to cleanse and suture the wound, as well as reassuring the patient and his parents.
Case 1.3
Figure 1.3
CO: A 32‐year‐old woman presented with a soft hemorrhagic lump on her lower left gingivae.
HPC: The lump appeared three months ago and became gradually bigger, covering the whole crown of the second premolar, thus causing eating difficulties and phobias to the patient of being a malignant neoplasm.
PMH: A healthy woman at the third month after baby delivery, with no serious medical problems and drug use apart from iron and calcium tablets prescribed by her gynecologist during her pregnancy. Smoking or drinking habits were plentiful.
OE: A very soft penduculated mass on the gingivae from the distal part of the 1st lower right premolar to the 1st molar. It was very soft, vascular and sensitive, and was bleeding easily with slight probing and caused eating problems (Figure 1.3). The lesion developed gradually and reaching its biggest site at the last month of pregnancy and began to decrease slowly within the next three months after her delivery. No other similar lesions were found within her mouth, other mucosae or skin. Regional or systemic lymphadenopathy was not recorded.
Q1What is this lesion?
Kaposi's sarcoma
Pregnancy epulis
Peripheral giant cell granuloma
Gingival hemangioma
Peripheral ossifying fibroma
Answers:
No
Pregnancy epulis is a localized hyperplastic hemorrhagic soft lesion on the upper and lower gingivae of pregnant women with decayed teeth and poor oral hygiene. The lesion grows slowly and reaches its largest size during the last trimester of pregnancy.
No
No
No
Comments: In contrary to pregnancy epulis the gingival hemangiomas are found earlier (at childhood); sarcoma Kaposi are usually associated with lymphadenopathy and have an aggressive course. The peripheral odontogenic fibroma has a firmer feel on palpation, while the peripheral giant cell epulis does not improve with the baby's birth and is associated with endocrinopathies.
Q2Which are the other oral conditions seen during pregnancy?
Melasma
Pregnancy gingivitis
Increased risk of caries
Erosions of teeth
Sialorrhea
Answers:
No
Pregnancy gingivitis is the commonest complication of pregnancy and can start even from the second month, reaching its peak on the eight month of pregnancy. This type of gingivitis is due rather to the action of increased female hormones on their gingival receptors rather than to microbial plaque.
Pregnant women tend to be at increased risk of caries as the number of cariogenic bacteria in the mouth, and the frequency of eating, especially sweet food as a means of coping with nausea, are increased.
Erosions on the palatal tooth surface and especially on the upper anterior teeth are common and are also attributed to the acidity of gastric juice that reaches the mouth during vomiting.
Sialorrhea is a common finding in pregnant women and caused by the increased nausea and vomiting recorded during their pregnancy.
Comments: Melasma or pregnancy mask as it is known, is characterized by a brown discoloration of the facial skin and lips, but is never seen within the mouth of pregnant women and those taking contraceptives or hormone replacement medications.
Q3 Which conditions have been detected in babies, related to the periodontal status of their mothers?
Premature birth
Low weight
Vision or hearing deficits
Mental retardation
Dental anomalies
Answers:
Women with chronic inflammation of their gingivae seem to produce a number of inflammatory cytokines, some of which are responsible for the uterine muscle contractions which finally induce early labor.
Premature babies show incomplete growth and low weight.
Vision or hearing deficits are commonly seen in premature babies whose early birth may be associated with the periodontal problems of their mother.
No
No
Comments: The mental status of pregnant women may worsen their periodontal problems by increased secretion of cortisol and refusal of tooth brushing, while the periodontitis per se does not affect the mental status or dentition of their children.
Case 1.4
Figure 1.4
CO: A 42‐year‐old woman came in with a hemorrhagic bulla inside her cheek.
HPC: The bulla appeared three hours ago after eating a sandwich. No similar bullae were recorded in her or her close relatives in the past.
PMH: From her medical records a few episodes of allergic rhinitis controlled with antihistamine and steroids in crisis were recorded. No blood and other systemic diseases, other allergies or drug uptakes were recorded.
OE: Examination revealed a large bulla with hemorrhagic content on the left buccal mucosa at the occlusion level (Figure 1.4). The bulla appeared during mastication and was easily broken during the examination's manipulations, leaving a painful superficial ulceration. No other bullae, ulcerations or petechiae and ecchymoses were seen on the oral and other mucosae or skin. Cervical lymphadenopathy was not seen.
Q1 Which is the disease responsible for this bulla?
