79,99 €
Mehr erfahren.
- Herausgeber: Thieme
- Kategorie: Fachliteratur
- Sprache: Englisch
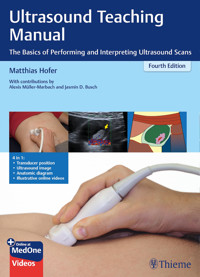
Step by Step to Proficiency in Diagnostic Ultrasound
This workbook is divided into lessons that guide you—like an instructor in an ultrasound course—systematically through the individual organ systems and body regions.
Key features of the fourth edition:
- Special multiple-exposure photos demonstrate the dynamics of handling the transducer
- Triplet-image units vividly illustrate transducer positioning, the ultrasound image, and relevant anatomy
- Reference numbers on the accompanying diagrams help you to both actively develop your knowledge and to test it at any time. The legend located on the back cover flap is the key to the reference numbers that are used consistently in each diagram.
- Quiz images at the end of each chapter are the perfect tool for rigorous self-evaluation
- Physical fundamentals are presented in vibrant, illustrative diagrams
- Numerous practical tips and tricks make it easy to familiarize yourself with ultrasound
- A primer on ultrasound interpretation explains specialized terminology concisely and clearly
- Precise descriptions of algorithms for transducer positioning facilitate real-time examinations
Videos (online access) showing relevant ultrasound anatomy, optimal transducer positioning, and the images you will see on the monitor during examination let you experience the content live—a perfect complement to the book that will greatly improve your retention of the material.
This book includes complimentary access to a digital copy on https://medone.thieme.com.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 322
Veröffentlichungsjahr: 2020
Ähnliche
The Most Important Planes in Abdominal Ultrasound
In this book, the point at the end of the position mark on the transducer corresponds to the right edge of the respective image. Think about which organs will be visualized in which respective imaging plane. To find the solutions, fold this page out and look on the back.
Standard Planes with Appropriate Transducer Position and Drawing Templates
Ultrasound Teaching Manual
The Basics of Performing and Interpreting Ultrasound Scans
Fourth expanded and revised edition
Matthias Hofer, MD, Associate Professor, MPH, MME (Univ. Bern)Director of Education at the University Institute of Diagnostic, Interventional and Pediatric Radiology (DIPR)Dept. Head: Univ.-Prof. Johannes Heverhagen, MD, Inselspital Bern, Bern University, Switzerland
With Ultrasound Images from:
Alexis Müller-Marbach, MDHead of Dept. of Gastroenterology, Hepatology and Palliative CareHelios Hospital Niederberg, Germany
Jasmin D. Busch, MD, Associate ProfessorSection Head of Pediatric Radiology, Inselspital Bern, Bern University, Switzerland
930 Images
Library of Congress Cataloging-in-Publication Datais available from the publisher.
This book is an authorized translation of the 10th German edition published and copyrighted 2020 by Georg Thieme Verlag, Stuttgart.Title of the German edition: Sono-Grundkurs
Translator: John GrossmanIllustrators: Dr. Willi Kuhn, Ramona Sprenger
© 2021 Georg Thieme Verlag KG
Georg Thieme Verlag KGRüdigerstrasse 14, 70469 Stuttgart, Germany+49 [0]711 8931 421, [email protected]
Thieme Publishers New York333 Seventh Avenue, New York, NY 10001, USA+1-800-782-3488, [email protected]
Thieme Publishers DelhiA-12, Second Floor, Sector-2, Noida-201301Uttar Pradesh, India+91 120 45 566 00, [email protected]
Thieme Publishers Rio, Thieme Publicações Ltda.Edifício Rodolpho de Paoli, 25º andarAv. Nilo Peçanha, 50 – Sala 2508Rio de Janeiro 20020-906 Brasil+55 21 3172 2297 / +55 21 3172 1896
Cover design: Thieme Publishing GroupTypesetting by Ramona Sprenger, Colognewww.einraumapartment.dePrinted in Germany byDruckerei Steinmeier, Deiningen
DOI 10.1055/b000000431
ISBN 978-3-13-243760-9 5 4 3 2 1
Also available as an ebook:eISBN (PDF): 978-3-13-243761-6eISBN (ePub): 978-3-13-243762-3
Important note:
Medicine is an ever-changing science undergoing continual development. Research and clinical experience are continually expanding our knowledge, in particular our knowledge of proper treatment and drug therapy. Insofar as this book mentions any dosage or application, readers may rest assured that the authors, editors, and publishers have made every effort to ensure that such references are in accordance with the state of knowledge at the time of production of the book.
