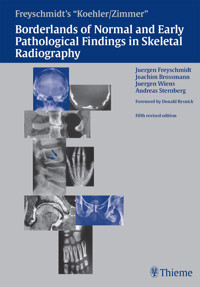
Freyschmidt's "Koehler/Zimmer" Borderlands of Normal and Early Pathological Findings in Skeletal Radiography E-Book
Jürgen Freyschmidt
149,99 €
Mehr erfahren.
- Herausgeber: Thieme
- Kategorie: Fachliteratur
- Sprache: Englisch
The classic text in a revised and expanded fifth edition!
Is a radiological finding normal or pathologic? This "borderline" between the two states presents a daunting challenge to radiologists and orthopedic surgeons on a daily basis. Thieme proudly presents the updated and expanded fifth edition of the landmark text generations of physicians have used to differentiate borderline findings!
Redesigned for optimal use, the book is organized according to diagnostic questions raised by clinical findings, radiographic findings, or both. You'll find all possible variants in five pathologic categories: anomaly; trauma; necrosis; inflammation; and tumor. The book provides imaging examples of the entire body, from the skull base, shoulder, and clavicle, to lower spine, knees, and the feet. More than 4,200 high-quality illustrations give clear examples of potential findings.
Key features of this historic text:
- Illustrated with more than 4,200 outstanding drawings, photographs, and radiographs--nearly 4 per page!
- Full coverage of pathologic conditions in their fully developed form,
- Exhaustive analysis of borderline findings for both pediatric and adult cases
- Valuable guidelines on integrating pathologic conditions with CT and MRI findings
This book is the encyclopedic resource that will expand your knowledge of findings in skeletal radiology and enhance your diagnostic skills. No personal or professional library is complete without this new standard-bearer in the field!
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 1988
Veröffentlichungsjahr: 2002
Ähnliche
Freyschmidt's “Koehler/Zimmer”
Borderlands of Normal and Early Pathological Findings in Skeletal Radiography
Fifth revised edition
Juergen Freyschmidt, M.D.
Professor and Director Division of Diagnostic Radiology and Nuclear Medicine Zentralkrankenhaus Sankt–Juergen–Strasse Bremen, Germany
Joachim Brossmann, M.D.
Professor Division of Diagnostic Radiology Hospital of the University of Kiel Kiel, Germany
Juergen Wiens, M.D.
Division of Diagnostic Radiology and Nuclear Medicine Zentralkrankenhaus Sankt–Juergen–Strasse Bremen, Germany
Andreas Sternberg, M.D.
Division of Diagnostic Radiology and Nuclear Medicine Zentralkrankenhaus Sankt–Juergen–Strasse Bremen, Germany
Foreword by Donald Resnick, M.D.
4206 Illustrations 74 Tables
ThiemeStuttgart • New York
Library of Congress Cataloging-in-Publication Data is available from the publisher
1st German edition, 1910
2nd German edition, 1915
3rd German edition, 1920
4th German edition, 1924
5th German edition, 1928
6th German edition, 1931
7th German edition, 1939
8th German edition, 1943
9th German edition, 1953
10th German edition, 1956
11th German edition, 1967
12th German edition, 1982
13th German edition, 1989
14th German edition, 2001
1st English edition, 1956
2nd English edition, 1961
3rd English edition, 1968
4th English edition, 1993
1st French edition, 1930
2nd French edition, 1936
3rd French edition, 1956
1st Italian edition, 1955
2nd Italian edition, 1967
3rd Italian edition, 1986
1st Spanish edition, 1933
2nd Spanish edition, 1959
This book is an authorized and revised translation of the 14th German edition published and copyrighted 1910, 2001 by Georg Thieme Verlag, Stuttgart, Germany. Title of the German edition: Freyschmidt's “Köhler/Zimmer”: Grenzen des Normalen und Anfänge des Pathologischen in der Radiologie des kindlichen und erwachsenen Skeletts
Important Note: Medicine is an ever-changing science undergoing continual development. Research and clinical experience are continually expanding our knowledge, in particular our knowledge of proper treatment and drug therapy. Insofar as this book mentions any dosage or application, readers may rest assured that the authors, editors, and publishers have made every effort to ensure that such references are in accordance with the state of knowledge at the time of production of the book.
Nevertheless, this does not involve, imply, or express any guarantee or responsibility on the part of the publishers in respect to any dosage instructions and forms of applications stated in the book. Every user is requested to examine carefully the manufacturers' leaflets accompanying each drug and to check, if necessary in consultation with a physician or specialist, whether the dosage schedules mentioned therein or the contraindications stated by the manufacturers differ from the statements made in the present book. Such examination is particularly important with drugs that are either rarely used or have been newly released on the market. Every dosage schedule or every form of application used is entirely at the user's own risk and responsibility. The authors and publishers request every user to report to the publishers any discrepancies or inaccuracies noticed.
Translated by Terry C. Telger, Fort Worth, TX, USA
© 1956, 2003 Georg Thieme Verlag,
Rüdigerstraße 14, D-70469 Stuttgart, Germany
http://www.thieme.de
Thieme New York, 333 Seventh Avenue,
New York, N.Y. 10001 U.S.A.
http://www.thieme.com
Cover design: Thieme MarketingTypesetting by Druckhaus Götz, Ludwigsburg Printed in Germany by Druckhaus Götz, Ludwigsburg
ISBN 3-13-784105-4 (GTV)
ISBN 1-58890-150-5 (TNY) 1 2 3 4 5
Some of the product names, patents, and registered designs referred to in this book are in fact registered trademarks or proprietary names even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
This book, including all parts thereof, is legally protected by copyright. Any use, exploitation, or commercialization outside the narrow limits set by copyright legislation, without the publisher's consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, mimeographing or duplication of any kind, translating, preparation of microfilms, and electronic data processing and storage.
For our children
Fritz-Maximilian, Johannes, Benedikt, Christina and grandchildren
Carla, Felix, and Robert
Foreword
Once again, I have the honor to prepare the foreword for the monumental text Borderlands of Normal and Early Pathological Findings in Skeletal Radiography, edited by Drs. Juergen Freyschmidt, Joachim Brossmann, Juergen Wiens, and Andreas Sternberg. This latest edition is true to the tradition of excellence that was readily apparent in the previous version. It again emphasizes the interface between what should be considered normal and what is pathologic, an interface that is encountered every day on multiple occasions by any physician who is involved in the interpretation or review of imaging studies, whether they appear on the viewbox or, with increasing frequency, on the computer screen.
As would be expected, much has transpired since the publication of the last edition of this work. Old concepts have been clarified, have changed considerably, or have even been discarded, and new concepts have emerged. Dr. Freyschmidt and colleagues have addressed these modified or new ideas through the use of important alterations in the text and a dramatic increase in the number of illustrations, all well chosen to display the findings in as vivid a fashion as possible. A new emphasis on advanced imaging methods, such as computed tomography and magnetic resonance imaging, is apparent throughout and certainly justified, but the importance of conventional radiographic analysis remains central. The organization of the book has also been updated, with new reliance on the assessment of five basic pathologic processes: dysplasia, trauma, necrosis, inflammation, and tumor.
Why purchase and read this book? Simply, because the knowledge that one would gain by doing so would clearly lead to a marked improvement in accurate assessment of skeletal images. More specifically, one's ability to differentiate between clinically significant and insignificant findings would improve dramatically, resulting in more appropriate patient care. Yes, there are other available books on this subject, and some are quite good. Borderlands is unique and my favorite, however, because of its organization, completeness, and focus. The previous edition was situated in a prominent place in my office—I referred to it often (some of its pages are now folded or torn) as did our residents and fellows. This new addition will sit alongside it and I expect its fate will be the same. In short, this is not a book to be placed on the shelf and forgotten but one to use on a regular basis.
