5,39 €
Mehr erfahren.
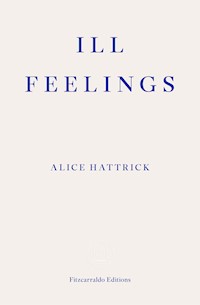
- Herausgeber: Fitzcarraldo Editions
- Kategorie: Sachliteratur, Reportagen, Biografien
- Sprache: Englisch
In 1995 Alice's mother collapsed with pneumonia. She never fully recovered and was eventually diagnosed with ME, or Chronic Fatigue Syndrome. Then Alice got ill. Their symptoms mirrored their mother's and appeared to have no physical cause; they received the same diagnosis a few years later. Ill Feelings blends memoir, medical history, biography and literary non-fiction to uncover both of their case histories, and branches out into the records of ill health that women have written about in diaries and letters. Their cast of characters includes Virginia Woolf and Alice James, the poets Elizabeth Barrett Browning and Emily Dickinson, John Ruskin's lost love Rose la Touche, the artist Louise Bourgeois and the nurse Florence Nightingale. Suffused with a generative, transcendent rage, Alice Hattrick's genre-bending debut is a moving and defiant exploration of life with a medically unexplained illness.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Veröffentlichungsjahr: 2021
Ähnliche
‘Ill Feelings is a deeply personal and deeply political reckoning with the nature of illness, inheritance, time, silence, bodies and invisibility. Alice Hattrick offers both a radical redefinition of the dominant narratives surrounding health and pain, and the knowledge we need in order to name, understand and resist them. Hattrick has found a voice and form which open up new and exciting possibilities for writing the self and making sense of the collective past: I read this remarkable book with outrage, fascination and immense admiration.’
— Francesca Wade, author of Square Haunting
‘I love the quality of attentiveness that Alice Hattrick brings to their poised and pointillistic exploration of the mysterious aetiologies and affects of chronic fatigue. They excel in listening out for echoes and whispers, their narrative of illness wriggling into uncomfortable places that medicine dismisses or ignores. Their book makes you pause to think – and rethink – page by page.’
— Marina Benjamin, author of Insomnia
‘Ill Feelings defies neat conclusions as well as easy categorization of the book itself, so that attempting to describe it here seems like misdiagnosis, and to try and name the paradox at its heart seems like a betrayal of its rewards. But the thrill of Alice Hattrick’s writing stems from its struggle to be free of its constraints, communicating with unspooling fury the mutability of lived experience rather than presuming to define it. In doing so, they remind us that the undefined – our own ill feelings – reveals not weakness so much as our inherent capacity for resistance.’
— Olivia Sudjic, author of Exposure
4‘I read Ill Feelings with a sense of wonder at the courage required not just to live with a medically unexplained illness, but to write about it with such descriptive clarity and probing intelligence. Alice Hattrick’s book is a powerful cure for ignorance or indifference about a complex form of suffering.’
— Edmund Gordon, author of The Invention of Angela Carter
‘Ill Feelings is a necessary, urgent book that I feel I have been waiting my whole life to read. A beautiful combination of memoir, reportage and razor-sharp analysis, it made me think very deeply and critically and feel powerfully understood all at once – a testament to what truly accomplished non-fiction writers can achieve. This book makes me excited for the future of literary non-fiction writing and it’s power to change the world and how we see it.’
— Lucia Osborne-Crowley, author of My Body Keeps Your Secret
‘“Poetry is not the same to the ill, the clouds look different, and so too does the rest of nature.” Alice Hattrick brilliantly geographies sick time and ill feelings. They chronicle not just how pain is located in the body but how it stretches outside of itself, across time and generations, through society and literature. The weight or unweight that is given to it; how disabled voices are heard (or not heard); the toxic way society views unrecovery. This book, and others like it, are always needed, but this feels especially needed right now, when 60 per cent of those who have died of Covid-19 in England have been disabled, and online disability hate crime has risen 46 per cent.’
