Erhalten Sie Zugang zu diesem und mehr als 300000 Büchern ab EUR 5,99 monatlich.
- Herausgeber: The History Press
- Kategorie: Geisteswissenschaft
- Sprache: Englisch
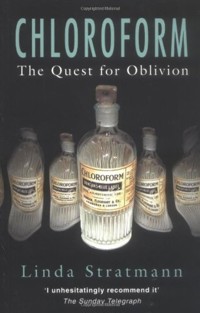
Chloroform, discovered in 1831 by three independent researchers - an American, a German and a Frenchman - has had multitude of roles. This engaging and entertaining book traces the social, medical and criminal history of the drug. Initially viewed with suspicion, chloroform gained immense popularity after it was administered to Queen Victoria during childbirth. Used in the Crimean, Punjab and American Civil wars, it saved thousands of soldiers from suffering extreme surgical ordeals. Chloroform was also used to treat asthma and cholera, as a rather dubious 'cure' for gonorrhoea and as a sweetener in medicines. However, the price of this anaesthesia was many sudden, inexplicable deaths under surgery, which caused years of passionate controversy. On an even more sinister note, chloroform featured in thefts, rapes and murder. W.T. Stead, editor of the Pall Mall Gazette, decided to expose the trade in young girls by 'buying a virgin' - chloroform was administered to her to prevent her fear when he entered her room. Chloroform was also used by America's first serial killer and in the mysterious death of a Texan millionaire. The fascinating story of an extraordinary substance, used and abused since its first discovery, Chloroform: The Quest for Oblivion includes previously unpublished research and will be essential reading for anyone intrigued by true crime or interested in social and medical history.
Sie lesen das E-Book in den Legimi-Apps auf:
Seitenzahl: 507
Veröffentlichungsjahr: 2005
Das E-Book (TTS) können Sie hören im Abo „Legimi Premium” in Legimi-Apps auf:
Ähnliche
To Gary
J’avais dit, au sujet de l’ether, que c’etait un agent merveilleux et terrible, je dirai du chloroforme, que c’est un agent plus merveilleux et plus terrible encore.
I have said, on the subject of ether, that it is a wonderful and terrible agent, I will say of chloroform that it is still more wonderful and more terrible.
Velpeau and Flourens, ‘Communications relatives au chloroforme’:see Chap. 14, n. 51.
Contents
Title Page
Dedication
Epigraph
Illustrations
Preface
Acknowledgements
1 Give Me to Drink Mandragora
2 Sweet Whiskey
3 Adam’s Rib
4 Under the Influence
5 Her Majesty is a Model Patient
6 The Cure for All Ills
7 Chloroform Goes to War
8 Murder, Mishap and Melancholy
9 Innocent Women
10 The Joy of Ether
11 The Crime of Adelaide Bartlett
12 The Sleep of Death
13 The Zealot of Hyderabad
14 Fade to Black
Appendix: The Chemistry of Chloroform
Glossary
Notes
Bibliography
Plate Section
Copyright
Illustrations
1 Replica of the original still used by Samuel Guthrie
2 The ‘Discovery Room’, 52 Queen Street, Edinburgh
3 Dr John Snow’s chloroform inhaler
4 Dr Clover and his apparatus
5 Simple chloroform masks from the catalogue of Cuxson Gerrard and Co., 1910
6 Entry in Dr John Snow’s diary, 7 April 1854
7 Dr Hardy’s patented chloroform douche, 1854
8 Dr John Mann Crombie’s patented apparatus for the self-administration of chloroform, 1873
9 The administration of chloroform in the American Civil War
10 Robbery under chloroform, as seen by Punch, 1851
11 The defendants in the Eliza Armstrong case
12 The anaesthetising machine of Raphäel Dubois, c. 1891
13 Frederic Hewitt’s modification of Junker’s inhaler, c. 1893
14 The Vernon Harcourt inhaler in use, with added oxygen, 1914
15 Professor J.P. Payne
Preface
When Professor James Simpson, on 10 November 1847, rose to address the gentlemen of the Edinburgh Medico-Chirurgical Society, he was about to realise one of his longest-held ambitions. Some twenty years previously as a young medical student, he had witnessed surgery for the first time. The operation, to remove a breast, was carried out by Robert Liston, one of the leading surgeons of the day. Speed was essential, as was the physical immobilisation of the patient, either by stout leather straps or the hands of burly attendants, since no reliable anaesthetic was then known. The sight and sounds of that operation were a horror that Simpson never forgot. He had fled the theatre in great distress, determined to abandon his cherished study of medicine, and enrol as a law student.
Fortunately he soon thought better of this decision and returned to his medical studies, but he made earnest enquiries of his professors to see if anything could be done to alleviate the terrible pain of surgery. The answer he received was that nothing could be relied upon to relieve the pain with any safety to the patient.
Simpson was not a man to be satisfied with that position, and later, as a qualified doctor, he experimented with a number of methods, including mesmerism. None of them, however, was the thing he sought. While other doctors accepted suffering as inevitable, it was clear that Simpson would not be content until he had found the perfect anaesthetic.
In 1846 news came from America of the development of anaesthesia using ether. Simpson took it up immediately and used it, controversially, in obstetrics, but soon felt that it had too many drawbacks. His use of ether had, however, given him both considerable experience with an inhaled anaesthetic, at a time when many medical men were opposed to its use, and also a standard by which to judge the effects of other volatile chemicals. The quest continued.
On that November day, Simpson prepared with some pride to reveal to the sober gentlemen of the Society his discovery of the anaesthetic powers of a previously little-regarded compound – chloroform. It was common for men of his profession to offer their research and observations for the assistance of their brethren and improvement of the human condition, hoping, also, to gain some personal prestige. All of these must have beckoned, though Simpson was successful enough for the last to be of little import. What he could not have expected was that the events of that November would be the defining moments of the rest of his life. Chloroform would bring him praise and honours, but it would also unleash upon him a storm of outrage. It brought him adulation such as few men ever experience, but when his career moved on to other causes he found that what he had hoped would be his greatest works were little regarded and that, even at the end of his life, all he was remembered for was chloroform. So closely was he associated with it that he was often credited with having discovered it, or administering it to Queen Victoria, neither of which was true.