Nevertheless, this does not involve, imply, or express any guarantee or responsibility on the part of the publishers in respect to any dosage instructions and forms of applications stated in the book. Every user is requested to examine carefully the manufacturers’ leaflets accompanying each drug and to check, if necessary in consultation with a physician or specialist, whether the dosage schedules mentioned therein or the contraindications stated by the manufacturers differ from the statements made in the present book. Such examination is particularly important with drugs that are either rarely used or have been newly released on the market. Every dosage schedule or every form of application used is entirely at the user’s own risk and responsibility. The authors and publishers request every user to report to the publishers any discrepancies or inaccuracies noticed. If errors in this work are found after publication, errata will be posted at www.thieme.com on the product description page.
Some of the product names, patents, and registered designs referred to in this book are in fact registered trademarks or proprietary names even though specific reference to this fact is not always made in the text. Therefore, the appearance of a name without designation as proprietary is not to be construed as a representation by the publisher that it is in the public domain.
This book, including all parts thereof, is legally protected by copyright. Any use, exploitation, or commercialization outside the narrow limits set by copyright legislation, without the publisher’s consent, is illegal and liable to prosecution. This applies in particular to photostat reproduction, copying, mimeographing, preparation of micro-films, and electronic data processing and storage.
To access the additional media content available with this e-book via Thieme MedOne, please use the code and follow the instructions provided at the back of the e-book.
Contents
Standard planes (front cover flap)
Physical principles
Image generation, sound transmission, reflection
Echogenicity, frequency ranges
Operation and features of ultrasound units
Selection of ultrasound units, types of transducers
New techniques
Panoramic imaging, 3D, Clarify Vascular Enhancement
Harmonic imaging, phase inversion,
Contrast agents
Ultrasound CT
Pulse compression, precision upsampling
Diagnostic ultrasound catheter
Artifacts
Reverberation, section thickness, acoustic enhancement
Acoustic shadowing, mirror-image artifacts
Side-lobe artifact, quiz for assessing progress
Practical tips and tricks for the beginner
Lesson 1
Retroperitoneum, Sagittal plane
Anatomy
Upper retroperitoneum, normal findings
Lower retroperitoneum, normal findings
Aortic aneurysm
Right heart failure
Quiz
Lesson 2
Retroperitoneum, Transverse Plane
Anatomy
Normal findings
Age-related echogenicity
Acute pancreatitis, chronic pancreatitis
Pancreatic tumors
Retroperitoneal lymph nodes
Quiz
Lesson 3
Porta Hepatis, Gallbladder, Biliary Tract
Anatomy
Porta hepatis
Normal findings
Portal hypertension
Portal vein thrombosis, lymph nodes
Gallbladder
Cholecystitis
Differential diagnosis of cholecystitis
Gallstones
Gallbladder polyps, cholestasis
Biliary tract
Lesson 4
Liver
Anatomy of the segments of the liver
Sagittal plane, organ size, lateral angle
Transverse plane, hepatic veins
Right heart failure
Normal variants, fatty liver
Focal fatty infiltration, focal sparing in fatty infiltration
Cysts, echinococcosis (CE)
Echinococcosis (CE), hepatic hemangiomas
Focal nodular hyperplasia (FNH)
Cirrhosis of the liver
Hepatocellular carcinomas, liver abscesses
Liver metastases, hypervascular metastases
Hypovascularized liver metastases
Quiz
Lesson 5
Kidneys, Adrenal Glands, Renal Transplants, Spleen
Anatomy of the kidneys and adrenal glands
Normal findings
Normal variants, renal cysts
Kidney degeneration, nephritis
Urinary obstruction