— Jen Campbell, author of The Beginning of the World in the Middle of the Night
7
ILL FEELINGS
ALICE HATTRICK
9
‘How well one has to be — to be ill!’
— Alice James’s Diary
Contents
Ill Feelings
¶ Dredge
The day after her fifty-fourth birthday, my mother and I walk through a field near her house at dusk, a small pair of scissors tied to a long string around her neck. The dogs are on their leads because it’s getting dark and she isn’t brave enough to let them off ‘because of the rabbits’. She has already been signed off sick for a year and three months. As we walk, my mother starts to sing the folk song, ‘She moved through the fair’.
My love said to me
My mother won’t mind
And my father won’t slight you
For your lack of kind
My mother mostly sings songs she learnt at musical theatre college, or Norwegian songs from choir, but this one is different – it belongs to her. The lyrics, and the tune, make her voice melancholic, and more relaxed.
And she smiled as she passed me
With her goods and her gear
And that was the last
That I saw of my dear.
We walk quite far that evening, further than I expect. My mother wants to walk further still, but she is worried about walking back, about me walking back. She is used to negotiating the length of these walks in her own mind, depending on how she is feeling in her body, and the things she still needs to do that day, or even the next day, like go and see her father at the care home, or finish filling out another form relating to her ‘Ill Health Retirement’. It 12is a careful calculation that, once decided upon, can and most probably will be ruefully ignored – she just has to face ‘the consequences’.
My mother has moved to mid-Norfolk, where the River Nar crosses the Peddars Way, to be near my grandfather, who has vascular dementia and Alzheimer’s. He is convinced she lives in Burnham Market, a posh town near the North Norfolk coast, where no one in our family has ever lived, and none of us could ever afford. My mother will move away from here just as quickly, once he has died of leukaemia. The village she has moved to is an ancient land of crossings. When she first arrived, a woman told her she would be healed by the power of the place itself.
My mother had to reschedule her last meeting with HR because it was at 9 am on a Wednesday.
‘I was in bed all morning,’ she says, as if they should know that someone who is about to be signed off sick forever will never make it to a meeting first thing. It’s like the time she was annoyed at the ME/CFS service, who kept calling her when she was asleep, without warning.
What she means is: I am in bed all morning every day.
‘Dear Dr,’ reads a document on her desktop back at her house, ‘I have muscle weakness in my hands (holding a pen, lifting a kettle) and legs and breathlessness and palpitations on activity are problematic. Processing and translating information is very difficult and slow, which makes research, publication and teaching impossible.’
‘I’ve had enough of my shit,’ she says to me, on our walk. ‘I’m wasted.’
When my mother says she’s wasted, does she mean she feels wasted – ill, fatigued, sick – or does she also mean her working life is wasted, her potential is spent?
A long time ago, my mother sought a diagnosis. Upon 13relapsing into full-blown illness again, unable to go to her job as a lecturer in History of Design, she has found only more work: phone calls and confusing meetings with HR, days spent compiling documents with names like ‘Letter to Sussex Wide ME service.doc’ and ‘Ill Health Retirement Factsheet.pdf’. My mother must write her own medical history, over and over again, like a doctor, except she is also the patient.
‘ME also causes severe impairment of my cognitive functioning including extreme difficulty in focusing and concentrating for any length of time on a task, conversation or text,’ she writes. She suffers with ‘impaired and interrupted sleep and extreme irritability and mood swings’, wakes extremely fatigued, has ear pain, breathing difficulties, frontal headache, sore throat, nausea, heart palpitations, unrefreshing sleep, and even ‘orthostatic intolerance, anxiety and of course extreme fatigue’. She cannot ‘function’, has trouble ‘processing and translating information’, including ‘knowledge of her subject’ and ‘events in the past’. She must describe her ill feelings – not being able to stand for very long, feeling sick, feeling tired and sore – as if her body is not a body at all, as if her body is a machine malfunctioning, like she is faulty, or broken. If she were a computer she would have crashed.