What he was about to unleash was an agent whose innocuous appearance and pungent but not unpleasant fragrance concealed a dramatic power both to save and to take life. In the years that followed, there would be quarrels, controversy and confusion, with many expressions of pleasure and gratitude, and many deaths. Chloroform would revolutionise battlefield surgery, relieve distressing symptoms in numerous common complaints, and appear to effect astonishing cures – but it would also have a role to play in the crimes of robbery, rape and murder.
At the close of his address, Simpson recommended to the meeting that a committee should be appointed immediately to explore the qualities of chloroform. The gentlemen readily agreed, and the meeting was about to close, but Simpson had a final flourish to perform. He may have anticipated some scepticism, but he knew his audience, and he had come prepared. Never a man to lose the opportunity for drama, he produced a bottle of chloroform and a silk handkerchief, and invited the members to sample its effects. This attitude of almost careless confidence was always to characterise his future use of and total devotion to chloroform. Mr Young, a cutler, at once presented himself as a subject. A teaspoonful of chloroform was applied to the folded fabric, Mr Young inhaled deeply, and after only a few inspirations he was unconscious. A Dr Roberts was the next to try, with the same result. A Mr Hunter followed, and must have taken less than his predecessors, for he suddenly became excited, and jumped to his feet. This caused a certain bustle in the room, as he resisted the efforts of his fellow members to hold him. While this distraction was going on, the handkerchief was being passed around, and one by one the members applied it to their faces. All were surprised by the power of its effect. Gentlemen who might not have arrived at the meeting with the intention of becoming drunk soon found themselves in a state of intoxication. Others, having taken a more concentrated whiff, slumped unconscious in their seats. No doubt Simpson viewed the scene with amusement and satisfaction. Once recovered, the doctors were agreed that the sensation was delightful, and some were eager to repeat the experiment. Fortunately, no one was the worse for his experience. Had one of the audience died on that occasion, as might very well have happened, the future of chloroform would have been in some doubt, and history would have been a little bit different.
A NOTE ON MEDICAL STATUS
In nineteenth-century Britain only those medical men who were members of the Royal College of Physicians were entitled to call themselves ‘Doctor’. It is not always possible in contemporary material to identify the status of individuals, so for the sake of clarity, I have referred to all qualified medical practitioners as ‘Dr’ unless they had another title such as Professor, or a military rank.
Acknowledgements
I would like to extend my grateful thanks to the following individuals and organisations whose assistance in the preparation of this book has been beyond value: the Association of Anaesthetists of Great Britain and Ireland; Bellevue Hospital Archives, New York; the British Library; Cuxson Gerrard and Co. Ltd; Edinburgh City Archives; the Family Record Centre; the History of Anaesthesia Society; the Jefferson County Historical Society; the London Metropolitan Archives; the National Museum of Health and Medicine, Washington; the Newspaper Library, Colindale; the Nuffield Department of Anaesthesia, Oxford; the Royal College of Physicians, London; the Royal College of Physicians, Edinburgh; the Royal College of Surgeons, Edinburgh; the Simpson House, Edinburgh; the Society of Authors; the University of Edinburgh Archives.
A special mention is due to three people who have been extraordinarily generous with their time in steering me through the minefield that is the medical and chemical literature of chloroform – they are Dr Ray Defalque, Dr Harry Payne and Professor James Payne.
I owe a particular debt of thanks to Jaqueline Mitchell, for her unfailingly helpful and always excellent advice.
The encouragement and faith of one’s friends should never be underestimated. Gail, John, Liz – take a bow.
Finally, a big thank-you is due to my husband Gary, who, as well as giving practical help and support, has shown tremendous patience and fortitude in spending so many months living with a woman whose sole topic of conversation appeared to be chloroform.
CHAPTER 1
Give Me to Drink Mandragora
The escape from pain in surgical operations is a chimera, which it is idle to follow up today. ‘Knife’ and ‘pain’ in surgery are words which are always inseparable in the minds of patients, and this necessary association must be conceded.
Velpeau, a leading surgeon of his day, writing in 18391
In 1847 chloroform blazed on to the Victorian scene like a comet, whose muted beginnings were forgotten in scenes of brilliant light and grim shadow. Some regarded it with horror and despair, others predicted its rapid passing, but for many it was a triumph of science over nature, and the harbinger of a bold new age of medicine. To the confident and optimistic, chloroform appeared to be the ideal, the perfect anaesthetic that had been sought by humankind since the dawn of time. This heady excitement was soon to evaporate, but for many years to come, chloroform was widely used, abused and misused in human society.
To understand the reaction of the Victorian medical profession and public to the appearance of chloroform, we must first take a short tour of the history of anaesthesia, which is at least as long as recorded history itself. However, while there is ample information on the subject, it is hard to judge the effectiveness of early attempts at pain relief during surgery since the degree of success reported tends to depend on whether the writer is a surgeon, an academic, or a patient.
From earliest times, the possibility of anaesthesia has thoroughly engaged the minds of commentators on the human physical condition. Early Homo sapiens must surely have noticed that intense pain or a blow on the head would sometimes lead to unconsciousness, a state that mimics natural sleep but during which the patient (or, maybe, the victim) feels no pain. This observation would have stimulated the desire, and later the search, for some artificial means of procuring a pain-free slumber.
Possibly the first depiction of painless surgery in literature is in the Bible, when God causes Adam to fall into a deep sleep while He removes the rib from which He makes Eve. After the couple’s fall from grace, God issued a decree, the precise meaning of which is still a matter for lively debate. Henceforth, Adam must toil to bring forth food from the ground, while to Eve God said, ‘I will greatly multiply thy sorrow and thy conception; in sorrow thou shalt bring forth children.’2 The Bible therefore appears to associate painless surgery with the brief period of humankind’s innocence, and the travail of childbirth with the decline into sin, a distinction which was not lost on some nineteenth-century obstetricians.
EARLY PAIN RELIEF
The earliest attempts at pain relief probably used soporifics such as opium and alcohol, both of which have been available far longer than written records. Alcohol on its own was known to numb the senses, though its effects were short-lived, especially as pain could lead to rapid sobering of the patient. However, it was often used to carry doses of other drugs.