Thrombocytopenia
Burns
Mucous membrane pemphigoid
Angina bullosa hemorrhagica
Hemorrhagic mucocele
Answers:
No
No
No
Angina bullosa hemorrhagica
(
ABH
) is an acute, benign condition characterized by the development of subepithelial bullae filled with blood that are not attributed to any systemic disorders. A chronic trauma, consumption of hot and spicy or abrasive foods, or difficulties in restorative or periodontal treatment are considered to be the commonest causes.
No
Comments: Hemorrhagic bullae are often seen in other conditions such as thrombocytopenia, mucous pemphigoids and burns, but the presence of specific elements indicated the diagnosis. The appearance of low platelets and ecchymoses, epistaxis, and gingival bleeding in thrombocytopenia, the presence of numerous bullae with clear fluid in mucous pemphigoid, and the lack of close contact with thermal, chemical, or electrical elements in burns help to exclude these conditions from the diagnosis. Mucoceles are thicker and more resistant, while the bullae in angina are thinner and more easily break.
Q2 Which of the drugs below are usually related to the development of this condition?
NSAIDs
Antibiotics
Steroids
Anti‐diabetics
Bronchodilators
Answers:
No
No
Chronic use of steroids, especially inhalers, causes oral mucosa atrophy and decreases the submucosa's elastic fiber content, resulting in capillary breakdown locally, finally forming the characteristic hemorrhagic bullae.
No
No
Comments: Diabetes mellitus has also been associated with hemorrhagic bulla formation due to increased vascular fragility in these patients, and not to the drug for blood sugar reduction. Similar bullae could also be seen in patients who take antibiotics or bronchodilators and have various autoimmune diseases. As for NSAIDs, these drugs are responsible for peptic ulcers and bleeding from the intestine, but more rarely for skin bullous rash and fever.
Q3 Which of the histopathological finding(s) is/or are characteristics of this condition?
Subepithelial bulla
Intra‐epithelial abscess of neutrophils
Mononuclear inflammatory infiltration of submucosa deep to the muscles
Direct immunofluorescence negative
Eosinophils accumulation in the corium
Answers:
The breakage of the epithelial–connective tissue junction due to topical agents leads to local capillary hemorrhage and subepithelial bulla formation.
No
No
Direct immune‐fluorescence is always negative. DI is always positivein pemphigus and other intra‐epithelial blistering diseases.
No
Comments: The inflammatory response in ABH is intense and located only at the superficial parts of submucosa, often containing neutrophils but not eosinophils and mast cells.
Case 1.5
Figure 1.5
CO: A 48‐year old man was presented with a hemorrhagic lesion on the floor of his mouth.
HPC: The lesion appeared six months ago while the bleeding was noticed during eating three days ago.
PMH: No serious medical problems were recorded apart from an episode of severe pneumonia which was diagnosed last December and was treated with a strong course of antibiotics. No other drugs were taken, but the patient was a smoker (>40 cigarettes, daily) and a drinker (4–5 glasses of wine or relevant spirit per meal).
OE: The examination revealed an asymptomatic white lesion on the floor of mouth extended from the left lower premolar to the molar region. The lesion was fixed in palpation and had a warty‐like surface with two to three bleeding areas (Figure 1.5). Smoking‐induced lesions such as increased gingival pigmentation, nicotinic stomatitis and brown teeth discoloration were also found, together with ipsilateral, fixed, enlarged cervical lymph nodes where oral or skin petechiae and ecchymoses were not seen.
Q1 What is the cause of bleeding?
Traumatic ulceration
Pemphigus vegetans
Verrucous leukoplakia
Giant verruca vulgaris
Squamous carcinoma
Answers:
No
No
No
No
Squamous cell carcinoma is the cause of his oral bleeding. This tumor is a locally aggressive, tumor which appears as an indurated swelling, ulceration or plaque of various cellular differentiation and risk of metastasis. This lesion grows either slowly and superficially, but in majority of cases grows fast and invades deep tissues such as muscles and blood vessels causing muscle dysfunction and bleeding.
Comments: This tumor differs from other vegetating oral lesions such as hyperplastic traumatic ulcerations, pemphigus vegetans, verrucous leucoplakia, and verrucous vulgaris. The lack of local trauma or other vegetating lesions in the flexures of the patient rules out traumatic ulceration and pemphigus vegetans from the diagnosis, while the hard consistency and strong fixation of the lesion with the underling tissues is not an indication of verrucous vulgaris and leukoplakia where biopsy is required.