If ‘illness is the great confessional’, as Virginia Woolf wrote in her essay ‘On Being Ill’, why is my mother writing like this? Where are the ‘things said, truths blurted out, which the cautious respectability of health conceals’? There is the impossibility of speaking through pain, which Woolf also wrote about – ‘let a sufferer describe a pain in his head to a doctor and language at once runs dry’ – but that is not exactly true. It is as if my mother is writing against the possibilities of a literature of illness entirely. 14
My mother does not speak to me in the way she writes in her ‘Details of Illness’. She speaks like Woolf in June 1919, writing a letter to her sister Vanessa: ‘Did anyone ever suffer as I did? You might have seen my soul shrivelling like a – I cannot remember the image exactly, but it is something one does by rubbing a piece of sealing wax and then everything else curls up – as if in agony.’
When I am touched, I feel like those fish that twist up in the heat of your hand.
‘Fuck all this fucking paperwork,’ she says. ‘I’m wasted.’
Audre Lorde wrote The Cancer Journals so that, in her words, ‘the pain not be wasted’.
Is feeling wasted the same as feeling worthless? I do not need to ask her. I’m not her therapist. I am her daughter, her biographer, and I know how she feels. I have always been like her, and, for most of my life, she has felt ill.
With the onset of illness, there is a ‘before and after’ instead of a beginning, a middle, and an end. There is before you got sick, and then there is after – your life forever changed. My mother has a small black-and-white photograph of herself, taken when she started her BA, a copy of which would have been pinned to the notice board during her undergraduate course at the university where she would eventually teach students about archives, material culture and queer histories: her ‘before’. On the back, she has written: ‘Taken in 1994. I am 29. Pre-ME – JUST’. She has short hair and is wearing a white wide-collared shirt and a dark coloured waistcoat. She is young: thirty-one, not twenty-nine, unless she got the year wrong. Either way, she is younger than me, except she has two young children, a girl and a boy. She is on her own, when it comes to childrearing and homemaking at least. She isn’t ill, yet. 15
The following year, my mother collapsed with mycoplasma pneumonia, which causes flu-like symptoms, such as fatigue, headache, chest pain and fever. I don’t remember how long she had pneumonia for – it wasn’t even the kind of illness that requires hospitalisation, which is why it’s commonly called ‘walking pneumonia’ – but she never fully recovered and was eventually diagnosed with ME/CFS two years later. Five years spent in her bedroom in the dark followed; ten years of carers in and out most days.
I remember her still lying in the dark of her bedroom in our ground-floor flat in Brighton when I got home from school, if I myself had been well enough to go. She got chest infections all the time, which she would read as a sign of something else more deeply wrong with her, but then she would not get at all sick, and explain that this was because of her ‘overactive immune system’. At night, she slept lightly, if she slept at all. Her legs and arms felt heavy all the time, like they were weighted down at her hands and feet. She would often shudder as if electrified, at even the smallest noises or movements, sometimes nothing at all. She struggled to remember things – mainly nouns. She would get this awful ringing in her ears. She had digestive problems, pains in her chest and difficulty breathing. Sometimes her throat would close up, and she’d cough and cough, as if there was something poisonous in the air.
Since that time, some years have been better than others, just like some days are better than others. My mother’s initial bouts of pain relieved, and her fatigue got worse. She got well enough to finish her degree, eventually, and then her MA and a PhD, to teach part time, but hers is not the kind of illness you ever really recover from. ‘Fatigue’ is not the main problem anymore, not that I can 16ascertain what the main problem is, or where it is: her heart; her head; her sleep; her whole body. She still has muscular pain and light sensitivity, a lot of weakness, the feeling that her muscles ‘don’t have power’. More recently, she has taken to calling it the vapours.