The unripe seed heads of the opium poppy yield a milky juice rich in alkaloids, of which the most important is morphine. The juice could be dried for storage and later mixed with water and alcohol. Its sedative and sleep-inducing properties made opium a valued aid to medicine, but it had two major drawbacks: it was poisonous; and it was addictive. It was not, of course, an anaesthetic, but for someone about to undergo surgery it was very much better than nothing. Despite the availability of soporifics, however, ‘nothing’ was what the patient often received. This meant that if a surgeon was to be able to operate effectively, the only thing to do was to tie or hold the patient down and work quickly.
Although the Greeks and Romans knew about opium, their writings make little mention of pain relief. It is not clear, therefore, whether the second-century Greek physician Galen, who advised opium and mandragora for the relief of pain before performing operations, was typical of his time or an enlightened exception. The Greek essayist and biographer Plutarch, describing a first-century operation on the Roman general Caius Marius for tumours in his legs, did not refer to any methods of alleviating pain – rather he praised the patient for his fortitude. Marius elected not to be tied down, but having endured the cutting of one leg without flinching or making a sound, he declined to allow the surgeon to touch the other, commenting, ‘I see the cure is not worth the pain’.3 Celsus, a Roman encyclopaedist writing about surgical practice in AD 30, advised that the ideal surgeon should be among other things ‘so far void of pity that while he wishes only to cure his patient yet is not moved by his cries to go too fast or cut less than is necessary’.4
Another plant with a long history of use for medicinal and social purposes is Cannabis indica, which grows naturally in Asia and India and produces a resin that has been used from early times to ease pain, induce sleep and soothe nervous disorders. In AD 220 the Chinese physician Hua T’o was said to have performed extremely complex surgical procedures without causing pain after administering a preparation of cannabis in alcohol. Unfortunately, his patients have left no record of their experiences.
Mandragora officinarum, a native of southern Europe whose root and bark have long been known to have soporific properties, is related to the deadly nightshade. It was described in Historia Naturalis, a 37-volume work written in about AD 77 by Pliny the Elder that included the medicinal use of herbs among its many subjects and retained its influence throughout the Middle Ages. According to Pliny, mandragora was ‘given for injuries inflicted by serpents and before incisions or punctures are made in the body, in order to insure insensibility to pain. Indeed for this last purpose, for some persons the odour is quite sufficient to induce sleep.’5 This may be the first recorded reference to pain relief during surgery being produced by inhalation.
The Greek pharmacologist Dioscorides, who lived in the first century AD, prepared the first systematic pharmacopoeia, De Materia Medica. It was translated and preserved by the Arabs, and finally translated back into Latin by the tenth century. This suggested that the root of the mandragora plant be steeped in wine and given ‘before operations with the knife or actual cautery that they may not be felt’.6 Mandragora had its dangers, however, which may have led to some caution in its use. Aetius, a Greek physician writing at the end of the fifth century, remarked on the effects of an overdose of mandragora, stating that a patient given too much would gasp for breath, became convulsed, and, if assistance was not given, die. This description has the ring of personal observation.
Mandragora continued to be used with caution for many hundreds of years. Bartholomeus Anglicus, who compiled an encyclopaedia of natural history in 1235, stated: ‘the rind thereof medled with wine … gene to them to drink that shall be cut in their body, for they shall slepe and not fele the sore knitting’.7 The thirteenth-century Spanish chemist, Arnold of Villanova, gave the following recipe:
To produce sleep so profound that the patient may be cut and will feel nothing as though he were dead, take of opium, mandragora bark and henbane root equal parts, pound them together and mix with water. When you want to sew or cut a man dip a rag in this and put it to his forehead and nostrils. He will soon sleep so deep that you may do what you will. To wake him up, dip the rag in strong vinegar.8
A contemporary surgeon, Hugo of Lucca, refined this method. He added the juice of lettuce, ivy, mulberry, sorrel and hemlock to the above and boiled it with a new sponge. This was dried and when wanted dipped in hot water and applied to the patient’s nostrils.
The properties of mandragora were still well known in the early seventeenth century. Shakespeare mentioned it in Antony and Cleopatra, when the Egyptian Queen demands:
Give me to drink mandragora! …
That I might sleep out this great gap of time
My Antony is away.9
Hyoscyamus niger, commonly known as henbane, is found throughout central and southern Europe, western Asia and India, and was well known by the first century AD for its action in pain relief and inducing sleep. The main constituents are the alkaloid hyoscyamine with small amounts of hyoscine and atropine. The plant was recommended by Dioscorides, though Pliny declared it to be ‘of the nature of wine and therefore offensive to the understanding’.10
It is also mentioned in medical works of the tenth and eleventh centuries, and by Elizabethan herbalists such as Nicholas Culpepper, an apothecary who in 1652 wrote his famous herbal The English Physician, and John Gerard, who in 1597 published his Historie of Plants, a compendium of the properties and folklore of plants.
Later it seems to have fallen into disuse, and is omitted from eighteenth-century pharmacopoeias. Gerard wrote that the juice caused ‘an unquiet sleep, like unto the sleep of drunkenness, which continueth long and is deadly to the patient’,11 and Culpepper advised that it should never be taken internally at all. In the Middle Ages the fumes obtained from heating the seeds were a popular treatment for toothache, though it was observed that there was considerable risk in its use, as its actions were uncertain and could lead to dangerous side-effects.
THE ABANDONMENT OF OLD KNOWLEDGE
The works of Galen, the Arab physician Avicenna, and the Greek ‘father of medicine’ Hippocrates were the basis of medical knowledge until the Middle Ages. Universities studied the old texts but added nothing to them. Since medieval philosophers held that the forms of nature were determined by God, it was not felt necessary to explain how things worked. Medicine was based on superstition, folk remedies, herbs, astrology and prayer.
While there were no real advances in pain relief up to the mid-nineteenth century, one might imagine that the old tried and tested herbal soporifics would continue to be employed in the absence of something better. The evidence of those who actually experienced or observed surgery tells a different and remarkable tale. Surgery after the Middle Ages was a terrifying and bloody agony, and the early methods of pain relief were largely abandoned.
Why did this happen? Some historians admit that they don’t know the answer. Others skate so carefully around the gap that one has to look carefully to find it. Still others say, in the face of considerable evidence to the contrary, that since the old soporifics were available they ‘must’ have been given. A few offer explanations, that there was a Renaissance backlash against the practices of the ancients, that opium, henbane and mandragora were not as effective as had been claimed and were dangerous in use, or that medical and religious tracts suggested that pain was in some way essential to the proceedings. All of these suggestions have some element of truth.