Differential Diagnosis of Urinary Obstruction
Renal calculi, renal infarction
Benign renal tumors, malignant renal tumors, adrenal tumors
Normal findings
Determining the size of a renal transplant, lymphoceles
Spleen
Anatomy, examination technique
Spleen size, splenomegaly
Splenomegaly, splenic infarcts, practical suggestion
Lymphomatous infiltration, splenic hematomas, hyperechoic lesions, splenic cysts
Quiz
Lesson 6
Thyroid Gland, Lymph Nodes, Gastrointestinal Tract
Anatomy, volumetric measurements, normal values
Normal findings
Goiter
Focal solid nodules, thyroiditis
Lymph nodes
Neck: lymph nodes
Differential diagnostic criteria, perfusion parameters
Differential diagnostic criteria, reactive inflammatory
Retroperitoneal lymph nodes
Gastrointestinal tract
Anatomy, wall layers
Gastric tumors
Crohn’s disease
Intestinal intussusception, hernias, contrast enema
Wall thickening, diarrhea, appendicitis
Fecal impaction, colitis, colon carcinoma
Diverticulitis
Quiz
Lesson 7
Bladder and Reproductive Organs
Anatomy
Bladder
Examination technique, determining postvoiding residual bladder volume
Indwelling catheter and differential diagnosis of cystitis, wall thickening, internal echoes and sedimentation, ureteral peristalsis
Reproductive organs
Prostate and testis
Undescended testis, orchitis, hydrocele
Endovaginal ultrasound, image orientation
Uterus: normal findings
Uterine tumors
Ovaries: volume, menstrual cycle phases
Ovarian cysts and tumors
Pregnancy testing
Placenta position and gender determination
Quiz
Lesson 8
FAST, eFAST, Lung, FAST algorithm eFAST algorithm
Seashore sign, barcode sign
Lung mobility, pulmonary pulse
Lung point in pneumothorax
Pleura
Quantifying pleural effusions
Pleuritis, empyema, mesothelioma
Ribs
Costal fractures, costal metastases
Lung
Pneumonia, pulmonary infarct, bronchial carcinoma
Quiz
Lesson 9
Pediatrics
Skull and central nervous system
Anatomy of the CSF spaces
Normal findings in the sagittal plane
Normal variants
Normal findings in the coronal plane
Cerebral hemorrhage
Hydrocephalus
Spinal canal
Hip
Preparation and positioning
Normal findings
Setup and measurement errors
Graf’s classification of Infant Hips
Kidneys, Bladder, Spleen
Kidneys in newborns
Diffusely increased echogenicity, nephrocalcinosis
Urinary obstruction and reflux
Urinary obstruction, voiding cystourethrogram
Renal and adrenal tumors
Urachus, ureterocele, spleen size
Gastrointestinal tract
Pyloric hypertrophy, reflux, Hirschsprung’s disease
Appendices
Primer of Ultrasound Findings
Index
Template for Report of Normal Findings
Template for Report of Normal Findings
Answers to Quizzes
Thanks to Contributors, Hands-on Ultrasound Courses
List of Abbreviations
Examination Algorithms
References
Space for Your Notes and Drawing Exercises
Where Do I Find Which Chapter?
Physical Principles
Lesson 1
Retroperitoneum, Sagittal Plane
Lesson 2
Retroperitoneum, Transverse Plane
Lesson 3
Porta hepatis, Gallbladder, Biliary Tract
Lesson 4
Liver
Lesson 5
Kidneys, Adrenal Glands, Renal Transplants, Spleen
Lesson 6
Thyroid Gland, Lymph Nodes, Gastrointestinal Tract
Lesson 7
Bladder and Reproductive Organs
Lesson 8
FAST, eFAST, Lung
Lesson 9
Pediatrics
Appendices
Tips for the Reader
How can you best profit from this book?
How can you use this manual optimally?
As you work through the individual chapters, you can benefit from several methodical and didactic features.
Find it quickly …
• Find a chapter: You will find the respective tab for each chapter on page 5.
• Find tough quiz questions for in-depth study.
• Find cross-referenced figures: The figures are numbered according to the page on which they appear. For example, Fig. 115.2 is on page 115.
• Find an explanatory figure or diagram supplementing the text. They are highlighted in the accompanying text in color and are almost always on the same page, eliminating the need to page through the book looking for them.