The day my mother collapsed in 1995, I found her on the kitchen floor. ‘Alice witnessed this,’ she later wrote, as if I had observed a crime and needed a new identity. I had told my brother to stay in the living room and went to our neighbour for help. According to my mother, it was then that I become ‘insecure about leaving the house’, and ‘became angrier and her schoolwork suffered’. Was this enough of a reason to contact the already-over-subscribed mental health service? Did I just not want to leave our flat knowing that if I wasn’t there, no one would be there if she collapsed again? I also developed symptoms of illness. My mother reported to doctors that I felt ill on waking, with sore throats, tummy aches and headaches that seemed to last all day; that I said I needed to rest and wanted to sleep during breaktimes at school; that I had pain in my arms and legs after sport, dancing and ‘just the normal walking and standing of the day’; that these symptoms felt heightened when I lay down to sleep; that I had mood swings and emotional symptoms; that I was ‘full of anger’ which was often directed at her because she was ill; that I got upset because I felt ill so much of the time and could not cope with what was expected of me. I was eventually diagnosed with chronic fatigue syndrome by the doctor at the local children’s hospital, where I was being monitored for my size and weight. I remember feeling almost pleased with my diagnosis, even if I was not entirely convinced by it. It made me feel closer to my mother.
‘It was awful when you first got ill,’ my mother said to me, during that same trip to Norfolk. ‘They told me we 17had a shared hysterical language.’
Hysteria – wasn’t that a nineteenth century diagnosis? Did a doctor really tell her that our symptoms, our pain and fatigue, were, in fact, not symptoms of an illness at all, but a – gendered – language that only we could speak and no one else could understand?
‘They made me feel so guilty about you,’ my mother recalled, ‘and at the same time I had to prove my own illness was real. It was an awful time. They told me I was making you ill.’
My mother and I have symptoms of illness without any known cause – according them the status of feelings, confined to our bodies, or our sense of them as ill. Ill – bad, sick, wrong – is also how I learned to feel about my diagnosis. Those ill feelings were not really my own, but reflections of societal ones, which deemed people with ME/CFS as fakers, scroungers, lazy and privileged, and indeed all chronically ill and disabled people as less-than-human, deserving of fewer rights, less pay, and less security and care.
Ill feelings were always something we shared. I never went to support groups or had a friend with the same diagnosis. If I did talk about it to someone else, it didn’t feel real, or mine. It is that kind of illness: somehow ubiquitous, or at least recognizable, continually reported on, and always inexplicable. The NHS website describes the main symptom of ME/CFS as ‘feeling extremely tired and generally unwell’. It made it all sound so vague – the feeling of being ill, without a reason – no biomarker or treatment or explanation. It is often referred to now as an ‘invisible illness’, but I don’t remember that term when I was growing up.
If illness was our problem, separation appeared to be the only solution. At the suggestion of my grandmother, 18I even went to a boarding school – my place funded by charity – in the Sussex countryside. I had just turned eleven. Away from my mother, I was unable to pick up symptoms off her. I recovered, for a time, but I am not well now, and we are further apart than we have ever been. My grandmother was right about one thing: my mother’s illness and my own ill feelings were inexplicably intertwined.
The day after my grandfather collapsed with what would be diagnosed as leukaemia, many years after my mother’s first illness, she told me her ‘old ME symptoms’ had come back. Her mother had already died, and she had taken on the role of her father’s primary carer.
‘When I lie down in bed my heart feels heavy,’ she said to me, ‘as if it’s been straining to pump blood to my legs all day.’
She had felt the loss of her mother in her body as illness, and now, over the time caring for her father, it was as if that loss in her body had tired her heart. She still had no language for her feelings, besides the terms she has managed to steal from medicine – a form of subterfuge.
‘What is fatigue anyway,’ she continued, ‘your heart not pumping hard enough?’