In the fifteenth century, improved translations of the classic texts created a renewed interest in Greek and Roman medicine, and this eventually spawned a counter-movement, whose most influential voice was the Swiss physician who called himself Paracelsus. He certainly believed in sweeping away the old beliefs, for in 1527 he publicly burned the revered works of Avicenna and Galen in front of the University of Basel. He believed in personal observation rather than books, and, importantly, he ushered in the study of the chemistry of the body and medicine. After his death his followers continued his work and, ignored by the universities, obtained private funding for their laboratories. Science and religion were still linked, and God was still the creator, but man could use science to explain the nature of the universe.
The movement gained ground, fuelled by advances in scientific method and inventions such as the microscope. The works of Galen and Hippocrates were no longer regarded with un-questioning veneration, and their remedies could be tested. While the old drugs were still used, it was no longer claimed that they produced anaesthesia, and it was realised that complete pain relief was only possible at great risk to the patient.
Nineteenth-century surgeons were extremely sceptical of the efficacy of such measures as Hugo of Lucca’s anaesthetic sponge. Dr John Snow, the leading London anaesthetist of his day, examined the prescription and announced his utter disbelief that such a sponge as prepared would, after being placed in hot water, give off any odour or vapour that would cause insensibility. He thought that if sleep were really caused by it, some of the moisture on the sponge might have reached the mouth or throat and been swallowed, his reason being that that the main ingredient was hemlock, which is not volatile enough for inhalation.
Snow also referred to a description written by Theodoric, the son and student of Hugo of Lucca, of patients about to undergo an operation being tied down or held by strong men. In operations for hernia Hugo directed that the patient be tied to a bench or table with three bands; one round the ankles, one round the thighs and one across the chest holding down the arms and hands. This hardly suggests a confidence in the anaesthetic.12
Henry J. Bigelow, professor of surgery at Harvard University, declared in 1876 that the essentials of a modern anaesthetic were that insensibility should be always attainable, complete, and safe. By contrast, he described stupefaction with poppy, henbane, mandragora and hemp, as partial, occasional and dangerous.13 Certainly, prior to the development of instruments for the sensitive measurement of drugs and the establishment of dosages, the amount of active principle in a herbal preparation must have varied enormously, with highly unpredictable results.
It is tempting to conclude with the nineteenth-century doctors that if their predecessors had had, as they claimed, a safe and successful method of preventing pain, it would not have fallen into disuse. The patient might well have felt that some pain relief was much better than none at all, but many doctors were chary of using strong soporifics, and while there were a few who were willing to make their patients drunk to the point of stupor before an operation, this practice was generally condemned.
A great deal of progress would be needed before anaesthesia could become possible, particularly in the development of the science of chemistry and the evolution of sensitive measuring apparatus. Meanwhile, just as doctors unable to prevent infection assumed that suppuration was normal and desirable, and welcomed the appearance of ‘laudable pus’, so they also declared that pain was a necessary and beneficial part of surgery, and deplored attempts to relieve it as not merely wrong, but dangerous. Medically, pain was a stimulant – it was good for you – while morally it was a punishment for sin, or a test of faith for the holy. If this was true of surgical pain, it was doubly true of the pain of childbirth, which was a perfectly natural thing with which it was unnecessary to interfere.
SURGERY AND PAIN
Descriptions and illustrations of surgery in the seventeenth to mid-nineteenth centuries are mainly a catalogue of unrelieved agonies. An account of an amputation by John Woodall of St Bartholomew’s Hospital, written in 1639,14 makes no mention of pain relief, but refers to the surgeon requiring five helpers, two of whom were to assist the surgeon with his instruments and needles, and the other three to restrain the patient. It was normal practice to locate the operating theatre of a hospital as far as possible from the main wards, often in a tower room, so the shrieks of the unfortunate patient could not be heard by those destined to suffer the same fate.
Despite Celsus’s recommendation that a surgeon be without pity, it is clear that many felt acute distress at the sufferings they were about to inflict. William Chesleden, one of the most distinguished surgeons of his day, was said to have suffered great mental anguish on operating days. His method of sparing the patient agony was speed, and he was able to complete a lithotomy (extraction of stones from the bladder) in less than one minute. In 1731 he recommended a draught of opium for the pain, but that was after the operation, not before. John Hennen, a deputy inspector of military hospitals, suggested in 1820 that ‘many of the primary operations would be rendered much more favourable in their results by the administration of a single glass of wine’,15 which does rather suggest that in some cases the patient was not even receiving that much.
A few doctors were eager to experiment with various means of reducing pain during surgery. Quite apart from humanitarian considerations, there was a great advantage to the surgeon. The cries and struggles of the unfortunate patient were distracting and distressing. The surgeon was obliged to hurry to complete his work and had little or no time to consult with colleagues when difficulties were encountered. Muscle spasms made treatment of fractures and dislocations especially difficult, and many delicate or lengthy operations, while technically possible, could not be performed on a conscious patient.
Some of the methods tried sound drastic and even dangerous. Many would only have been suitable for certain operations and robust patients. In the sixteenth century the effect of the tourniquet in dulling pain was well known, and was occasionally used in cases of amputation. An English surgeon, James Moore, suggested in 1784 that compression of the nerve trunks should be practised before cutting the area supplied by them, and John Hunter carried out this method for the amputation of a leg at St George’s hospital. A French surgeon, Richerand, declared that a dislocated hip was easily corrected after a bottle of port wine, though the main object of intoxication was muscular relaxation rather than pain relief. The seventeenth-century Italian physician, Marco Aurelio Severino, used a mixture of snow and ice to numb the skin before operations, applying it in narrow parallel lines for only fifteen minutes to avoid tissue death. Other methods used were compression of the carotid arteries to produce unconsciousness, and encasing the head in a helmet to which a sound blow was delivered with a wooden hammer! Philip Syng Physick of Philadelphia, referred to as ‘the father of American surgery’ decreased sensitivity to pain by bleeding patients to a state of collapse. In the 1790s he reported an operation in which after the bloodletting he was able to manipulate a dislocated joint. The patient, he stated, was entirely relaxed and seemed to feel no pain.16
One method that was extremely successful, with no risk at all to the patient, was hypnosis. This met with all the enthusiasm that one might have expected of the nineteenth-century medical establishment. The first accredited operation under hypnosis, a mastectomy, took place in France in 1829, but the authorities denounced the patient as a fraud and the doctor as a dupe. A Scottish surgeon, Dr James Esdaile, practised most of his working life in India, and there performed his first operations under hypnosis in 1845. Despite thousands of painless operations to his credit, on such conditions as piles, scrotal tumours, and compound fractures, with the mortality rate an amazingly low 5 per cent, the British medical profession refused to take his work seriously. John Snow was quite unable to believe in hypnosis. He thought that Esdaile and other surgeons had been ‘imposed upon by dishonest and designing patients, who afterwards confessed they had suffered the pain to which they had pretended to be insensible’.17 Alternatively, he suggested that the patients were susceptible persons in whom a condition resembling hysteria or catalepsy had been produced.