Dr. Freyschmidt and colleagues are to be congratulated for once again providing the rest of us with an invaluable reference source. To complete such a work is no easy task, and the authors have my deep admiration. It is a privilege for me to provide this foreword, and I congratulate the editors on a job well done.
Donald Resnick, M.D.
Chief, Osteoradiology
Professor of Radiology
University of California, San Diego
Preface
With the increasing use of cross-sectional imaging modalities in skeletal radiology, our knowledge of the true anatomic relationships of many normal variants and borderline findings has grown considerably. Meanwhile, concepts regarding the clinical importance of some variants and borderline findings have changed, especially in sports-related conditions.
Faced with these facts, we felt that a new approach was needed in organizing our material.
This fifth edition of Borderlands is based on a new didactic approach, which is intended to give the book an unprecedented logical consistency throughout. The material is organized according to the basic diagnostic questions that are raised by the primary clinical findings, the primary radiographic findings, or both. As in other organ systems, key diagnostic issues are based on several broad pathologic categories:
– Anomaly
– Trauma
– Necrosis
– Inflammation
– Tumor
When faced with a skeletal finding that may be a normal variant or one of the basic types of pathology listed above, the reader can turn to a specific portion of the book to decide whether the finding is normal or definitely pathologic.
Borderline findings are difficult to collect for publication, either because they were missed or because the first radiographic examination was performed too late. Also, borderline findings can be difficult to portray in an illustration, as it is not possible to bring out certain relevant details by changing the viewing conditions (e.g. by using an iris diaphragm with a halogen source for reading a plain film or by adjusting the computer screen). For these reasons, the book also deals with pathological conditions in their fully established forms. By knowing the fully developed presentation, the radiologist can easily picture earlier forms that occupy the “borderland” range.
We have maintained the tradition of including some rare entities among the illustrations. This has been done to uphold the reputation of the book as an “all-in-one” reference source.
We suggest that the reader study Chapter 1, as it covers methods and stratagems for separating the wheat from the chaff, i.e., differentiating normal and still normal findings (variants) from findings that are definitely pathological.
Bremen, KielJ. FreyschmidtAutumn, 2002J. BrossmannJ. WiensA. SternbergContents
1 Introduction to the Radiological Evaluation of Normal Variants
J. Freyschmidt
References
Appendix
2 Upper Extremity
J. Freyschmidt
The Hand
Metacarpus and Phalanges
General Aspects
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Degenerative Changes?
Soft-Tissue Calcifications
Specific Bones of the Hand
Distal Phalanges
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture? Dislocation?
Necrosis?
Inflammation?
Tumor?
Middle Phalanges
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation, Tumor?
Other Changes?
Proximal Phalanges
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Inflammation?
Tumor?
Thumb
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Other Changes?
Metacarpus
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
References
Carpus (wrist)
General Aspects
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Specific Bones of the Carpus
Trapezium
Normal Findings
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Tumor?
Trapezoid
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Capitate
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Hamate
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Inflammation? Tumor?
Scaphoid
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Inflammation?
Tumor?
Lunate
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Inflammation?
Tumor?
Triquetrum
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Pisiform
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture or Dislocation?
Necrosis?
Inflammation?
References
Forearm
Distal Radius and Ulna
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Diaphysis of the Forearm
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
References
Elbow Region
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Tumor?
Inflammation?
Soft-Tissue Calcifications and Ossifications, Changes at the Fibro-osseous Junction
References
Upper Arm
Diaphysis
Normal Findings
Pathological Finding?
Fracture
Inflammation, Tumor?
Soft-Tissue Calcifications
References
Proximal Humerus
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Tumor?
Inflammation?
References
3 Shoulder Girdle and Thorax
J. Freyschmidt
Scapula
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
References
Acromioclavicular Joint
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
The Shoulder Joint as a Whole
Soft-Tissue Anatomy of the Shoulder Joint
Shoulder Impingement and Rotator Cuff Tears
Shoulder Dislocation and Shoulder Instability
Calcifications and Ossifications in the Soft Tissues of the Shoulder
References
Clavicle and Sternoclavicular Joint
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Sternum
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Ribs
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
4 Skull
J. Wiens, A. Sternberg
General Aspects
References
Cranial vault
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Special Aspects
Frontal Bone
Parietal Bone
Squamous Temporal Bone
Occipital Bone
References
Skull Base
Anterior, Middle, and Posterior Cranial Fossae
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Sella Turcica
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Tumor?
Temporal Bone
Middle Ear, Air Cells, and External Auditory Canal
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Petrous Temporal Bone and Inner Ear
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Styloid Process, Hyoid Bone, Larynx
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Facial Skeleton
Orbit
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Other Changes?
Nose: Nasal Bone, Cartilaginous Nasal Skeleton, and Nasal Cavity
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Other Changes?
Paranasal Sinuses
During Growth
Maxillary Sinus
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Frontal Sinus
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Ethmoid Cells
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Sphenoid Sinus
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Zygomatic Arch
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Inflammation?
Tumor?
Mandible
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Other Changes?
Temporomandibular Joint
Normal Findings
Pathological Finding?
Normal Variant/Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
5 Spinal Column
J. Brossmann
Introduction
Atlas and Axis
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Midcervical and Lower Cervical Spine
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Thoracic Spine
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Lumber Spine
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Sacrum and Coccyx
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Sacroiliac Joints
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Other Changes?
References
6 Pelvis
J. Freyschmidt
General Aspects
Normal Anatomy
Examination Technique
Trauma
Osteonecrosis of the Acetabulum, Femoral Head, and Femoral Neck
Ossification and Calcification of Soft-Tissue Structures
Anomalies and Deformities
Structural Changes
References
Pelvis, Specific Section
Ilium
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Pubis, Pubic Symphysis, and Ischium
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Hip Joint
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
7 Lower Extremity
J. Freyschmldt
Femur
Femoral Shaft
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
Other Changes?
References
Distal Femur
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Patella
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
Other Changes?
References
Proximal Tibia and Fibula
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
Other Changes?
References
Knee joint as a Whole
Normal Findings, Variants, Early Pathological Changes
Pathological Findings?
Other Changes?
References
Shaft of the Tibia and Fibula
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture?
Necrosis?
Inflammation?
Tumor?
References
Distal Tibia and Fibula
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Inflammation?
Tumor?
Other Changes?
References
Foot
General Aspects
Normal Findings
Pathological Finding?
Variants?
Anomalies?
Soft-Tissue Variants
References
Specific Bones of the Foot
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
References
Calcaneus
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Navicular Bone
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
Other Changes?
References
Cuboid Bone
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
References
Medial Cuneiform Bone
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Other Changes?
References
Intermediate and Lateral Cuneiform Bones
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
References
Metatarsal Bones
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Tumor?
Other Changes?
References
Sesamoid Bones
Normal Findings
Pathological Finding?
Variant or Anomaly/Deformity?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation?
Other Changes?
References
Toes
Normal Findings
Pathological Finding?
Normal Variant or Anomaly?
Fracture, Subluxation, or Dislocation?
Necrosis?
Inflammation? Tumor?
References
Index
The differentiation of a normal anatomic variant from a skeletal abnormality based on empirical visual assessment is not the real problem in the diagnostic radiology of borderline findings between normal and early pathology.