• Find numbered structures. Their reference numbers appear in bold in the accompanying text or on the back cover flap (the same number for each structure is used throughout the entire book).
• Find keywords on page 148 (or on pages 4-6).
• Find for each structure normal values and checklists. These are also provided on laminated, water-resistant, pocket-sized cards.
Why we call this book a “workbook”?
A unique feature of this book is that you can use each page as a quiz to test your knowledge. The diagrams contain reference numbers instead of labels. This means you can go through the material a second time and use any figure to test which structures you know and which you still have to learn. The quiz questions and drawing exercises have a similar purpose. In this way, you can become familiar with several efficient study methods that allow you to integrate new material into your long-term memory faster – even though this requires you to take a more active approach to learning. Not only do I wish you good luck with this course, I also hope you have fun doing it!
Matthias Hofer, MD, Associate Professor, MPH, MME, Summer 2020Director of Education at the University Institute of Diagnostic, Interventional and Pediatric Radiology (DIPR) Inselspital Bern, Bern University, Switzerland
What does the respective color coding mean in the diagrams?
Introduction
Physical Principles and Technical Fundamentals
New Techniques
Artifacts
Quiz
Practical Tips and Tricks for the Beginner
Physical Principles and Technical Fundamentals
Image Generation
Ultrasound images are generated not by X-rays but by sound waves that are sent by a transducer into the human body and reflected there. In abdominal ultrasound, the frequencies used generally are between 2.5 and 5.0 megahertz (MHz; see p. 11). The primary condition required for sound wave reflections is the presence of so-called “impedance mismatches.” These occur at the interface between two tissue layers with different sound transmission properties (interfaces in Fig. 8.1). It is interesting to note that different soft tissues show only minor differences in the transmission speed of sound (Table 8.1).
Only air and bone are marked by massively different sound transmission in comparison with other human tissue. For this reason ultrasound units can be operated at a preselected medium frequency of approximately 1540 m/s without producing any major inaccuracies in the calculated origin (”depth”) of the echo.
The processor computes the depth of origin of the echo from the time difference detected between emission of the sound impulse and return of the echo.
Echoes from tissue close to the transducer (A) arrive earlier (tA) than echoes from deeper tissues (tB, tC in Fig. 8.1a). The mean frequency is strictly theoretical since the processor cannot know which type of tissue the sound waves traversed.
Table 8.1
Fig. 8.1ab
Which Component of the Sound Wave is Reflected?
Fig. 8.1a shows on the left three tissue blocks traversed by sound waves that differ only minimally in their transmission velocity (indicated by similar gray values). Each interface only reflects a small portion of the original sound waves () as echo (). The right–hand diagram shows a larger impedance mismatch at the interface A between the different tissues (Fig. 8.1b). This increases the proportion of reflected sound waves () in comparison to the tissues shown on the left. However, what happens if the sound waves hit air in the stomach or a rib? This causes a so-called “total reflection,” as illustrated at interface B in Fig. 8.2b: The transducer does not detect any residual sound waves deep to this structure from which it can generate an image. Instead, the total reflection creates an acoustic shadow (45).
Conclusion:
Intestinal or pulmonary air and bone are impenetrable by sound waves, precluding any imaging deep to these structures. The goal will later be to work around intestinal air or ribs by maneuvering the transducer. The pressure applied to the transducer against the abdominal wall (see p. 21) and the acoustic gel that displaces air between the surface of the transducer and the patient’s skin (see p. 22) play a significant role.
From a “Snowstorm” to an Image …
Do not get discouraged if at first you can only make out a blinding “snowstorm” on ultrasound images. You will be surprised how soon you will learn to recognize the ultrasound morphology of individual organs and vessels. Fig. 8.2 visualizes the gallbladder (14) as a black structure and shows two round polyps (65) within it. The surrounding gray “snowstorm” corresponds to the hepatic parenchyma (9) which is traversed by hepatic vessels (10, 11). How can you quickly work out which structures in the image appear bright and which are dark? The key lies in the concept of echogenicity (see p. 9).
Fig. 8.2a Gallbladder with polyps b
What Does the Term “Echogenicity” Mean?