In the early nineteenth century, therefore, patients were still being tied or held to the operating table, fortified only by the power of prayer, though not a few might have had a stiff ‘bracer’ before the event. A patient undergoing lithotomy in 1811 at St Thomas’s Hospital in London described his experience:
My habit and constitution being good, it required little preparation of body, and my mind was made up. When all parties had arrived I retired to my room for a minute, bent my knee in silent adoration and submission and returning to the surgeons, conducted them to the apartment in which preparations had been made. The bandages etc., having been adjusted I was prepared to receive a shock of pain of extreme violence and so much had I over-rated it, that the first incision did not even make me wince although I had declared that it was not my intention to restrain such impulse, convinced that such effort to restrain could only lead to additional exhaustion. At subsequent moments, therefore I did cry out under the pain, but was allowed to have gone through the operation with great firmness … and when the words, ‘Now Sir, it is all over’ struck my ear, the ejaculation of ‘Thank God, Thank God!’ was uttered with a fervency and fullness of heart which can only be conceived. I am quite unable to describe my sensations at the moment. There was a feeling of release, not from the pain of the operation, for that was gone and lost sight of, but from my enemy and tormentor with a lightness and buoyancy of spirits, elating my imagination to the belief that I was restored to perfect health as if by a miracle.18
That more complex surgery was done without pain relief can be illustrated in the letter written by Professor George Wilson to James Young Simpson, blessing him for inventing chloroform anaesthesia. In 1843, Wilson had a Syme amputation of the foot, which involves a disarticulation of the foot with preservation of the heel pad. After the removal of the foot, the heel pad is swung forward as a flap, and attached to the stump. Once healed it will eventually bear weight. Wilson wrote:
Of the agony it occasions, I will say nothing. Suffering so great as I underwent cannot be expressed in words, and thus fortunately cannot be recalled. The particular pangs are now forgotten, but the black whirlwind of emotion, the horror of great darkness, and the sense of desertion by God and man, bordering close to despair, which swept through my mind and overwhelmed my heart, I can never forget however gladly I would do so.19
THE BEGINNINGS OF INHALATION ANAESTHESIA
Henry Hill Hickman, born in Shropshire in 1800, was probably the first person to attempt anaesthesia using an inhaled gas. A member of the Royal College of Surgeons from 1820, he conducted a number of well-documented experiments on small animals in 1824. When he placed a puppy under a glass dome filled simply with air, he saw that the animal gradually became unconscious, and he was then able to surgically remove one of its ears without it showing any signs of pain. The animal survived, and in later operations lost the other ear and its tail. Hickman went on to use carbon dioxide to produce unconsciousness in animals, and removed the leg of a dog, the ears of a rabbit and the ears and tail of a kitten. He published the results of these experiments in an open letter dated 1824 but it was given little attention. In 1826 the Lancet published a derisive letter headed ‘Surgical Humbug’ from someone signing himself ‘Antiquack’, in which Hickman’s letter was denounced as ‘a decoy by which the credulous may be induced to give up their senses as well as their cash’, and his procedures, which were effectively the production of asphyxia, were condemned as ‘occasioning sensations far more horrible than the pain inflicted by ordinary operations’.20 Hickman went to Paris in 1828 and asked for permission to perform his experiments there, but nothing came of this and he returned to England where, dispirited, he died in 1830.
Help, however, was at hand for suffering humanity. It had been at hand but unrecognised for centuries. It is not known for certain who first demonstrated the action of sulphuric acid on alcohol to produce what was known as ‘sweet oil of vitriol’. This may have occurred as early as the thirteenth century. The colourless volatile liquid, light enough to float smoothly on water, was highly inflammable and potentially explosive. The vapour had a distinctive penetrating odour, and a tendency to make people cough. In 1540, Valerius Cordus, a German botanist and apothecary, described its preparation, but it was Paracelsus who observed the hypnotic effect of the liquid after mixing it with the feed of chickens, recording that after a long sleep they awoke unharmed. More than 300 years were to pass before another scientist noted the effect. In 1730, the German chemist W.G. Frobenius renamed it ‘ether’. Its mode of preparation led to its later appearance in the literature as ‘sulphuric ether’.
The eighteenth century saw a renaissance of chemical and medical research. Doctors still had very little idea of what caused diseases, and most of their remedies were little more than palliatives, if they worked at all. However, as new compounds emerged from chemists’ laboratories and new elements were identified, the hope arose that among these modern marvels might be that elusive thing – a ‘cure’. The only way for doctors to find this cure was to try out any likely looking substance, on animals, on patients, and on themselves. In 1758, Dr Michael Morris explained the method of preparing ether to the Society of Physicians in London and related three cases in which he had ‘cured’ lumbago and rheumatism by rubbing it on the affected parts. The cold caused by the evaporation of the ether had created local anaesthesia.
In 1775, the English amateur chemist Joseph Priestley published a six-volume series called Experiments and Observations on Different Kinds of Air. Not only had he been one of the first to isolate oxygen, but he had also discovered nitrous oxide, a colourless gas with a slightly sweet aroma. Medical men were very excited about the new gases, and were eager to experiment by inhaling them, as well as the vapour of volatile liquids, to see if they had any therapeutic effect, especially for respiratory diseases.