My grandfather had begun lining up all the tools he could find in his house, from screwdrivers to biros, in rows on the kitchen table. Losing his own grasp on reality and time, he tried to make order out of chaos, a vast chasm or void. With my mother, this disorder was happening in her body: it felt like there was something wrong with her chest or her heart or her legs. These were disturbing sensations that couldn’t be measured, tested or diagnosed, let alone treated.
It had taken the doctors at the hospital a few days to 19diagnose my grandfather with leukaemia as well as dementia. Apparently, he hadn’t had a blood test for a long time. The consultant said to my mother that he’d had cancer for months, but he says it like ‘for months’ to make her feel bad for not caring for him properly, as if his health was her responsibility, as if she could diagnose disease with the power of a daughter’s duty itself. ‘He was wearing an Yves Saint Laurent belt,’ she told me on the phone, which seemed to prove something, to her at least. We could not speak for too long because using her mobile made her ear hot, to the extent that she thought her brain was being ‘zapped’.
‘Once you’re diagnosed with one thing doctors attribute every problem you have to that one disease,’ she said. ‘And we know all about that, don’t we?’ When she speaks to me, she speaks to herself, or to the both of us at once.
In 1868, Alice James’s mother called her daughter’s teenage affliction ‘a case of genuine hysteria for which no cause as yet can be discovered’. Alice’s ‘nervous turns’ were ‘not in the least degree morbid in character’; she never seemed to dread an attack and seemed ‘perfectly happy when they are over’ – the tell-tale sign of nervousness, rather than an underlying physical ailment. The lack of reason for Alice’s symptoms was frustrating for both mother and daughter: ‘It is a most distressing form of illness, and the most difficult to reach, because so little is known about it.’ Alice spent the majority of her adult life in bed or on a sofa, propped up by cushions, known as the invalid sister to her two famous – and prolific – brothers, who often suffered with their own ailments, to the extent that as a family they shared the same body: ‘my nerves are his nerves’, she wrote of Henry, a devoted brother, ‘and my stomach his stomach’.
After Alice’s mother contracted bronchial asthma 20and died in 1882, everyone had expected Alice to get ill. Daughters were known to be affected by the deaths of their parents because of their lives spent at home. Instead, her Aunt Kate reported her ‘taking up of household duties that her mother laid down’, which ‘brought new life to Alice’. Alice and her father moved from Boston into a ‘little’ three-storey cottage at Manchester-by-the-sea that summer, built in an English country style. Henry Snr got up between 5 and 6 am every morning and wrote until 1 pm, while Alice managed the house, the meals, the workmen and the visitors – ‘just as her mother had done’.
‘I feel like I’ve lost my partner,’ my mother said, after the death of her father, having returned to care for him. She sounded like Alice, who became her father’s replacement wife: ‘I used to think I loved my dear Mother & knew her burdens,’ she wrote, ‘but I find I only knew half them, & that in losing her I am only nearer to her than I ever was before; it is such a happy thought that her dear, tired body is at rest… Instead of having lost her it seems sometimes as if I had never known or loved her before.’ A singular loss is always experienced as more than itself: it is felt as total.
For Alice, becoming a wife, carer and nurse to her father was preferable to another stay at the nursing home for nervous women. It was a way to hold herself together, to stop herself breaking down, or, in her words, ‘going under’. Like Alice, we were told we were hysterical, that we were inventing a language of our own demise, that for some reason we needed to be ill to get the attention we desired. My illness could be explained by my mother’s. It was as if our personalities were sick.