This problem arises only when a patient's clinical symptoms may have something to do with the radiological variant, or when the variant itself may harbor pathological changes (e.g., necrosis), or when a pathological process mimics a normal anatomic variant (Table 1.1).
The problems in this situation cannot be solved by visual assessment alone. The solution, rather, lies in the true art of medicine, which includes the interpretation of pain and neurological symptoms and the selection of further diagnostic procedures (such as radionuclide scanning or MRI). It may also include recommending an appropriate treatment.
We know from experience that routine radiographic examinations in hospital and office settings most often demonstrate normal findings along with more or less harmless normal variants. Unless the radiologist is familiar with this type of finding, there are likely to be numerous false-positive studies leading to unnecessary additional (and costly)diagnostic and therapeutic measures.
At the same time, the prevalence of normal findings and harmless normal variants in routine practice can engender a kind of complacency that makes it hard for radiologists to recognize a symptomatic normal variant or even a definite abnormality that is mimicking a normal variant.
In any given case, therefore, the following question should be added to the standard checklist or algorithm for radiographic interpretation: Is it possible that the normal variant is clinically significant, or is a supposed normal variant actually a pathological process?
How Can These Pitfalls Be Avoided?
The basic approach to radiological interpretation follows the principles of pattern recognition.
The basic criteria for image interpretation in conventional radiography and computed tomography (CT) are as follows:
• Shape
• Size
• Position relative to surrounding structures (topography)
• Symmetry
• Density
In a radionuclide bone scan, the regional degree of tracer uptake is evaluated in addition to the basic interpretive elements of shape, size, topography, and symmetry.
Most of the skeletal disorders discussed are associated with an increase in radiotracer uptake.
An increase in uptake means only that bone turnover or metabolism in a given area is increased or that the radiotracer has a greater affinity for the pathological process than for surrounding tissues. The cause of the increased uptake may be a traumatic, neoplastic, necrotic, or inflame-matory process. Nevertheless, a radiologist with some experience in osteology and the recognition of radionuclide patterns can often establish the identity of a lesion.
A whole-body scintigram should always be obtained, if necessary using SPECT (single-photon emission computed tomography) and a pinhole collimator.
In magnetic resonance imaging (MRI), the signal intensity in various sequences replaces density as a basic criterion for image interpretation.
In projection radiography (plain film or digital), which still accounts for more than 80% of all radiological studies, projection geometry and the superimposition effect are additional key elements in interpreting radiographic films.
Projection geometry influences shape, size, and topography, while the superimposition effect mainly influences density. Superimposition refers not only to the superimposed projection of several bones or bony elements but also to the summation of internal or substructures contained within a single bone. Thus, while a bony ridge produces a linear density in an orthograde projection, a bony groove or canal appears as a linear lucency. Plain radiographs of a cancellous bone area are never identical, because the slightest rotation of the bone relative to the film plane (even by 1° or 2°) will significantly after the projection of the individual bony trabeculae and may cause them to appear thickened. If two bony elements of different density are superimposed, an effect called the Mach band phenomenon occurs, creating a line of apparent radiolucency that is comparable to an optical illusion. In zones of contrasting radiographic densities, areas of higher density are perceived as being darker while areas of lower density appear lighter.
The various changes of the individual elements of pattern recognition and their combination ultimately determine how a particular skeletal abnormality will be classified. The basic categories of skeletal abnormality that are encountered in radiological practice are listed below:
• Anomaly (malformation, deformity)
• Fracture, subluxation, or dislocation
• Necrosis
• Inflammation
• Tumor
Of course, changes in pattern recognition criteria do not create a pathological entity—the reverse is true. Nevertheless, the process of radiological interpretation always follows this “reverse path.” So whenever a radiograph shows what appears to be a variant, it is important to ask whether the questionable feature might possibly be a component or manifestation of a fracture, necrosis, inflammation, etc.
The following cases will help to illustrate these points.
• An isolated bony element at the end of the acromion (Fig. 3.34) raises various diagnostic possibilities. It may be an acute or old nonunited fracture or a persistent apophysis with no clinical significance, or its shape and position may be such that it predisposes to rotator cuff impingement. In making this differentiation, it is important to consider the history and clinical findings. An isolated bony element found distal to the acromion after shoulder trauma should be interpreted as a fresh fracture if the patient reports isolated tenderness over the site, perhaps accompanied by crepitation. But if these circumscribed signs are absent, it should be assumed that the feature is an incidental finding based on an anatomic variant. If radiographs were ordered for unexplained shoulder pain not related to trauma, the radiologist should decide whether the shape and position of the accessory bony element are sufficient to narrow the subacromial space and cause an impingement injury with a partial or full tear of the supraspinatus tendon in the case of hyperextension. This question is most easily resolved by ultrasonography or MRI, depending on availability and examiner experience.
• A 50-year-old woman complains of pain in the metatarsophalangeal joint of the right big toe after prolonged walking. She gives no history of trauma. A radiograph shows a relatively dense “bipartite” lateral sesamoid and mild hallux valgus deformity of the toe. Question: Is the lateral sesamoid a normal anatomic variant (duplication), does the bone exhibit necrotic fragmentation, or is the pain caused by metatarsophalangeal osteoarthritis that is not yet visible on radiographs? Clinical examination is not helpful in this case because both extreme flexion and hyperextension elicit pain throughout the metatarsophalangeal joint, and the pain is very poorly localized on palpation of the plantar side. Further evaluation by radionuclide bone scan is indicated (Fig. 7.440). Increased uptake in the lateral “bipartite” sesamoid would indicate necrotic fragmentation, necessitating surgical removal. Increased uptake in the subchondral portion of the bone would be more suggestive of osteoarthritis.
• A 5-year-old child presents with nonspecific pain in the right knee. Radiographs show rarefaction and irregularity of the distal medial metaphyseal cortex. Differential diagnosis: inflammation, malignant tumor, or cortical irregularity?
The region is completely normal to palpation and ultrasound scanning. The opposite knee has the same radiographic appearance. The finding can now be confidently interpreted as a transient cortical irregularity (normal variant), and there is no need for follow-ups (Fig. 7.45). It should be added, however, that highly typical radiographic findings in a bone do not always require a “confirmatory” view of the opposite side. Also, the absence of a corresponding finding on the opposite side does not preclude a normal variant, since many such variants occur on one side only. But if the area is tender to pressure and also shows slight swelling, the case warrants further investigation by bone scanning or modern sectional imaging techniques.
Rules for Correctly Identifying Variants
Accessory bone element:
An accessory bone element arises from an isolated ossification center that is independent of the adjacent “established” bone, or it may result from a failure of fusion of a second ossification center at the margin of the established bone. In the last case generally a synchondrosis persists between the accessory element and the established bone. Painful regressive changes may develop in a synchondrosis that is exposed to adverse mechanical stresses (Table 1.1). The accessory bone element is entirely surrounded by cortical bone and does not “complete” the other bone (Figs. 2.205 and 2.151 b). The main differential diagnosis is a detached bone fragment, which is generally distinguished by irregular fracture margins and by the absence of a cortical boundary in acute cases. This is not the case in nonunions (Fig. 2.129d). Displaced fragments geometrically “complete” the adjacent bone from which they were fractured. Theoretically they could be fitted back into the defect in the parent bone, just as a surgeon does when performing an internal fixation. When a posttraumatic radiograph is obtained in an acute situation, clinical palpation and a knowledge of the possible fracture mechanism are helpful if the diagnosis is in question. When a patient is examined weeks or months later for purposes of disability assessment, the examiner should not only consider the morphological criteria listed above but also decide whether the accessory bone element seen in the radiograph corresponds to one of the known accessory bones that have been named and described. This problem is discussed more fully elsewhere in the text (p. 117 ff.).