In the 1790s English physicians Richard Pearson and Thomas Beddoes started using ether in the treatment of asthma, consumption, catarrhal fever (influenza), bladder stones, and scurvy. As a bronchodilator it may have relieved some respiratory symptoms. In 1798 Beddoes founded the Pneumatic Institution for Inhalation Gas Therapy in Bristol, then a thriving centre for patients coming to enjoy the mineral waters. His object was to combine a laboratory for the investigation of therapeutic gases with a small hospital. His advertisements offered permanent cures for consumption, paralysis, and venereal diseases, and while orthodox doctors denounced him as a quack, patients flocked for his free treatments. The gases they inhaled were mixed with air and included oxygen, carbon dioxide, nitrogen, and even carbon monoxide, which was thought to improve health as it gave the patient pink cheeks! Beddoes’s assistants were destined to outshine their master, for he employed Humphry (later Sir Humphry) Davy and the engineer James Watt to help manufacture the gases. As might be expected, the treatments offered no real benefit, and eventually even Beddoes ceased to believe in them. Patients did not return, even when offered money as an inducement, many of them feeling they were being experimented upon. When Davy left in 1801 the work dwindled to nothing and the Institution was closed in 1802. It was Davy who coined the term ‘laughing gas’ after inhaling nitrous oxide and discovering its pleasurably intoxicating effects. He noticed, however, that it also had the property of destroying physical pain and in 1800 observed ‘it may probably be used to advantage during surgical operations in which no great effusion of blood takes place’.21
It was more than forty years before anyone followed up this observation, and in the meantime ‘nitrous oxide capers’, where the public would pay to inhale the gas, became a feature of travelling carnivals. It created a dreamy, floating, drunken sensation, but also made the participants giddy so that they staggered about and became objects of amusement to onlookers.
In 1818 an article on the subject of ether appeared in the Quarterly Journal of Science and Arts.22 The author was Michael Faraday, then working as an assistant to Humphry Davy, and three years away from his more famous work on electromagnetism. He pointed out the resemblance between the effects of ether vapour and those of nitrous oxide gas but advised caution, since following an experiment with ether, a man had remained in a lethargic state for more than thirty hours and there had been fears for his life. This warning prevented serious investigation for a number of years. In the 1820s and 1830s, American physicians confirmed Faraday’s finding that ether and nitrous oxide were similar in effect, but this was seen more as a laboratory curiosity than something capable of practical application. The careful use of ether continued. In 1833 a Dr James Hurd was treating a patient with an abscess by inhalation of ether diluted in hot water. She became exhilarated, hummed tunes, and lapsed into unconsciousness for half an hour. He was so terrified he determined never to try it again.23 When ether and nitrous oxide were eventually recognised as anaesthetics this would emerge not from the laboratory, but from their recreational use.
Public interest in the sciences in the nineteenth century had led to the popularity of lectures by travelling ‘professors’ at which members of the audience would be invited to inhale the new intoxicants. Afterwards, medical students would retire to their lodgings and continue the experiments, not always with a scientific purpose in mind, and as the public heard about this so the practice spread. The custom of ‘ether frolics’ was duly added to the nitrous oxide capers. Since fluid ether was more easily transported than a bag of gas, it was now possible to have an ether party in your very own home. From time to time, a participant would be obliged to sleep off the effects, but several years were to pass before anyone thought this was an interesting development.
In 1839, William Clarke, a medical student of Rochester, New York, began entertaining his friends with ether inhalations. On an unknown date, possibly as early as January 1842, Clarke ad-ministered ether on a towel to a Miss Hobbie who then had a tooth painlessly extracted by her dentist, Elijah Pope. Clarke’s failure to publish an account of this groundbreaking event suggests that he didn’t fully appreciate its importance.24
In 1841, Dr Crawford Long of Jefferson, Georgia, introduced the practice of inhaling nitrous oxide to the young men of the town, and later changed to using ether. A mischievous soul, he used the excuse of mild intoxication to get away with kissing all the girls at parties. The fashion soon spread to other parts of the state, where reeling students could sometimes be seen inhaling ether in the street or on campus. Long had often discovered when recovering from the effects of ether that there were bruises on his body which he could not recall suffering, and wondered if operations could be performed painlessly under its influence. The first recorded use of ether as a surgical anaesthetic occurred on 30 March 1842, when Long used it in the removal of two tumours from the neck of James M. Venable, who felt no pain from the procedure and paid two dollars for his treatment. Long went on to perform other minor operations using ether anaesthesia, but although his methods were known in his immediate neighbourhood he refrained from publishing the results. His lack of any sense of urgency seems astounding, and his chief apologist was his wife, who pointed out that older doctors in the area were sceptical of the practice and Long felt he needed more time to perfect it, a difficult task in a small town where surgery was infrequent. He was also under the impression that the real answer to anaesthesia would come from current work on hypnosis. He finally published an account of his work in 1849 in the Southern Medical and Surgical Journal, but by then two major developments had taken place.
The first serious promoter of nitrous oxide anaesthesia was a dentist from Hartford, Connecticut, Horace Wells. Wells had inhaled nitrous oxide during a stage demonstration by a Dr Gardner Quincy Colton, who after receiving his degree had chosen a career of lectures and demonstrations. On 10 December 1844 he gave a gas demonstration at Hartford, which was attended by Wells. One of the audience, a young man named Sam Cooley, danced about the stage under the influence of the gas and ran against some wooden settees, injuring his knees without noticing the pain. Wells, who was shortly due to have a molar extracted, at once saw the relevance of this to dentistry. He persuaded Colton to bring a bag of gas to his surgery the next day. Colton brought it along in a rubber bag fitted with a tube and administered the gas to Wells, the tooth being extracted by his associate, Dr Riggs. Wells, who had felt only a little discomfort, was very optimistic. After some further experiments, he was confident of the value of this discovery. Convinced that he would make his name, he arranged a demonstration before a group of medical students in January 1845 at the Massachusetts General Hospital. It was a failure, for by mistake the gas bag was with-drawn too soon and the patient (who later claimed he had felt far less pain than usual) was only partly anaesthetised, and groaned loudly during the operation. An unruly audience cried ‘Humbug!’, Wells was humiliated, and he left Boston. His continued attempts to promote nitrous oxide failed. In 1847 the Paris Medical Society looked favourably on his work, but when he returned to the United States, it was to find ether established and chloroform the new rage. In January 1848, he spent a week repeatedly testing chloroform to the point of addiction and under its influence rushed out into the street and threw acid over the clothing of two women. He was committed to the Tombs Prison, his life in ruins. There, he committed suicide by inhaling chloroform to the point of analgesia, then slitting an artery in his leg with a razor. He was thirty-three.