In July 1890, writing in her diary, Alice recorded that she took a very small amount of morphine, the first in three years, during her last and ‘rather excessive and 21comic’ prostration. Taking such a slight dose of opiates, Alice was consequently able to steady her nerves and experience the pain (toothache, rheumatic gout and a very bad crick in her neck) ‘without distraction’, for there is, she thought, ‘something very exhilarating in shivering whacks of crude pain which seem to lift you out of the present and its sophistications (great Men unable to have a tooth out without gas!) and ally you to long gone generations’. The unmedicated generations Alice writes of suffered toothache ‘such as we can’t dream of’, but also gendered illnesses lost, not recorded, unheard. When my mother and I enter the doctor’s surgery, our symptoms are still opaque and illegible, real and unreal. they are still ours alone to record, and, often, self-medicate.
To relapse is to return, to fall back, or fall off; to fall from grace.
When I started to explore my childhood diagnosis, I cycled everywhere, I went to work, I stayed out for late dinners with friends without needing to rest for days before and after. I still had days in bed and knew I couldn’t do as much as other people, like work as many days, or do much in the evenings. I knew I got muddled and confused often. I spent most weekends in bed. I got angry and I didn’t know why. I knew if I kept trying to keep up with everyone else, I would crash. But I also knew these things were not the same as being ill. Ill was not how I identified. But then: I had never known what ‘well’ felt like either. As a child I was often very tired, always had a headache and complained of my legs hurting.
When I told my mother, I was resigning from my full-time job because I could not manage the hours, and that my relationship had broken down (again), she was strangely surprised. She had thought I was well enough 22to work, to have a long-term relationship and a social life. I had somehow kept my ill feelings from her too. In fact, they were largely invisible even to myself. It was as if illness was lying dormant in me as a sense of unease, or mistrust in my own feelings.
As time passed – sick time, the time of relapse and re-diagnosis, naming and categorization, treatment and advice – I grew increasingly aware of how many women, and their mothers, I already knew with some form of unexplained illness. These people confided in me, as a fellow sufferer. A friend emailed to tell me she had been diagnosed with ‘burn out’ after months of suspected ME/CFS. A collaborator told me her sister, who was in her twenties, was still being cared for by her mother at home. A school friend did not realize her mother’s fibromyalgia had no known root physical cause, and another’s was coming off strong opiates for hers. Someone else told me her mother had once forgotten everyone’s names and was still living without a diagnosis for what appeared to be neurological problems with no neurological cause. My own partner’s mother revealed it was many years into her marriage before she realised not everyone had pain all the time. They had been there all along, but I had never really seen them. It was as if we had become invisible to each other.
And then I got ill: less and less able to get out of bed before the morning became the afternoon, less mobile, less able to walk very far or stand without support, concentrate long enough to read a book, or go to work for a whole day, or sit at my desk. Less able to control my mood, my anger.
And I got sick. I got sick of reading about how mothers ‘spread’ their borderline personality disorder to their children, stories of ‘fatal mothering’, and teenagers being 23detained in psychiatric units because of their diagnosis. I got sick of reading theories that chronic fatigue had something to do with mitochondria, or mice leukaemia, or nematode worms, or that they had nothing at all to do with any of these things after all. I got sick of hearing how half of all people with a diagnosis of ME/CFS also have Lyme disease, and that the bacterium Borrelia burgdorferi, which causes symptoms such as tiredness, pain, memory loss and confusion, is also found in seventy per cent of people who have died of Alzheimer’s. I got sick of reading about how the ill feelings and strange sensations I had always felt to be real are actually a cry for maternal affection projected onto a female lover: Vita Sackville West, who was ‘tender and affectionate to Virginia Woolf in her illness, and making herself more valuable by the threat of absence’. I got sick of reading about some kind of as-yet-unknown ‘familial susceptibility’ in cases of ME/CFS, about the sort of influence that does not allow space for care and love. I got sick of all this fucking paperwork. I got sick of hearing about the relation between mental illness and maternal neglect or absence, which of course sometimes involves the total loss of a mother. I write through this sickness, or sicknesses, knowing all these things are true, and not true, because they are not known, they are felt.