With regard to the naming of accessory bones, most of these bones have been given Latin names based on their first describer or their anatomic location. Given the wealth of detailed knowledge that today's medical practitioners must have, we do not feel it is necessary to know the names of every accessory bone that may be encountered.
It is not the name of an accessory bone that is important, but its correct identification as such.
Instead of using the term “os subfibulare,” for example, it is quite acceptable to write: “accessory bone element located below the tip of the fibula."
The next entity requiring differentiation from an accessory bone element is a fragmented osteonecrosis. Generally the necrotic bone is denser than normal bone and lacks internal structural features. The radionuclide bone scan (see above) is definitive in terms of differential diagnosis.
A final differential diagnosis is an ossified tissue matrix, as illustrated by circumscribed myositis ossificans (Fig. 2.235) or paraosseous cartilaginous formations. The late stage of myositis ossificans is indistinguishable from an accessory bone by its morphological features alone, because the lesion has an internal structure and a cortical boundary (Fig. 2.235), contrasting with the ill-defined ossification seen in earlier stages. Cartilaginous calcification patterns usually show some kind of lobulation, and geometric figures (e.g., rings, arcs, stars) that come from a superposition of ossified interlobular septa.
An unusual or extraneous-appearing density within a bone:
The density may result from a different overlapping bone, due either to an atypical projection or atypical relative positions of the bones. It can also have other causes such as an exceptionally well-developed bony ridge (e.g., linea aspera), which usually appears as a linear density (Fig. 7.3a). Finally, it may represent a pathological bony structure on or within the bone. The best solution to this problem is to obtain a contralateral film or, when dealing with an unpaired element such as a vertebral body, to compare the left and right halves on the same film. Spot films can also be obtained to resolve projection-related issues. CT may be necessary in selected cases.
An unusual or extraneous-appearing lucency within a bone:
If the lucency is linear, differentiation is required between a fracture and a Mach band phenomenon. If the lucency is not linear, it may represent a circumscribed area of rarefied cancellous bone, thinned cortical bone, or a deep groove or cleft in the outer surface of the bone. A familiar example is the greater tuberosity of the humerus, which appears as an elliptical lucency (Fig. 2.431). This feature can vary markedly among different individuals and is due simply to a diminution of cancellous trabeculae combined with an increased proportion of fatty marrow. In questionable cases, especially when symptoms are vague, doubts can be resolved by examining the opposite side or proceeding with CT or MRI. As a rule, though, the reader should know the typical skeletal sites at which such lucencies typically occur. The same applies, of course, to normally occurring densities.
Beginners in particular should avoid ordering costly tests just because they lack the knowledge to interpret these phenomena correctly.
It is equally important, especially in symptomatic patients, to avoid the temptation to classify radiographic densities as normal, even if they appear to blend harmoniously with surrounding features.
The following two phenomena should be familiar to anyone who interprets radiographs:
• Gray cortex: The “gray cortex” is a result of circumscribed resorptive changes in normal cortical bone caused by focal osteoclastic activity induced, say, by an inflammatory or neoplastic bone lesion (Figs. 7.10, 7.14 a, 7.20 a).
• Loss of differentiation between the cortex and marrow cavity, especially in tubular bones: This occurs when the radiographic density of the bone marrow is increased due to a pathological process (matrix ossification due to osteosarcoma, bone necrosis, deposition of calcium phosphate or calcium carbonate compounds, etc.). Normally the marrow or medullary cavity of a tubular bone contains fat. Replacement of the fat by nonmineralized tumor tissue is not detectable on conventional radiographs unless the tumor tissue causes circumscribed, lacuna-like resorptive changes (scalloping) in the endosteal cortical margin.
A bony structure appears too large or too small or has an unusual shape:
This finding may represent a normal variant, bone dysplasia, or an aquired deformity. Again, it is helpful to obtain contralateral radiographs for comparison. If the same changes are seen, they may result from a systemic pathological process. “Gamut lists” (like those of Reeder and Felson) are very often helpful for identifying morphological variants, and several chapters in this book list differential diagnoses based on morphological criteria. Otherwise the history and clinical findings should be used to aid interpretation. A detailed description of congenital skeletal dysplasias, dysostoses, and acquired deformities is beyond our present scope but may be found in the specialized literature.
The 1992 International Classification of Osteo-chondrodysplasias is presented without commentary at the end of this chapter (Appendix, Table 1.2). Published by J. Spranger (European Journal of Pediatrics 51 [1992] 407–415), this classification was compiled by an international panel of experts on bone dysplasias at a conference in Bad Honnef (26–28 June 1991). Unlike the older Parisian Nomenclature for the classification of constitutional skeletal diseases, the International Classification is based solely on radiological criteria, with diseases grouped on the basis of similar morphological features. It was the opinion of the expert panel that the former “mixing” of clinical, pathogenetic, and radiological criteria led to inconsistencies and was too imprecise. Clinical criteria, such as age at disease onset and course, are no longer used because they are too variable and depend too much on the diagnostic experience and therapeutic activities of the reader. Spranger notes that, despite major advances in the fields of biochemistry and molecular biology, our knowledge of etiology and pathogenesis is still too sketchy to attempt a causal type of classification. But the table does provide information on gene locations, protein defects, and modes of inheritance. The classification pertains exclusively to osteochondrodysplasias, i.e., developmental disturbances of chondro-osseous tissue. The new classification does not include dysostoses, which are defined as developmental disturbances of individual bones.
Spranger also points out that the work done to date is still rudimentary and that further revision is needed. This prompted us to include the unabridged 1986 version of the Parisian Nomenclature, which does include dysostoses (Appendix, Table 1.3).
References
Berg, E. E.: The symptomatic os subfibulare: avulsion fracture of the fibula associated with recurrent instability of the ankle. J Bone Jt Surg. 73-A (1991) 1251
Cuono, C. B., H. K. Watson: the carpal boss: surgical treatment and etiological considerations. Plast, reconstr. Surg. 63 (1979) 88
Henderson, R. S.: Os intermetatarseum and a possible relationship to hallux valgus. J Bone Jt Surg. 45-B (1963) 117
Johnson, R. P., B. D. Collier, G. F. Carrera: The os trigonum syndrome: use of bone scan in the diagnosis. J. Trauma 24 (1984) 761
Keats, T. E.: Atlas of Normal Roentgen Variants That May Simulate Disease, 6th ed. Mosby-Year Book, Chicago 1996
Lawson, J. P.: Clinically significant radiologic anatomic variants of the skeleton. Amer. J. Roentgenol. 163 (1994) 249
Lawson, J. P., J. A. Ogden, E. Sella et al.: The painful accessory navicular. Skelet. Radiol 12 (1984) 250
Ogden, J. A., S. M. McCarthy, P. Jokl: The painful bipartite patella. J. pediat. Orthop. 2 (1982) 263
Reeder, M. R.: Reeder and Felson's Gamut's in Bone, Joint and Spine Radiology. Springer, Berlin 1993
Spranger, J.: International classification of osteochondrodysplasias. Europ. J. Pediat. 151 (1992) 407
Van Holsbeeck, M., B. Vandamme, G. Marchal et al.: Dorsal defect of the patella: concepts of its origin and relationship with bipartite and multipartite patella. Skelet. Radiol. 16 (1987) 304
I. Osteochondrodysplasias
(Growth and developmental disturbances of and/or bone)
1. Growth and developmental disturbances of tubular bones and/or the spinal column
(A) Manifested at birth
(a) Usually lethal before or shortly after birth
1. Type I achondrogenesis (Parenti-Fraccaro)
2. Type II achondrogenesis (Langer-Saldino)
3. Hypochondrogenesis
4. Fibrochondrogenesis
5. Thanatophoric dysplasia
6. Thanatophoric dysplasia with cloverleaf skull
7. Atelosteogenesis
8. Short-rib syndromes (with or without polydactyly)
(a) Type I (Saldino-Noonan)
(b) Type II (Majewski)
(c) Type III (lethal thoracic dysplasia)
(b) Usually nonlethal dysplasias
9. Chondrodysplasia punctata
(a) Rhizomelic form, autosomal recessive
(b) X-linked dominant form
(c) Common, mild form (Sheffield); exclude: symptomatic forms, chromosome abnormalities
10. Camptomelic dysplasia
11. Kyphomelic dysplasia
12. Achondroplasia
13. Diastrophic dysplasia
14. Metatropic dysplasia (several forms)
15. Chondroectodermal dysplasia (Ellis-van Creveld)
16. Asphyxiating thoracic dysplasia (Jeune)
17. Spondyloepiphyseal dysplasia congenita
(a) Autosomal dominant form
(b) Autosomal recessive form
18. Kniest dysplasia
19. Dyssegmental dysplasia
20. Mesomelic dysplasia
(a) Nievergelt type
(b) Langertype (probably homozygous dyschondrosteosis)
(c) Robinowtype
(d) Reinhardt type
(e) Other
21. Acromesomelic dysplasia
22. Cleidocranial dysplasia
23. Otopalatodigital syndrome
(a) Type I (Langer)
(b) Type II (André)