In 1846, a one-time partner of Wells’s dentistry practice, William Thomas Green Morton, asked his former tutor Charles T. Jackson about the production of nitrous oxide gas. In the previous two years, Jackson had been experimenting with ether. He had realised that earlier difficulties were due to impurities, and had succeeded in purifying it so it could be inhaled without danger. He had intended to develop it for surgical purposes, but lacking the time to do the work himself, he responded to Morton’s enquiry about nitrous oxide by recommending ether as having a similar effect. Morton began to experiment with ether, and that year painlessly extracted a tooth from Eben H. Frost, who was asked to sign a statement to say that he had felt no pain. H.J. Bigelow was invited to observe a number of extractions and, as a result, a demonstration of ether anaesthesia took place at the Massachusetts General Hospital on 16 October 1846. Morton administered the ether, but the surgery, to remove a tumour from the neck of twenty-year-old Edward Gilbert Abbott, was carried out by a leading surgeon, Dr John Warren, the patient afterwards claiming not to have felt any pain. ‘Gentlemen,’ Dr Warren remarked to the enthralled audience, ‘this is no humbug.’25
In November 1846, Oliver Wendell Holmes, an eminent physician and father of the future Supreme Court Justice, wrote to Morton suggesting that the state produced by the agent be named anaesthesia, from the Greek an for ‘without’ and aesthesia for ‘sensibility’. The word was not previously unknown, but Holmes’s suggestion led to its common use.
Morton, certain that ether would make his fortune, refused to disclose the nature of the solution, added a few harmless impurities to try and disguise the smell, named it ‘Letheon’ (in Greek mythology, the waters of the River Lethe were held to expunge painful memories), and persuaded Jackson to join him in taking out a patent. They distributed circulars to doctors demanding half the fee in the case of any operation in which it was used. Dr Bigelow was not to be fooled. He soon discovered by its characteristic smell that Letheon was ether and sent the news to his friend Dr Boott of London. The day after receiving the news, Dr Boott tried the administration of ether in his own house at Gower Street while a neighbouring dentist, James Robinson, removed some teeth from a patient without causing any pain. This operation performed on 19 December 1846 was the first in which ether vapour was employed in England as an anaesthetic.
Morton’s attempts to capitalise on the process led to his being discredited. When Jackson tried to claim that he was the originator of the discovery, the partnership and the friendship came to an abrupt end. Morton spent the rest of his life neglecting his business and spending his money trying to obtain recognition, and ultimately became bankrupt. When he was forty-nine, in the July heat of New York in 1868, his mind finally gave way. Trying to drive out of the city in his buggy, he reached Central Park, then suddenly stopped, leaped out and collapsed, probably from a stroke. He died later in hospital.
Jackson spent many years attacking Morton’s claims to have originated the use of ether. Embittered, he turned to alcohol. Five years after Morton’s death he was found, raving drunkenly, at Morton’s graveside, where the stone commemorated his rival’s contribution to anaesthesia. He spent the remaining seven years of his life in an asylum, dying at the age of seventy-five.
With nitrous oxide temporarily disgraced, ether was the sensation of the day, although not everyone embraced the new concept of anaesthesia. The differences between the conscious and unconscious states were little understood, and the effect of anaesthetics on the brain was a mystery. Sleep was believed to be a halfway house between consciousness and death, during which the brain, apart from maintaining basic functions, was inactive. The higher functions of the brain, the essence of what made an individual human, were therefore locked in the state of consciousness, and to remove these was to reduce man to little more than an animal. The creation of artificial unconsciousness therefore raised the spectres of madness and idiocy. It was not only life, reason and intellect that were at risk, for the search was still in progress for the physical seat of the human soul, which might be in some part of the nervous system as yet not fully understood. Dr James Parke of Liverpool stated:
I contend that we violate the boundaries of a most noble profession when, in our capacity as medical men, we urge or seduce our fellow creatures for the sake of avoiding pain alone – pain unconnected with danger – to pass into a state of existence the secrets of which we know so little at present. … What right have we even as men, to say to our brother man ‘sacrifice thy manhood – let go thy hold upon that noble capacity of thought and reason with which thy God hath endowed thee …’26
Numerous contributions to the medical and general press show that, in the main, the detracting voices were few and surgeons welcomed the use of ether, although it did have its drawbacks. The smell was both unpleasant and persistent, and it irritated the airways, while large amounts were required for protracted surgery. It was slow to take effect, creating an initial state of violent excitement undesirable in delicate operations. In February 1847 it was reported that in a recent experiment, a man under the influence of ether had suddenly sprung up, jumped over three chairs and attacked an onlooker.27 It had taken six men to restrain him. Ether’s easy inflammablity was very worrying in the days of open fires, gas jets and candlelight. (Mr Young, the cutler who had been so keen to be Simpson’s guinea-pig, had once offered himself as a volunteer in a test where he was rendered unconscious with ether while a flame was held to his mouth. He survived.)28 What was needed was an anaesthetic that was simple to administer, requiring only small quantities, yet giving a rapid and complete effect, nonflammable for preference, and with a pleasant smell into the bargain. The answer was chloroform.
CHAPTER 2
Sweet Whiskey
I presume it was little suspected that such things were doing in a remote region on the shore of Lake Ontario.
Professor Benjamin Silliman1
In 1872 the eminent German chemist Justus von Liebig published a paper claiming the honour of being the original discoverer of chloroform.2 His only rival to that title, he believed, was the leading French pharmacist Eugène Soubeiran, who was in no position to argue the point, having died in 1858. The true discoverer of chloroform, however, was an industrious and eccentric amateur, the American Dr Samuel Guthrie. These three men produced chloroform independently and within a few months of each other, each by a different method. None of them knew what he had made.
Samuel Guthrie was born in Brimfield, Massachusetts, in 1782. His father, also Dr Samuel Guthrie, was a practising physician and surgeon of Scottish descent. Young Samuel studied medicine with his father and began his own practice in Smyrna County, New York. In 1804 he married sixteen-year-old Sibyl Sexton, and they started raising a family. In the war of 1812 Guthrie was an examining surgeon and took part in the second battle of Sackets Harbor. After the war he returned to medical practice but before long had set his sights on another career, starting what was to be a lifetime of manufacturing ventures, independent research and experiment.