Please use the following terms:
These fluids are anechoic (= black):
Hyperechoic (= bright)
pericardial or pleural effusion,
Hypoechoic (= dark)
ascites, cysts, blood, urine, bile,
Anechoic (= black)
cerebrospinal fluid
This is due to the lesser density of fat in comparison with normal liver tissue. On ultrasound the fatty deposits produce more impedance mismatches (Fig. 9.1c) than in normal liver tissue (Fig. 9.1d). Consequently, a fatty liver appears more echogenic (brighter) on ultrasound despite its significantly lower physical density.
A common misunderstanding:
What do ultrasound examiners mean when they refer to a “dense liver”? Either they are not expressing themselves clearly or they have failed to grasp the fundamental principle of ultrasound imaging and how it differs from radiography. Ultrasound does not visualize physical tissue densities but differences in sound transmission (impedance mismatches) which are unrelated to density.
Fig. 9.1a CT: Fatty liver b CT: Normal liver c Ultrasound: Fatty liver d Ultrasound: Normal liver
Generation and Frequency Ranges of Sound Waves
Sound waves are generated by the reverse “piezoelectric effect.” The pressure waves of an echo distort crystals, causing them to emit an electrical impulse. The reverse takes place during transmission. A transducer includes many such crystals. Depending on the impulse applied, they can produce sound waves of various frequencies specified in megahertz (MHz). A “3.75–MHz” transducer does not exclusively emit pressure waves (sound waves) at a frequency of 3.75 MHz. That is merely the specified median frequency (= “center frequency”). In fact, such a transducer may emit sound wave frequencies between, for example, 2 and 6 MHz. So-called “multi frequency transducers” have the additional capability to increase or decrease this center frequency and the surrounding bandwidth of transmitted sound frequencies. In thin patients or children, for instance, the bandwidth can be shifted (say 4–8 MHz with a center frequency of 6 MHz) to achieve better spatial resolution. However, this decreases the depth penetration of the sound waves.
In very obese patients, the use of lower frequencies (1–5 MHz with a center frequency of 2.5 MHz) can be appropriate to achieve the necessary penetration, but at the cost of lower resolution (see p. 11). Newer methods base their image generation on frequency shifts or harmonic frequencies of the echo in relation to the original ultrasound impulse (see p. 13).
Operating an Ultrasound Unit
Many controls on different ultrasound units are quite similar in function and arrangement regardless of the manufacturer. Therefore this section will look at the console of one unit supplied by Samsung (Fig. 10.1), which will then be used to introduce common technical terms.
Selection of Transducer and Preset
After you have switched on the unit (A) and it has booted, select the appropriate preset (PS) and the appropriate transducer for the respective examination and enter the current patient data (PD). You will usually select a linear array transducer (L) for evaluating the thyroid gland and the extremities but a convex array transducer (C) for abdominal examinations. The sector transducer (E) is used primarily in echocardiography, and the endovaginal transducer (G) is used for gynecologic examinations.
Selecting the Image Mode, Gain, and Focus
Usually you will begin with “normal” black and white or B-mode ultrasound (B), before later possibly switching to color-coded imaging (C). If you also wanted to obtain a flow profile from a blood vessel, you would then activate the Doppler mode (D) as well. This unit is equipped with control knobs that increase the respective signal (gain) of the active imaging mode when turned clockwise and reduce it when turned counterclockwise. The amplification (gain) can also be adjusted using the depth gain compensation feature (G). The transducer angle (A) must also be entered to determine flow velocities in Doppler mode. If you wish to display the change in a line of the image over time, switch to M-mode (MM). You can also set the specific depth range that is to have the best spatial resolution; here you use a toggle switch to set one or more focal zones (FZ) in your penetration depth. A few units also have a CW Doppler (CW) that measures frequency shifts (= flow speeds) not by means of depth gain compensation but as the summation of all speeds over an entire line of the image.
Magnification and Zoom Function
Especially with smaller target structures, you can significantly increase your detection of pathologic changes by magnifying the target organ (Mag) organ or zooming (Z) certain parts of the image. One common feature on almost all units is the position of the freeze or stop button (St) in the lower right corner of the console. This freezes the moving image. It is recommended to rest one finger of your left hand lightly on this button during the examination to minimize delay in capturing a desired image.