24. Larsen syndrome
25. Other syndromes with multiple joint dislocations (Desbuquois, etc.)
(B) Manifested in later life
1. Hypochondroplasia
2. Dyschondrosteosis
3. Metaphyseal chondrodysplasia, Jansen type
4. Metaphyseal chondrodysplasia, Schmid type
5. Metaphyseal chondrodysplasia, McKusick type
6. Metaphyseal chondrodysplasia with exocrine pancreatic insufficiency and cyclic neutropenia
7. Spondylometaphyseal dysplasia
(a) Kozlowski type
(b) Other forms
8. Multiple epiphyseal dysplasia
(a) Fairbanktype
(b) Other forms
9. Multiple epiphyseal dysplasia with early diabetes (Wolcott-Rallisson)
10. Arthro-ophthalmopathy (Stickler)
11. Pseudoachondroplasia
(a) Dominant
(b) Recessive
12. Spondyloepiphyseal dysplasia, tarda (X-linked recessive)
13. Progressive pseudorheumatoid chondrodysplasia
14. Spondyloepiphyseal dysplasia, other forms
15. Brachyolmia
(a) Autosomal recessive
(b) Autosomal dominant
16. Dyggve-Melchior-Clausen dysplasia
17. Spondyloepimetaphyseal dysplasia (various forms)
18. Spondyloepimetaphyseal dysplasia with loose joints
19. Otospondylometaepiphyseal dysplasia (OSMED)
20. Myotonic chondrodysplasia (Catel-Schwartz-Jampel)
21. Parastremmatic dysplasia
22. Trichorhinophalangeal dysplasia
23. Acrodysplasia with retinitis pigmentosa and nephropathy (Saldino-Mainzer)
2. Anarchic development of cartilage and fibrous tissue
1. Dysplasia epiphysealis hemimelica
2. Multiple cartilaginous exostoses
3. Acrodysplasia with exostoses (Giedion-Langer)
4. Enchondromatosis (Oilier)
5. Enchondromatosis with hemangiomas (Maffucci)
6. Metachondromatosis
7. Spondyloenchondroplasia
8. Osteoglophonic dysplasia
9. Fibrous dysplasia (Jaffe-Lichtenstein)
10. Fibrous dysplasia with skin pigmentation and precocious puberty (McCune-Albright)
11. Cherubism (familial fibrous dysplasia of the jaw)
3. Anomalies of bone density, cortical structure, and/ or metaphyseal modeling defects
1. Osteogenesis imperfecta (several forms)
2. Juvenile idiopathic osteoporosis
3. Osteoporosis with pseudoglioma
4. Osteopetrosis
(a) Autosomal recessive lethal
(b) Intermediate recessive
(c) Autosomal dominant
(d) Recessive with tubular acidosis
5. Pyknodysostosis
6. Dominant osteosclerosis, Stanescu type
7. Osteomesopyknosis
8. Osteopoikilosis
9. Osteopathia striata
10. Osteopathia striata with cranial sclerosis
11. Melorheostosis
12. Diaphyseal dysplasia (Camurati-Engelmann)
13. Craniodiaphyseal dysplasia
14. Endosteal hyperostosis
(a) Autosomal dominant (Worth)
(b) Autosomal recessive (van Buchem)
(c) Autosomal recessive (sclerosteosis)
15. Tubular stenosis (Kenny–Caffey)
16. Pachydermoperiostosis
17. Osteodysplasia (Melnick–Needles)
18. Frontometaphyseal dysplasia
19. Craniometaphyseal dysplasia (several forms)
20. Metaphyseal dysplasia (Pyle)
21. Dysosteosclerosis
22. Osteoectasia with hyperphosphatasia
23. Oculodento-osseous dysplasia
(a) Mild type
(b) Severe type
24. Infantile cortical hyperostosis (Caffey disease, familial type)
Inheritance
AR
AR
AR
AR
AR
AR
XLD, lethal in males
AR
AD
AR
AR, AD
AR
AD
AR
AD
AR
AD
AD, AR
AD
AR
AD
XLD
XLR
AR, AD
AD
AD
AD
AD
AR
AR
AD
AD
AR
AR
AD
AR
AL
XLR
AR
AR
AD
AR
AR
AR
AR
AD
AD
AR
AD
AD
AR
AD
AR, AD
AR
AR
AR
AD
AR
AR
AD
AD
AD
AD
AD
AD
AR
AD
AR
AR
AD
AD
AD
XLR
AD
AR or AD
AR or XLR
AR
AD
AR
AD
II. Dysostoses
(Malformations of individual bones, isolated (combined)