In 1817 Guthrie was looking for a piece of land on which he could start a commercial enterprise, and recalled the pleasant location of Sackets Harbor on the shores of Lake Ontario. About a mile east of the harbour was a tract of land, almost a wilderness, but with considerable potential. It was good farming country, near a thriving port, and most importantly there was Mill Creek, a source of water power. Guthrie purchased the land, and with his wife and three children set off to make a new life. The area eventually became known as Jewettsville, after Abram Jewett, another 1817 arrival, who set up a brickyard. In the following years, industry flourished, and the village soon boasted sawmills, lime kilns, coopers’ shops, blacksmiths, a rope factory and three vinegar mills.
Guthrie was a resourceful man of great energy and ingenuity. He believed in wasting nothing. Soon he had cleared the land, built a home from local materials, piped water from a nearby stream, and planted his first crops, walling the area with the stones he had excavated from the soil. Until his commercial ventures matured he continued to practise as a doctor, and also articulated skeletons, which he sold to medical schools. Visitors and servants were sometimes horrified when opening containers in the house to discover them full of human bones. He was regarded with some awe by his neighbours and was considered a little peculiar by medical colleagues. A slender, stooping figure, with a prominent nose and expressive eyes, he had a thoughtful demeanour, and in common with so many great thinkers, dressed plainly and was a little careless of his appearance. He abhorred extravagance, but never grudged spending on scientific experiment.
By 1820 Guthrie’s tremendous industry had established him as a formidable presence in the neighbourhood. He had built a substantial brick house, which still stands today, barns and outbuildings for his farm, a distillery, vinegar factory, gunpowder mill, workshop and chemical laboratory. In his library were to be found works on medicine and chemistry, as well as scientific journals. The products of his businesses supplied Madison Barracks, a local military post, or were shipped to New York for sale. He also cultivated forty acres, planted a vineyard and raised cattle, sheep, poultry and hogs. This would seem to leave no time for recreation, but he enjoyed hunting and fishing, and the occasional game of whist, and sometimes entertained his family and friends on the violin. He was not, however, a man for idle conversation, and much of the time he was to be found in his laboratory or workshops, where he was occupied in a lifelong fascination with explosives.
Disappointed by the slowness of ordinary gunpowder he deter-mined to devise an improved priming powder. It was extraordinarily dangerous work. Every so often the villagers would hear a muffled explosion and see Dr Guthrie running out of his powder mill with eyebrows singed and face and arms scorched. He once claimed in a letter to have had about 100 explosions from the percussion powder alone, some of them very severe, the largest amount he had burned at one time being 30 pounds.3 On one occasion he had received the blast from a quarter of a pound of powder full in his face and eyes. In the middle of writing that letter he recorded that he had been obliged to break off and rush out of the house, because of a loud noise and a shrill scream of ‘Fire!’ from his alcohol distillery. The history of his accidents, he said, would fill a volume. The worst one was from putting his hand into a keg containing four pounds of percussion powder and cracking a piece of it between thumb and finger. The friction set fire to the powder and the resulting detonation resulted in terrible burns to his hand and arm, and tore most of the skin from his chest, neck and face. He was lucky not to lose his arm. His grandson described another such incident that lifted the roof off the workshop and flattened the walls; only the fact that the door opened outwards saved the occupants from injury. Altogether Guthrie was involved in eleven major explosions, and was often seriously burned, twice nearly fatally. Sometimes he was so badly burned that he did not want to be seen, even by his family, until some healing had taken place. While he recovered, a bed would be made up for him in the laboratory and meals would be passed to him through the slightly open door. Despite these incidents, which did permanent damage to his health, he did not give up this work until he was satisfied with the product, which was eight and a half times faster than common gunpowder. He also compounded the powder into small pellets, which achieved a wide sale.
Such was the success of his business ventures that Guthrie, even though there were now four children to provide for, was able to abandon the medical profession and spend more time on his experiments. In 1830 his sons, Alfred and Edwin, were old enough to take over many of the business activities, and in the next two years, before they left to pursue their own careers, Guthrie devoted a great deal of his time to his laboratory. The results of his work were published in the American Journal of Science, whose founder and editor, the noted pioneering chemist and geologist Professor Benjamin Silliman of Yale College, would receive boxes packed with small bottles of the compounds produced by Guthrie. One such project, which Guthrie undertook in 1830, was an attempt to produce sugar from potatoes. He didn’t succeed, but did make what he called ‘potato molasses’, which was glucose syrup.
Early in 1831, Guthrie read an entry in Silliman’s Elements of Chemistry4 that greatly interested him. Silliman described how in 1796 an association of four Dutch chemists who had already discovered the gas ethylene (C2H4), which they called ‘olefiant gas’, studied the effects of mingling it with chlorine. Chlorine (Cl2) had been discovered in 1774 by the Swedish chemist Carl Wilhelm Scheele, but it was not until 1809 that it was recognised as an element. Its compounds were widely used for bleaching and fumigation.
The result of the Dutch chemists’ experiment was a dense oily-looking liquid with an interesting ethereal odour and a sweet taste, which they called ‘chloric ether’, though it was popularly known as ‘Dutch liquid’. They had not been able to discover its composition, and for many years it was a little-regarded curiosity. Silliman had been in the habit of preparing an alcoholic solution of the liquid in his laboratory at Yale, sipping it diluted with water and calling the attention of the medical students to its ‘remarkably grateful properties as a cordial’,5 suggesting that it might prove to be invaluable in medicine. By 1831 it was known to be a compound of carbon, hydrogen and chlorine (C2H4Cl2), and though its medical potential had not been explored, Silliman declared it was highly probable it that would be an ‘active diffusive stimulant’.6 This liquid we now know as ethylene dichloride. It is inflammable and highly irritant when inhaled. It is mainly used in the manufacture of PVC and as a pesticide, and is not considered suitable for human consumption.
The Dutch chemists’ method of producing their liquid resulted in only a small yield of the promising product from a large volume of gas. Guthrie scented commercial potential, and at once started experimenting to see if he could produce the liquid in a simpler and cheaper way. He decided to start by combining, at great expense and after some soul-searching, two gallons of best whisky and three pounds of chlorinated lime (which he had been using as a disinfectant in the henhouse). Presumably he expected the lime to give up its chlorine, which would then combine with carbon and hydrogen from the alcohol (C2H5