Size and Distance Measurements
After freezing (St) you can retrieve individual images from digital storage with the cine loop function: To do so, turn the trackball (T) to the left to 9:00 o’clock and go back image by image until you reach the desired one. Depending on the manufacturer and preset, up to eight simple measurements (M) can be performed one after the other on the frozen image. Use the trackball (T) and the set button(S) to define the beginning and end positions of your measured distances. It may be helpful to switch to double image mode (2x) for comparative measurements in different planes. Right next to this on most units is another button for switching back to single image mode (1x). More complex measurements such as volume measurements or flow indexes can be accessed with the measurement program (MP).
Helpful Extras
When you want to explain the imaging findings to the patient or a colleague, it is helpful to activate a pointer (P) which you can move across the frozen image with the trackball (T) to point out the findings you are explaining. If you really want to score points with your patients, install an additional monitor below the ceiling in their field of view. Well equipped units also offer automatic image optimization (QS), several hot keys for frequently used settings (P1-P3), and also several transducer sockets (SP) spare you the time and hassle of plugging and unplugging probes.
Fig. 10.1 Console and keypad
Selection of Ultrasound Units
In addition to large color Doppler units, ultrasound units with connections for several multi frequency transducers have proven especially useful in a hospital setting. Such mobile units are easily moved from the ultrasound suite to the ward or intensive care unit (Fig. 11.1).
The most important precaution when transporting the unit is to make sure that transducers are safely stowed so that dangling cables cannot become caught on doorknobs, gurneys, etc. A transducer that falls on the floor can easily represent a loss of €3000–7000 ($3300–7700) depending on the model. For the same reason, the transducer should never be left unattended on the patient’s abdomen when the examination is interrupted, for instance by a telephone call. Stowing the transducer in the frame with the cable hanging avoids unnecessary kinking that can lead to broken conductors in the cable.
Types of Transducers
Of the many types of transducers, only the three most important ones will be discussed here (endovaginal transducers, see p. 103).
A linear array transducer or “parallel scanner” emits parallel sound waves into the tissue and produces a rectangular image (Fig. 11.2a). The width of the image and the number of scan lines remain constant at all tissue levels. Linear array transducers have the advantage of good near-field resolution and are primarily used with high frequencies (5.0–10.0 MHz or higher) for evaluating soft tissue and the thyroid gland. Their disadvantage is the large contact surface. This can lead to air gaps between skin and transducer when it is applied to a curved body contour (loss of acoustic coupling). Further-more, acoustic shadowing (45) caused by ribs, lungs, or intestinal gas can greatly degrade image quality. Consequently, linear array transducers are rarely used for visualizing abdominal organs.
A sector transducer produces a fanlike image that is narrow near the transducer and increases in width with deeper penetration (Fig. 11.2b). This type of transducer has become established primarily in cardiology with lower frequencies (2.0–3.0 MHz) allowing deeper penetration. Due to the fanlike propagation of the sound waves, the heart can be well visualized through a small intercostal window without acoustic shadows from the ribs. The disadvantages of this type of transducer are their poor near-field resolution and decreasing line density in the far field with correspondingly decreasing resolution. Moreover, finding the desired imaging plane is difficult and takes some practice.
A curved or convex array transducer is a combination of the two types described above (Fig. 11.2c). The shape of the monitor image resembles a coffee filter and combines good near-field resolution with relatively good far-field resolution. The major advantage of the slightly curved contact surface is its ability to displace interfering intestinal air outside the imaging plane by applying increasing pressure (see p. 21). With this type of transducer, however, one has to accept decreasing resolution with increasing depth and, in certain locations, acoustic shadowing behind the ribs. This type is usually used in abdominal ultrasound with center frequencies from 2.5 MHz (in very obese patients) to 5.0 MHz (in slender patients).
The average frequency (center frequency) is usually 3.5–3.75 MHz. Memory aid: The higher the frequency, the better the resolution and the worse the penetration. The best way to remember this is to compare it to that loud music from your neighbor’s apartment. Which tones best penetrate even thick walls? The basses. These lower frequencies travel farther (i.e., penetrate deeper), see page 9.