1. Craniofacial dysostoses
1. Craniosynostosis (various forms)
2. Craniofacial dysostosis (Crouzon)
3. Acrocephalosyndactyly
(a) Apert type
(b) Chotzen type
(c) Other types
4. Acrocephalopolysyndactyly (Carpenter, etc.)
5. Cephalopolysyndactyly (Greig)
6. Syndromes of the first and second branchial arches
(a) Mandibulofacial dysostosis (Treacher–Collins, Franceschetti)
(b) Acrofacial dysostosis (Nager)
(c) Oculoauriculovertebral dysostosis (Goldenhar)
(d) Hemifacial microsomia
(e) Other (probably parts of a broad spectrum)
7. Oculomandibulofacial syndrome (Hallermann–Streiff–Francois)
2. Dysostoses with predominant involvement of the axial skeleton
1. Vertebral segmentation defects (including Klippel–Feil)
2. Cervico-oculoacoustic syndrome (Wildervanck)
3. Sprengel deformity
4. Spondylocostal dysostosis
(a) Dominant form
(b) Recessive form
5. Oculovertebral syndrome (Weyers)
6. Osteo-onychodysostosis
7. Cerebrocostomandibular syndrome
3. Dysostoses with predominant involvement of the extremities
1. Acheiria
2. Apodia
3. Tetraphocomelia (Roberts) (SC pseudothalidomide syndrome)
4. Ectrodactyly
(a) Isolated
(b) Ectrodactyly, ectodermal dysplasia (cleft palate syndrome)
(c) Ectrodactyly with scalp defects
5. Oroacral syndrome (aglossia syndrome, Hanhart syndrome)
6. Familial radioulnar synostosis
7. Brachydactyly types A, B, C, D, E (Bell's classification)
8. Symphalangia
9. Polydactyly (several forms)
10. Syndactvly (several forms)
11. Polysyndactyly (several forms)
12. Camptodactyly
13. Manzke syndrome
14. Poland syndrome
15. Rubenstein–Taybi syndrome
16. Coffin–Siris syndrome
17. Pancytopenia-dysmelia syndrome (Fanconi)
18. Blackfan–Diamond anemia with thumb combined) malformations (Aase syndrome)
19. Thrombocytopenia-radial aplasia syndrome
20. Orodigitofacial syndrome
(a) Papillon–Leage type
(b) Mohrtype
21. Cardiomelic syndrome (Holt–Oram and others)
22. Femoral focal defect (with or without facial anomalies)
23. Multiple synostoses (including several forms of symphalangia)
24. Scapuloiliac dysostosis (Kosenow–Sinios)
25. Hand-foot-genital syndrome
26. Focal dermal hypoplasia (Goltz)
AD
AD
AD
AR
AD
AD
AR
AD
AR
AD
AR
AR
AD
AD
AD
AR
AR
AR
XLD, lethal in males
AR
AD
AD
AD
AD
XLD, lethal in males
III. Idiopathic osteolyses
1. Phalangeal (several forms)
2. Tarsocarpal
(a) Including Francois type and others
(b) With nephropathy
3. Multicentric
(a) Hajdu–Cheney type
(b) Winchester type
(c) Torg type
(d) Other types
AR
AD
AD
AR
AR
IV. Miscellaneous diseases with osseoi involvement
1. Acceleration of skeletal maturity in young children
(a) Marshall–Smith syndrome
(b) Weaver syndrome
(c) Other types
2. Marfan syndrome
3. Congenital arachnodactyly with contractures
4. Cerebrohepatorenal syndrome (Zellweger)
5. Coffin–Lowry syndrome
6. Cockayne syndrome
7. Fibrodysplasia ossificans congenita
8. Epidermal nevus syndrome (Solomon)
9. Nevoid basal cell carcinoma syndrome
10. Multiple congenital fibromatosis
11. Neurofibromatosis (several types)
AD
AD
XLD
AR
AD
AD
V. Chromosome abnormalities
VI. Primary metabolic disorders
AD
Autosomal dominant
AR
Autosomal recessive
XLD
X-linked dominant
XLR
X-linked recessive
The Hand
The skeleton of the hand (carpus, metacarpus, phalanges) contains an average of 31 bones including the more common sesamoids. The number of joints in the hand is variable, ranging from 25 to 28 depending on carpal joint anatomy. The metacarpals and phalanges (except for the sesamoids) are tubular bones, while the carpus is composed of small, irregular, nontubular bones. This abundance of bony elements and joints correlates with an almost overwhelming number of variants in terms of number, size, structure, and density and with a great variety of pathological changes due to trauma, necrosis, inflammation, etc.
The hand causes very little x-ray scattering, making its skeleton an ideal object for radiography. Some features, such as early structural bone changes and early inflammatory joint changes, are best displayed by using mammo-graphic technique and reading the film with a magnifying lens or by performing direct geometric magnification radiography using a microfocus tube.
A good way to deal with equivocal findings is to obtain a radiograph of the opposite side and, when interpreting the films, examine each individual bony element for unusual or abnormal features.
The favorable imaging conditions in the hand are one reason why the hand is used as a radiological test region for many systemic disease processes (e.g., renal osteodystrophy, acromegaly, polyarticular joint diseases such as rheumatoid arthritis, psoriatic arthritis, etc.).
Metacarpus and Phalanges
General Aspects
We start with a discussion of the general radiographic aspects of the metacarpus and phalanges because numerous variants and pathological changes can exist in multiple bones simultaneously and in varying degrees, and a general perspective is needed to interpret and classify them correctly. Another purpose of this general introduction is to highlight certain anatomic and pathoanatomic features that the different bones have in common, and to show how certain pathological changes in one bone can also involve adjacent metacarpals or phalanges. By addressing these general issues now, we can avoid the repetitiveness of listing them in later sections that deal with specific bones in the hand.
Normal Findings
During Growth
The ossification processes in the metacarpals and phalanges are subject to interindividual, sex-specific, and ethnic variations, especially with regard to the times at which the ossification centers appear and the growth plates become fused. These variations are beyond our scope, but Fig. 2.1 shows the most common sequence for the development of the ossification centers in the hand.
For questions pertaining to skeletal age, including the prediction of adult height (growth prediction), we refer the reader to radiographic atlases of skeletal development (e.g., Greulich and Pyle, Tanner and Whitehouse).
In Adulthood
Figure 2.2 shows the normal radiographic appearance of the adult hand, including the anatomic terms that will be used in the rest of the chapter.
All the metacarpals and phalanges are classified as small tubular bones, and they articulate via synovial joints. The size of the bones of the hand (length and width) depends chiefly on constitutional factors. The shape of the bones is determined mainly by the nature and extent of mechanical stresses. This is most evident at sites of tendon attachment: the stronger and more sustained the muscular traction, the larger and more prominent the bones appear. The bones of a manual laborer have a heavier, “stockier” appearance than those of an office worker (Fig. 2.3a,b).
In the normal hand, a line drawn tangent to the heads of the fourth and fifth metacarpals passes just above the head of the third metacarpal (Fig. 2.4). If the line intersects the head of the third metacarpal, this is a sign that a pathological condition (e.g., pseudohypoparathyroidism) is present. A tangent that just touches the articular surface of the third metacarpal is considered borderline.
Fig. 2.1 Typical progression of the radiographic appearance of epiphyseal ossification centers in the carpus, metacarpus, and phalanges.
The sum of the lengths of the proximal and distal phalanges should approximately equal the length of the associated metacarpal bone (the “phalangeal sign” of Kosowicz 1965, Fig. 2.4). An analysis of measurements of phalangeal lengths with metacarpophalangeal pattern profile plots (Poznanski and Holt 1971) has been extended by correlating the measurements with the total length of the phalanges to obtain a single mean-value and standard-deviation table for all ages from 3 years to adult. This table can be used to compare published pictures with actual radiographic images (Dijkstra 1983). The many possible causes of disproportionately short or long metacarpals and phalanges are discussed fully in the section on Specific Bones of the Hand.
Normally the thumb has three tubular bones and the other fingers have four. There are several reasons why fewer than the normal number may be encountered in one or more fingers:
• Absence of a joint (congenital: symphalangia; acquired: postarthritic ankylosis)
• Congenital absence of one or more phalanges
• Loss of one or more phalanges (e.g., loss of a distal phalanx due to neoplastic or inflammatory destruction)
Two sesamoid bones are found at the base of the proximal phalanx of the thumb in virtually 100% of the population, one occurring more toward the radial side of the thumb and one toward the ulnar side. These sesamoids become radiographically visible between 12 and 14 years of age. Another sesamoid occurs at the interphalangeal joint of the thumb in approximately 70–75% of the population and at the head of the fifth metacarpal in 82.5% (Fig. 2.5).
Fig. 2.2 Normal radiographic appearance of the adult hand, with anatomic nomenclature.