Q2 Although the verrucous carcinoma is a variation of oral carcinomas, it differs from the other types in the following histological characteristics:
Evidence of dysplasia in adjacent epithelium
Shape of the rete pegs
Absence of keratinization
Location of mitosis
Basal basement membrane status
Answers:
Dysplastic epithelium is often seen close to the oral squamous, but not to verrucous carcinomas.
The shape of rete pegs entering the corium is variable in the majority of oral carcinomas, but is bulbous, like elephant feet in verrucous carcinoma.
No
In oral carcinomas, the mitoses are scattered in the basal and spinous layer, while in verrucous carcinoma they are located mainly in the basal layer.
In oral carcinomas the basal membrane is invaded by tumor islands, but in verrucous carcinoma it is intact and the tumor grows superficially as well.
Comments: Keratinization is commonly seen in both tumors; however keratin pearls are mainly found in squamous carcinoma, while keratin plugs are found in verrucous carcinomas.
Q3 Which of the measures below is/are not amenable to control bleeding from an oral carcinoma?
Identification of the underlying cause of oral bleeding
Blood investigations
Packing‐dressing
Suturing
Radiotherapy
Answers:
No
No
No
No
Radiotherapy is sometimes useful to the control of excessive bleeding that may arise from lung but not oral carcinomas. Patients with oral carcinomas and other head and neck tumors have already received the maximum dose of radiotherapy when bleeding begins, and therefore other aggressive measures such as arterial embolization should be undertaken.
Comments: Clinicians must control oral bleeding by following some basic steps such as the identification of the causative factor by taking a comprehensive history and careful clinical examination; excluding bleeding diseases by checking white blood count and clotting profiles as well as packing or dressing with hemostatic agents, while in more severe cases with cauterization, suturing, or embolization should be used.
Case 1.6
Figure 1.6a
Figure 1.6b
CO: A 24‐year‐old male was referred for an evaluation of bleeding from his upper lip.
HPC: The hemorrhage appeared on his upper lip during eating from a broken bulla three hours ago.
PMH: This young man suffers from Down syndrome and over the last two years he has been complaining about multiple bullae on the skin of his legs, mouth, and genitals. He had a short course of steroid cream for skin bullae which was not effective, causing him to refuse any other medications since then.
OE: An anxious young man, showing numerous ulcerations inside his mouth, lips, and legs as a result of ruptured bullae due to friction. A hemorrhagic ulceration on his upper lip (Figure 1.6a) together with a tiny hemorrhage of the nail bed of his middle finger was found (Figure 1.6b). No other hemorrhagic lesions (petechiae or ecchymoses) were seen inside his mouth, skin or other mucosae. On the other hand, epistaxis was not referred and general symptomatology was absent. The patient was admitted to an examination, and blood results revealed no clotting disorders while biopsy of the skin revealed a subepithelial bulla with positive immunofluorescence of IgG and C3 along the basement membrane zone (BMZ).
Q1 What is the cause of his lip bleeding?
Self‐induced lip trauma
Pemphigoid disorders
Clotting disorder
Erythema multiforme
Herpetic stomatitis
Answers:
No
Pemphigoid bullous diseases (mucous and bullous) are a group of subepithelial bullous disorders which affect mainly the mouth (mucous type; or less frequently bullous type) or the skin. They have a characteristic immunofluorescence profile. Their bullae break easily and leave painful hemorrhagic ulcerations covered with hemorrhagic crusts as seen in this patient.
No
No
No
Comments: Clotting disorders are easily excluded from the diagnosis as the blood tests were negative. Herpetic stomatitis causes similar hemorrhagic oral lesions but is ruled out as this condition lacks chronic skin lesions and its severe mouth lesions occur only once and not constantly, as seen in this patient. Erythema multiforme shows similar findings with the patient's lesions, but is also excluded due to the short duration of its lesions and presence of fibrin instead of IgG and C3 with BMZ. Factitious illness is a problem in the disabled but not in Down syndrome patients, as these are less likely to develop maladaptive behavior and the patient did not show any aggressive behavior capable of causing self‐induced lesions in his body.
Q2 Which of the bullous disorders is/or are initiated with urticarial skin lesions?