Fig. 11.1
Fig. 11.2abc
New Techniques
Panoramic Imaging (SieScape®)
New high-performance image processors generate extensive ultrasound images from data acquired as the examiner moves the transducer slowly and continuously over the region of interest. With some practice, the examiner can produce impressive and undistorted images that allow distance measurements accurate to within 1–3% even on a curved body surface. Fig. 12.1 shows a sagittal scan with massive pleural effusion (69), compressive atelectasis of the lung (47), and, inferior to the liver (9), anechoic ascites (68) that appears to inundate the small bowel (46).
Fig. 12.2 impressively illustrates the position of the placenta (94) relative to the fetus. The high contrast resolution even allows evaluation of the interface between the fetal liver (9) and heart (114).
Fig. 12.1
Fig. 12.2
(With kind permission of Drs. C.F. Dietrich and D. Becker, from Farbduplexsonographie des Abdomens, Schnetztor-Verlag, Konstanz, Germany)
3-D Visualization
Especially in obstetrics, the three-dimensional visualization of fetal facial features improves the diagnosis of malformations such as cleft lip and palate. This technique can now visualize the physiognomy of the fetal skull with amazing accuracy (Fig. 12.3).
Of course, conventional cross-sectional imaging techniques can also detect skeletal and other malformations, albeit less impressively and clearly than three-dimensional ultrasound.
Fig. 12.3
Clarify Vascular Enhancement Technology
This technique is based on an algorithm that is able to significantly reduce the blurring on B-mode scans resulting from partial volume or section thickness artifacts. Flow information from the power Doppler mode is used, which helps to improve the spatial resolution of vascular contours on the B-mode image.
The result is significantly improved visualization of findings such as the contours of hard and soft plaque in the carotid arteries (Fig. 12.4b) compared with the visualization achieved by the conventional technique shown in Fig. 12.4a. It also facilitates evaluation of peripheral vascular rarefaction in the liver as the lumens of the hepatic veins and portal venous branches are more clearly visualized in the hepatic parenchyma (Fig. 12.5).
Fig. 12.4a “Normal” image of the carotid artery … b … with Clarify
Fig. 12.5 Hepatic vessels
The material on the following five pages is not an absolute prerequisite for the first practice sessions and can be skipped. Beginners may prefer to move from here directly to the preparations for Lesson 1 (see p. 21). After some initial practice they should return to these pages to reinforce their fundamental understanding of ultrasound imaging.
Tissue Harmonic Imaging (THI): This technique does not use the fundamental frequency of the original ultrasound impulse but their harmonics, integer multiples of the fundamental frequency (for example 7.0 MHz for a fundamental frequency of 3.5 MHz). These harmonics increase with increasing penetration, but their amplitude (intensity) remains far less than that of the base signal. The advantage of these harmonics is that they hardly arise at all near the transducer, but only develop with increasing penetration depth (Fig. 13.1). Consequently, they are less affected by the major sources of scattered image noise, which occurs especially in the anterior abdominal wall. Why do harmonics develop only with increasing penetration depth? Ultrasound waves are distorted as they traverse tissues with varying acoustic properties. Their pressure waves compress and relax the tissue as they penetrate it. Compressed tissue increases the speed of sound. However, as the tissue relaxes, the speed decreases, causing the trough of the pressure wave to propagate more slowly. The resulting distortion of the wave form (Fig. 13.2) induces harmonics. This is a cumulative effect that increases with the depth of penetration. Consequently, the amplitudes of the harmonic frequencies initially increase with penetration depth until this increase is offset by general absorption (Fig. 13.1).
Fig. 13.1
Fig. 13.2
Second Harmonic Imaging: This technique uses only the doubled frequency of the base signal for imaging. To avoid any overlapping of the range of the fundamental frequency (Fig. 13.3a) a narrowband signal must be used to distinguish the stronger components of the fundamental frequency from the weaker components of the harmonic (Fig. 13.3b). However, the narrower bandwidth of the signal leads to a slight reduction in contrast and spatial resolution. In spite of these short-comings, this technique has markedly improved the detection of details (Fig. 13.4b) compared with conventional ultrasound imaging (Fig. 13.4a), especially in obese patients (whose abdominal wall produces excessive scattering).