1
Trapezium
2
Trapezoid
3
Capitate
4
Hamate
5, 5a
Triquetrum and pisiform, superimposed
6
Lunate
7
Scaphoid
8
Metacarpal bones
9
Proximal phalanges
10
Middle phalanges
11
Distal phalanges
12
Sesamoid
CMG
Carpometacarpal joint
DEG
Interphalangeal joint of thumb
DGG
Metacarpophalangeal joint of thumb
DSG
Carpometacarpal joint of thumb
DIP
Distal interphalangeal joint
IMG
Intermetacarpal joint
MCP
Metacarpophalangeal joint
PIP
Proximal interphalangeal joint
Fig. 2.3 a–d The diverse radiographic anatomy of the hand. a, b Mechanical stresses influence the size and shape of the hand bones. Film a is from an office worker, film b is from a manual laborer. In b, note the protuberant ligament and capsular attachments and the prominent nutrient canals, especially in the proximal phalanges. c, d Radiographs from a healthy 37-year-old woman show very dense, thick cortical bone in the metacarpals and osteosclerosis of the distal phalanges (the patient had no clinical signs of Morgagni syndrome).
Supernumerary sesamoid bones may be encountered. They have no pathological significance (Figs. 2.5–2.7).
In principle, single or multiple sesamoid bones can occur at various metacarpophalangeal and interphalangeal joints and may even be found dorsal to the metacarpophalangeal joint of the thumb. When a sesamoid is found at an unusual location and is symptomatic, the differential diagnosis should include a fragment from an adjacent bone, heterotopic bone formation, and the ossification of a soft-tissue tumor (e.g., chondroma, soft-tissue osteoma). The presence of differentiated cancellous bone structures with a cortical margin generally identifies the bone as a sesamoid. A sesamoid that completely overlaps a bony structure such as the head of a metacarpal is indistinguishable from an innocuous bone island (endosteoma), but neither one has pathological significance.
The radiographic density of the bones of the hand depends on the thickness of the cortical bone and the thickness and density of the cancellous trabeculae. Rarefaction of the cancellous trabeculae and thinning of the cortical bone are important signs of osteopenia. The Barnett-Nordin index, formerly used to diagnose osteoporosis, is a useful guide for determining the normal thickness of the cortical bone.
Barnett-Nordin index
Ratio of cortical thickness to total transverse diameter at the midpoint of the second metacarpal bone.
Fig. 2.4a,b Biometry of the metacarpals and phalanges.
a
Phalangeal sign of Kosowicz.
b
Metacarpal sign.
E
Distal phalanx
G
Proximal phalanx
M
Middle phalanx
MK
Metacarpal
Fig. 2.5 Sesamoid bones that have been described in the adult human hand (after Degen). Sesamoids are always found at the metacarpophalangeal joint of the thumb. The prevalence of the more common sesamoids is shown. The less common sesamoids are marked with the letter S (sporadic occurrence). Only one case has been observed and described for each of the distal interphalangeal sesamoids.
This index expresses the thickness of the cortex as a percentage of the total bone diameter and should average at least 43–44% in healthy adolescents and adults. The cortical thickness of all the metacarpals and phalanges declines slowly and steadily with aging, decreasing earlier in women than in men. Meanwhile, the cancellous bone undergoes a progressive rarefaction that is especially pronounced near joints. As a result, the bones become more radiolucent. Normally the cortex of the metacarpals and phalanges appears very solid and uniformly dense. The endosteal margin of the cortex may show slight undulations, but these have no pathological significance. The cortex of the metacarpals is sometimes very thick and dense and may greatly narrow the marrow space without pathological implications (Fig. 2.3c, d). Similarly, osteosclerosis of the distal phalanges and cortical thickening of individual phalanges do not necessarily have pathological significance (Fig. 2.3c, d). Occasionally, however, these hyperostotic changes may be associated with hyperostosis frontalis interna and endocrine disorders, especially in women 40 to 50 years of age (Morgagni syndrome). They may also be a manifestation of skeletal sarcoidosis or other diseases. “Roughening” of the cortical boundary and intracortical bone resorption always signify an abnormal structural change that may result from a metabolic disorder (e.g., hyperparathyroidism) or a regional increase in blood flow due to a pathological process. Fraying of the cortex or intracortical channels can result from dilation of the normally invisible Haversian canals (Figs. 2.43, 2.44). If this process occurs at a circumscribed site in the cortical bone, it produces a “gray cortex” sign like that seen with stress fractures, for example. If the inner cortical margin becomes poorly demarcated from the medullary canal, this may result from an incipient sclerotic process within the medullary cavity.
Fig. 2.6 Multiple sesamoids.
Linear Lucencies
Linear radiolucencies in the tubular bones of the hand can have two causes:
• Nutrient canals
• Projection-related lucencies
Nutrient canals in the metacarpal bones (Figs. 2.8b, 2.9c) run obliquely from the cortex to the medullary cavity in a distal-to-proximal direction. The nutrient canals in the phalanges show an opposite orientation, running in an oblique proximal-to-distal direction (Figs. 2.3b, 2.8b). This disparity results from differences in the longitudinal growth of the bone and of the vessels that traverse the canals. Longitudinal growth of the metacarpals occurs mainly in the distal portion of the bone, causing the metacarpal head to grow distally away from the proximal nutrient canals. By contrast, longitudinal growth of the phalanges occurs in their proximal portion, causing the bone to grow in a proximal direction away from the distal, more slowly developing vessels. A nutrient canal projected end-on appears as a small round lucency that, when viewed with a magnifier, is frequently surrounded by a dense rim (Figs. 2.8a, 2.10).
Projection-related linear lucencies are commonly found at sites where tendons attach to bony prominences. The grooves that flank the prominence and separate it from the adjacent cortex create a translucent effect (Fig. 2.9a-c).
Small, irregular densities ("calcium specks") found in areas of the metacarpals and phalanges with abundant cancellous bone are a summation effect caused by superimposed cancellous trabeculae and have no pathological significance (Fig. 2.10). Often they can be eliminated by changing the angle of the projection by a few degrees.
Fig. 2.7 Two normal and two rudimentary sesamoids at the metacarpophalangeal joint of the thumb.
Fig. 2.8a,b Nutrient canals in the metacarpals and phalanges. a End-on projection of a nutrient canal (arrow). b Course of the nutrient canals. Note howthe orientation of the metacarpal canals differs from that in the proximal phalanges.
Fig. 2.9a–c Causes of linear lucencies on the phalanges: nutrient canals and bony prominences. a Palmar aspect of a phalanx shows a bony prominence (for tendon attachment) flanked by groovelike depressions on each side. b Clear projection of a bony prominence with a slight peripheral overhang (arrow) that mimics a fracture line. c Lucency created by the base of a groove flanking a bony prominence and by a nutrient canal (arrow: point where the vessel enters the cortex).
Fig. 2.10 The arrow points to a “calcium speck” caused by superimposed trabecular lines. It happens to be adjacent to a nutrient canal projected end-on. The white arrow points to a normal area of “thin bone” that should not be mistaken for cortical erosion.
Pathological Finding?
Normal Variant or Anomaly?
While we cannot detail the many complex and diverse skeletal malformations and deformities that can occur in the hand, we can discuss variants, including extreme ones, and illustrate clear-cut malformations that are encountered in radiological practice. Table 2.1 shows the classification and relative frequency of skeletal malformations of the hand according to Swanson (1976) and Lister (1993).
The tubular bones of the hand are normally mono-epiphyseal. Usually the epiphyses are somewhat narrower than the adjacent metaphyses, but they may also be of equal width or even slightly broader (Fig. 2.11).