Pemphigus vulgaris
Bullous pemphigoid
Cicatricial pemphigoid
Paraneoplastic pemphigus
Dermatitis herpetiformis
Answers:
No
Bullous pemphigoid is a chronic subepithelial blistering disease that starts as an urticarial eruption which develops large firm bullae, especially in flexor skin areas over a course of weeks to months.
No
No
Dermatitis herpetiformis is a chronic pruritic papulovesicular eruption which is associated with urticarial wheals and located symmetrically on the extensor surfaces of skin.
Comments: Although paraneoplastic pemphigus and cicatricial pemphigoid are chronic bullous disorders affecting oral and other mucosae and appear either as fragile intra‐epithelial bullae associated with a neoplasm (leukemia or lymphoma) or subepithelial bullae, they are never associated with pruritic rash and scarring.
Q3 Which lip conditions are presented with lip bleeding?
Exfoliate cheilitis
Erythema multiforme
Actinic prurigo
Granulomatous cheilitis
Perioral dermatitis
Answers:
Exfoliate cheilitis is a common cheilitis characterized by the production of keratin scales in the vermilion border of lips in young women with anxiety, who have the habit of removing the scales by rubbing them against their teeth thus leaving ulcerated hemorrhagic lesions.
Erythema multiforme is an acute mucocutaneous reaction characterized by erythematous plaques, painful hemorrhagic bullae and erosions in the skin (target like lesions), in the mouth and other mucosae. The presence of hemorrhagic crusts on the lips is pathognomonic for this condition.
Chronic exposure to solar radiation causes actinic prurigo, a photodermatosis affecting the skin, lips and conjunctiva. Lips are usually erythematous, scaly and in places bleed while the skin lesions appear as itchy, red papillae or nodules on cheeks, nose, forehead or arms, and eyes showing hyperemia, photophobia and pseudopterygium.
No
No
Comments: Perioral dermatitis is a chronic itchy papulopustular rash affecting the skin around the mouth while granulomatous cheilitis is a chronic, persistent swelling of lips due to granulomatous inflammations. Neither of them have a bleeding tendency.
Case 1.7
Figure 1.7
CO: A 36‐year‐old woman was presented with hemorrhage from her tongue.
HPC: Her tongue bleeding appeared one month ago when she gave birth to a baby girl. The bleeding had arisen from a superficial strawberry‐like soft mass on the dorsum and inferior part of her tongue while it deteriorated with mastication movements.
PMH: Her medical history revealed no serious diseases such as bleeding disorders. A case of iron deficiency anemia was only recorded since puberty which was treated with iron supplements as well as a few tongue surgeries for the elimination of a vascular lesion of her tongue in the past. The patient was not a supporter of smoking or drinking habits, while she used to spend her free time painting.
OE. The oral examination revealed multiple small hemorrhagic dots on the dorsum and inferior part of tongue (Figure 1.7) which were similar to a mature strawberry. These dots are superficial and could easily bleed with touching, and were overlying a soft vascular mass. This mass was detected when she was one year old, and became larger during puberty, requiring surgery. It remained stable until her pregnancy when it became bigger and was occasionally bleeding. No other similar lesions, petechiae, or ecchymoses were found on her body.
Q1 What is the cause of bleeding?
Hemangioma
Vascular malformation
Kaposi sarcoma
Pregnancy pyogenic granuloma
Wegener granulomatosis
Answers:
No
Vascular malformations are characterized by abnormalities of the capillary, venous or arterio‐venous vascular bed which appear at birth or a few months later, and grow gradually. Contrary to other vascular lesions though, they do not resolve; instead they can be exacerbated with various conditions such as pregnancy.
No
No
No
Comments: Based on the early onset and long duration of this single lesion,without resolution throughout the coming years hemangiomas are easily excluded while the long duration and slow progress without other similar lesions in patient’s body or general symptomatolog rules out extensive pyogenic grannulomas or Wegener granulomatatosis from the diagnosis.
Q2 What are the differences between hemangiomas and vascular malformations?
Location
Course
Symptomatology
Pathogenesis
Complications
Answers:
No
Hemangiomas appear mostly at birth, grow rapidly and resolve during puberty while vascular malformation remain or even worsen.
No
Hemangiomas are characterized by endothelial hyperplasia while in vascular malformations the endothelial cell turnover is normal.
Both hemangiomas and vascular malformations cause a variety of complications from mild esthetic disfiguration to severe possibility of jeopardizing the patient's life dependent on the size and location of the lesion closely to vital organs.
Q3 Which of the syndromes below is/or are not associated with this condition?