Fig. 13.3
Fig. 13.4ab
Fig. 13.5a Linear b Nonlinear
If the echoes of both signals are added, the sum equals zero as long as the signal has not undergone any changes in the body. As a result, both fundamental frequency echoes are suppressed (Fig. 13.5a) whereas the second harmonic signal components are enhanced (Fig. 13.5b).
Fig. 14.2 depicts a case showing acoustic shadowing () deep to intrarenal calcifications (b) that are undetectable by conventional imaging (a). In addition, the renal cyst () appears better demarcated and can be classified as benign with greater confidence.
Fig. 14.1abc
Fig. 14.2ab
Fig. 14.3
Fig. 14.4
Contrast Enhancement
The echogenicity of blood and tissue can be enhanced with microbubbles with a diameter of 3–5 μm that pass through the capillaries and create more impedance mismatches within the blood stream (Fig. 14.3). So far, several contrast enhancement agents have been introduced and about 50 additional agents are under development. The contrast agent Levovist® consists of tiny air bubbles () about 3 μm in diameter (95% < 10 μm), which are stabilized with a thin envelope of palmitic acid (Fig. 14.4). They are initially bound to galactose microparticles that dissolve in the blood and release the microbubbles. The dry powder can be mixed by the examiner in different concentrations. The suspension passes through the pulmonary circulation, but is only injectable for about 8 minutes after preparation. Hypergalactosemia is a contraindication. Measuring just a few millimeters, the microbubbles are comparable in size to erythrocytes (Fig. 14.5), which explains how they are able to pass through the capillaries.
Ultrasound impulses with low sound pressure make these microbubbles vibrate at what is known as a low “mechanical index” of 0.05–0.2. Contrast images are created using the nonlinear resonance frequency exclusively. Alternatively, one can use a higher mechanical index around 1.0–1.5 to cause the microbubbles to burst and emit a significantly stronger signal (although only during a single passage). This is known as the burst method.
The contrast agent Sonovue® consists of an aqueous solution of sulfur hexafluoride (SF6) stabilized by a phospholipid layer (Fig. 14.6). The median size of the bubbles is about 2.5 μm (90% < 8 μm) with an osmolality of 290 mOsmol/kg. One possible advantage of this contrast agent is that the suspension remains stable for over 6 hours, allowing it to be used for several applications. The best results are achieved in conjunction with the tissue harmonic imaging (THI) technique, referred to as ”contrast harmonic ima-ging (CHI).” Frequently, the term contrast-enhanced ultrasound (CEUS) is also used.
A specific sound pressure causes the bubbles to vibrate and emit harmonic echoes. As a result, contrast harmonic imaging (Fig. 14.7b) can detect multiple liver metastases significantly better than noncontrasted imaging (Fig. 14.7a).
Fig. 14.5 Microbubbles
Fig. 14.6 Sonovue®
Fig. 14.7a Noncontrasted b CEUS
Spatial Compounding (SonoCT®T)
There is another technique for suppressing artifacts. “Real-time compound imaging” does not scan an image line by line (Fig. 15.1a), instead it scans from different angles and merges this data into an image in real time (Fig. 15.1b). Up to nine different slices can be scanned, allowing more precise visualization of tissue information. This is illustrated here by the morphology of arteriosclerotic plaque in the carotid artery ( in Fig. 15.2a) compared with conventional imaging (Fig. 15.2b).
Fig. 15.1ab
This technique has exhibited obvious advantages in ultrasound imaging of the breast and musculoskeletal system. Fig. 15.3b shows improved visualization of an entire biopsy needle () in the breast parenchyma in comparison with conventional imaging (Fig. 15.3a), making it possible to advance the needle to the suspicious lesion with greater precision.
Fig. 15.2ab
Fig. 15.3ab
Fig. 15.4
The combination of SonoCT® scanning with tissue harmonic imaging (see p. 13) has shown promising results. It allows detailed visualization of hepatic lesions (Fig. 15.5) or fetal morphology in prenatal ultrasound screening (Fig. 15.6). The high performance computer systems now available can easily combine SieClear® or SonoCT®