Epiphyses that are large and cone-shaped and have irregular margins may reflect an enchondral epiphyseal ossification disturbance (Fig. 2.12), but in these cases they are generally associated with epiphyseal abnormalities in the long tubular bones and in the skeleton of the foot.
Malformations
Frequency (%)
Failure of formation of parts
12.2
Failure of differentiation of parts
31.3
Duplication
35.9
Overdevelopment
0.5
Underdevelopment
4.3
Ring constriction complex
6.5
Malformation syndromes
Variable
Fig. 2.11 Broad epiphyses in a 14-year-old boy.
Fig. 2.12 Very stout, broad epiphyses in cleidocranial dysostosis. Note the pseudoepiphysis in the second metacarpal.
Fig. 2.13 These epiphyses appear small in relation to the metaphyses, especially in the phalanges.
Metaphyses that are broader than the epiphyses and diaphyses are illustrated in Fig. 2.13 as an anatomic variant.
The epiphyseal plates usually show slight distal convexity in the phalanges and slight proximal convexity in the metacarpals, but this pattern is subject to variation (Fig. 2.14) without pathological significance.
The course of the epiphyseal plates changes during skeletal growth.
Extra epiphyses are known as pseudoepiphyses, apparently because they do not contribute significantly to the longitudinal growth of the tubular bone (Figs. 2.15–2.17). One or more pseudoepiphyses may be found in normal children and adolescents, but they may also reflect a systemic disturbance of skeletal growth (e.g., in hypothyroidism or Down syndrome). Three basic histological patterns of pseudoepiphysis formation and development are listed below in chronological order (Ogden et al. 1994).
Fig. 2.14 Variants of epiphyseal lines in the metacarpals: transverse (left) and distally convex (right).
• A central osseous bridge extends from the metaphysis into the epiphysis, where it appears as a centrifugally expanding, mushroomlike ossification center. The remaining intact epiphyseal plate does not have the hypertrophic cartilage cell columns that are otherwise typical of the growth plate.
• A peripheral osseous bridge is formed, creating either an osseous ring or an eccentric bridge between the metaphysis and the epiphysis. Centrally, the physis is preserved.
• Multiple bridging occurs. As in the first and second patterns, the nonossified portions of the physis lack typical columns of cartilage cells.
These bridging phenomena cannot always be seen on radiographs, but the pathoanatomic and histological studies of Ogden et al. (1994) indicate that, visible or not, they probably exist.
Pseudoepiphyses are most commonly found between 5 and 10 years of age. They close years earlier than the normal epiphyseal growth plate in the same bone. As mentioned, they do not contribute to longitudinal bone growth.
Pseudoepiphyses are found in the proximal second metacarpal of 20–60% of normal children and in the distal first metacarpal of up to 65% of normal children.
Schäfer (1952) ranked the bones of the hand in the following order with regard to the frequency of pseudo-epiphyses:
Relative frequency of pseudoepiphyses according to Schäfer
First metacarpal > second metacarpal > fifth metacarpal > fifth middle phalanx > third metacarpal > fourth middle phalanx > first proximal phalanx > fourth metacarpal.
Fig. 2.15 Pseudoepiphysis in the second metacarpal bone. It is unusual that this bone is slightly too long relative to the third metacarpal, but this apparently has to do with the hypoplastic thumb (missing proximal phalanx) and the extra epiphysis on the first metacarpal. Also, the scaphoid appears somewhat small. Note also the relatively dense epiphyses of the middle phalanges (ivory epiphyses, see p. 52).
Fig. 2.16 Pseudoepiphysis in the distal portion of the first metacarpal.
Fig. 2.17 Pseudoepiphysis in the proximal second metacarpal with the formation of an osseous bridge.
Rochels and Schmidt (1980) found pseudoepiphyses in 82.4% of patients with Down syndrome. Significant sex differences were not observed. The frequency of involvement is different from that in normal individuals:
Relative frequency of pseudoepiphyses in Down syndrome
Second metacarpal > first metacarpal > fifth middle phalanx > fourth proximal phalanx.
The authors counted an average of 3.1 pseudoepiphyses per hand in children with Down syndrome. Brachyme-sophalangia was found in 67% of cases, dysmesophalangia in 4.6%, and clinodactyly in 56.4%.
The cone-shaped epiphysis (cone epiphysis) is a special morphological variant (Fig. 2.18a-c). Cone-shaped epiphyses are more commonly found in the skeleton of the foot in otherwise healthy individuals (Giedion 1968). It has been suggested that the condition is based on a disturbance in the timing and coordination of bone development. While the central portions of the bone become arrested in their growth, the peripheral portions continue to grow. Occasionally, though, cone-shaped epiphyses may be associated with clinical symptoms as illustrated by the case in Fig. 2.18d,e. Apparently, the cone-shaped epiphyses in such cases signal a true deformity or trophic disturbance.
Fig. 2.18a–e Cone-shaped epiphyses. a Cone-shaped epiphyses of the second and fifth middle phalanges on both sides (right side not shown). b Cone-shaped epiphyses of the second and fifth middle phalanges on both sides (left side not shown). c Pronounced cone-shaped epiphyses of all middle phalanges. The opposite hand showed the same changes with an otherwise normal appearance in a healthy 11-year-old child. d,e Cone-shaped epiphyses on the proximal phalanx of the thumbs and the second and third middle phalanges of both hands. Also relatively dense epiphyses, especially on the third and fourth proximal phalanges of the right hand. This 14-year-old Arabic boy presented clinically with visible swellings (and mild pain) affecting the thumbs and the proximal interphalan-geal joints of the index and small fingers.
Very dense epiphyses occurring as a normal variant are discussed in the section on necrosis (p. 52).
In contrast to cone-shaped epiphyses, the presence of a delta phalanx, known also as a longitudinally bracketed diaphysis (Fig. 2.19), represents a pathological condition of the metacarpals (and metatarsals) and phalanges, most commonly involving the proximal phalanges of the hands and feet (Theander and Carstan 1974, Ogden et al. 1981, Theander et al. 1982).
Fig. 2.19a,b Delta phalanges. a Delta-shaped proximal phalanx of the thumb and duplication of the distal phalanx in a 3-year-old girl. Note the distal epiphysis on the first metacarpal. b Delta-shaped proximal phalanx of the fourth finger of the left hand in a 3-year-old boy, resulting in shortening of that ray. Clinically, the patient had syndactyly of the third and fourth fingers and consequent or associated clino-dactyly of the small finger.
Fig. 2.20a,b Symphalangia of all proximal interphalangeal joints in a one-day-old infant. The finding is unmistakable in the small finger but is easily missed in the second and third fingers unless the narrow spaces between the proximal and middle phalanges are noted. The “spaces” themselves represent the proximal epiphyseal growth plates and the still-unos-sified epiphyses. The child's mother (Fig. 2.21) had the same changes (case courtesy of Professor Dr. D. Buck-Gramcko, Hamburg).
In the literature to date, delta phalanges have been described in the following skeletal dysplasias and syndromes:
• All forms of microphalangia, polydactyly, and syndactyly
• Trisomy 21 (fifth middle phalanx)
• Acrocephalosyndactyly (Apert and Pfeiffer type)
• Rubinstein-Taiby syndrome (thumb)
• Catel–Manzke syndrome (second and third fingers)
• Holt–Oram syndrome
• Otopalatodigital syndrome
• Otofaciogenital syndrome
• Diastrophic dwarfism
• Nievergelt syndrome
• Hand–foot–genital syndrome (Giedion)
Symphalangia refers to the absence of the interphalangeal joints with resultant end-to-end fusion of the phalanges (Figs. 2.20, 2.21). This condition is classified as a hereditary dysplasia. In adults