Sturge‐Weber syndrome
PHACE syndrome
Proteus syndrome
Maffucci syndrome
Blue rubber bleb nevus syndrome (BRBNS)
Answers:
No
PHACE syndrome is characterized by multi‐organ lesions such as posterior fossa anomalies; facial hemangiomas, arterial and cardiac anomalies as well as eye problems
No
No
No
Comments: Abnormal vascular malformations are often seen in a number of syndromes like Sturge‐Weber; Maffucci, Proteus and blue rubber belb but all of them have different clinical presentation. Sturge‐Weber syndrome is characterized by numerous facial (port‐wine stain) and cerebral angiomas, glaucoma, seizures and mental retardation while in Maffucci syndrome, angioma is associated with numerous endochondromas. Proteus syndrome has characteristic skin, bone, muscle and vascular abnormal growths, while venous malformations of the gastrointestinal tract and skin are seen in blue rubber bleb nevus syndrome.
Case 1.8
Figure 1.8
CO: A 68‐year‐old woman was presented with hemorrhagic gingivae over the last three months.
HPC: Her gingivae showed areas of hemorrhage over the last three months and was associated with generalized lymphadenopathy, fever, weight loss and sweating at night.
PMH: Hyperlipidemia and diabetes mellitus were the only serious diseases reported. A recent blood check‐up revealed an increased number of eosinophils and lymphocytes as well as chronic sideropenic anemia, despite her proper diet. No smoking or drinking habits, but a chronic exposure to chemicals because of her job at a painting industry was reported.
OE: The examination revealed swollen, soft, edematous and hemorrhagic gingivae that were associated with a few scattered petechiae on buccal mucosae. The gingivae were pale and easily bled from the interdental papillae (Figure 1.8). A few ecchymoses were also found on her legs and associated with a generalized lymph node enlargement.
Q1 What is the cause of her gingival bleeding?
Acute ulcerative gingivitis
Scurvy
Leukemia
Plasma cell gingivitis
Wegener disease
Answers:
No
No
Leukemia is the cause. Leukemia is a malignant neoplasm of white blood cells characterized by an abnormal growth of a certain type of white cells, anemia, easy bruising or bleeding, susceptibility to infections, swollen lymph nodes, together with weight loss and night sweating, as was also observed in this patient who was finally diagnosed of having chronic lymphocytic leukemia
No
No
Comments: Gingival bleeding is a common finding in other local conditions such as in acute ulcerative and plasma cell gingivitis, or systemic diseases such as Wegener disease and scurvy. The lack of necrosis of interdental papillae (seen in acute ulcerative gingivitis) and the erythematous and edematous red attached gingivae (in plasma cell gingivitis) or the erythematous swollen‐like‐strawberries gingivae (in Wegener disease) and the ulcerated, swollen gingivae with deep pocketing (in scurvy) exclude the above diseases from the diagnosis.
Q2 Which laboratory tests are routinely used for the diagnosis of this condition?
White blood count
Immunophenotypic analysis with flow cytometry
Bone marrow biopsy
Urine analysis
Cerebral fluid biochemical analysis
Answers:
White blood count shows an increased number of lymphocytes (>10,000 cells/mm
3
).
The flow cytometric analysis of the bone marrow aspiration cells and peripheral blood cells with the use of a series of monoclonal antibodies allow the identification of hematologic malignancies including chronic lymphocytic leukemia (CLL).
Bone marrow biopsy is used in undiagnosed cases of blood dyscrasias showing the replacement of bone marrow cells with pathologic lymphocytes.
No
No
Comments: Urinalysis and cerebrospinal fluid (CSF) analysis are useful only in a diagnosis of aggressive leukemias like CLL, involving bladder and brain respectively.
Q3 Which other conditions are associated with this disease?
Anemia
Thrombocytopenia
Eosinophilia
Complement deficiency
Paraproteinemia
Answers:
Anemia is a very common complication of CLL due to: (i) bone marrow accumulation of abnormal lymphocytes inducing the replacement of stem cells producing red cells; (ii) increased production of tumor necrosis factor (TNF) that suppresses red blood cell production; (iii) increased red cell destruction by circulated auto‐antibodies; and (iv) medications used for treatment of CLL that suppress red cell production.
Thrombocytopenia is responsible for the increased bleeding tendency among patients with CLL.
Eosinophilia is sometimes a preclinical sign of various hematological malignancies including lymphomas and CLL.
Complement deficiency is a common finding and seems to limit CD20 monoclonal cytotoxicity in treatment’s efficacy for these patients.
Monoclonal proteins are present in significant number of patients with CLL.
Case 1.9
Figure 1.9
CO: A 32‐year‐old woman was presented with red spots on her palate.
HPC: The red palatal lesions were asymptomatic and discovered by her GDP during her regular dental check‐up last week.
PMH: Her medical history revealed an asymptomatic HIV infection over the last 14 months and a few opportunist lung infections this winter. She was on no medication at the moment apart from a few broad antibiotics taken for her respiratory infections. Her HIV infection was probably caught after a blood transfusion given 10 years ago to recover after a car accident. She was non‐smoker or drinker.
OE: A few scattered red spots on both parts of hard and occasionally soft palate and buccal mucosae. These lesions did not bleach with pressure, but were associated with severe periodontal disease regardless of her young age (Figure 1.9) and cervical lymphadenitis.
Q1 What is the cause of palatal petechiae?
Fellatio
Infectious mononucleosis
Nicotinic stomatitis
HIV‐induced thrombocytopenia
Rendu‐Osler‐Weber syndrome
Answers:
No
No
No
Palatal petechiae on this lady appear due to thrombocytopenia induced by HIV infection. This is one of the early manifestations of the disease such as atypical oral ulcerations, infections like pseudo‐membranous or erythematous candidiasis, reactivation of herpes zoster infection and acute ulcerative gingivitis/periodontitis.
No
Comments: Rendu‐Osler‐Weber syndrome can be easily excluded, as this is about having scattered telangiectasia since childhood, in contrast with the hemorrhagic spots (petechiae) that were found in this young lady. Asymptomatic petechiae are also seen on the soft palate and on margins of the hard with the soft palate after orogenital sex, which this lady had not reported. Asymptomatic palatal red spots are characteristics in nicotinic stomatitis, but the red spots there represent the inflamed duct openings of minor salivary glands and not petechiae. Palatal petechiae associated with general lymphadenopathy are also seen in patients with infectious mononucleosis, but the typically increased number of monocytes in the blood test and positive mononucleosis (mono) test, excludes this condition from diagnosis.
Q2 Which is/are the difference/s between petechiae and purpura?
Size
Location
Reaction to pressure
Symptomatology
Shape
Answers:
Petechiae are hemorrhagic spots with a diameter of <5 mm while purpura have a 5–9 mm diameter.
No
No
No
Petechiae have round, regular lesions while the shape of purpura and ecchymoses may be irregular.
Comments: Both hemorrhagic lesions do not blanch with pressure, are usually asymptomatic and can be found anywhere in the body.
Q3 What are the causes of thrombocytopenia apart from an HIV infection?
Leukemia
Epilepsy
Hepatitis C infection
Heavy alcohol consumption
Anorexia nervosa
Answers:
Thrombocytopenia is very common sign of an acute myelogenous and lymphocytic leukemia, as well as in advanced chronic lymphocytic and in progressive myelogenous leukemia. The reduced number of platelets has been attributed to: (i) bone marrow replacement by leukemic cells; (ii) increased destruction of platelets by swollen spleen or cytotoxic drugs for leukemia treatment; and (iii) immune destruction of platelets in some CLL cases.
No
Thrombocytopenia is a major problem in HCV+ patients as it interferes with various measurements for its diagnosis and follow‐up. The cause of thrombocytopenia is multifarious and is due to: (i) immunogenicity; (ii) direct bone marrow suppression; (iii) hypersplenism; (iv) decreased production of thrombopoeitin; and (v) drug reactions.
The chronic use of alcohol affects the production, survival time and functions of platelets while it also increases their destruction rate by an enlarged spleen leading to thrombocytopenia. The cessation of drinking within the second week raises the number of platelets again.
Anorexia nervosa causes thrombocytopenia. The reduced production of platelets is attributed mainly to low thrombopoietin rather than folic acid levels due to malnutrition.
Comments: Anti‐epileptic drugs such as valproate and levetiracetam but not the disease per se cause thrombocytopenia.
Case 1.10
Figure 1.10
CO: A 42‐year‐old man was admitted with gingival bleeding since the previous night.
HPC: The bleeding started suddenly after eating a snack with potato chips and became more intense and constant on the lower molar gingivae. No similar bleeding episodes had been reported previously by him or his close relatives.





