I began writing before the existence of the novel coronavirus. With a global pandemic, and hundreds of thousands of deaths, comes something even stranger, more nebulous: life, post-viral, which does not mean sickness when it has gone away, when the original disease has been cured, and the patient recovered. Within weeks, ME/CFS advocacy groups warned of the coming uptick in cases amongst patients that had recovered from an initial Covid-19 infection. Doctors already studying the 24biology of ME/CFS started research into coronavirus patients as they recovered. There were reports of people – some of whom had never been tested for coronavirus, because there were so few tests available to begin with – whose symptoms still cycled after months. They found that their family and friends, and even doctors, could not understand why they were still fatigued, suggesting that perhaps it was anxiety, or depression, or deconditioning – terms borrowed from the ME/CFS playbook. When they tried to exercise, they found that it set them back in their recovery, if that was even the right name for it. In 2009, six years after the SARS virus infected around 8,000 people, forty per cent of patients who recovered reported a chronic fatigue problem, and twenty-seven per cent met the modified 1994 Centers for Disease Control and Prevention criteria for chronic fatigue syndrome. What if they never recovered fully?
ME/CFS and FM had not historically been studied enough. Funding had been syphoned off to other diseases in the US, and patients felt abandoned. In the UK, a group of influential psychologists, many of whom had ties to private CBT providers and insurance companies, had misreported that graded exercise and ‘cognitive behavioural therapy for erroneous illness beliefs’ were effective treatments for ME/CFS in the results of a trial costing the taxpayer £5 million. The NICE guidelines still advised these treatments because they hadn’t been reviewed for thirteen years. People with ME/CFS were hopeful that studying coronavirus would shed light on the biological processes underlying their own condition, and devastated by the lack of support after years spent in their beds, at home, with no treatments or financial support, told they could not work or study from home, told it was all in their heads, that they needed to be ill, that they 25had a shared hysterical language.
‘We’ll go as far as the river,’ my mother says, having quietly completed her calculation. ‘I have to see my river every day.’
Standing at the water, watching one of the dogs walk very carefully across the small rocks on the riverbed, I think about what she said to me the day before, when we were sitting in her garden: that no matter how far she walks each day, she never feels any stronger.
Later, I will read that some researchers have found markedly reduced cardiac mass and total blood volumes, causing orthostatic intolerance and cardiac arrhythmias, including tachycardia (racing heart) or palpitations, in patients with ME/CFS. One study in Japan suggested people with a diagnosis of ME/CFS had smaller hearts, and another suggested that ‘non-compliant veins’ – veins that were not moving enough blood around the body – were the problem and could explain ‘post-exertional malaise’. Maybe my mother was right, and her heart really wasn’t pumping hard enough after all.
I want to tell her, to confess, that I have been reading the documents on her desktop and in the paper folders on her dining table, which she has been writing and gathering for her application for Ill Health Retirement. I want to tell her I have been asking her about how she is feeling, and what it was like when I was much younger, when I was also ill and she was even more ill, and nobody seemed to believe us, because I want to know how she is feeling, but also because I want to tell our story. Except I don’t.
Dredging a river imposes a brake on the ability of the river to heal itself. When a low-energy river is dredged, it cannot recreate its meanders, pools and riffles; sediment is deposited across the full width of the channel creating 26excessive and unfocused plant-growth. It happened with the Nar, which is a chalk, and therefore relatively rare, river system. Riparian land in these reaches is mostly semi-wild wetland, scrub or meadow. I don’t know if dredging up the past makes her less likely to recover from this relapse into illness.
That evening, as we walk back to her house through the fields, she seems stronger to me than she ever has, like she could walk for as long as it was still light. It feels like I am holding her back, willing her to turn and walk home with me.
27
¶ Basically furious
My mother does not have a letter from the Children’s Hospital confirming my ME/CFS diagnosis, but she does have letters she wrote to doctors and services asking for help. She also has all the appointment cards and the letters relaying negative and normal test results, and the responses to her pleas. She keeps them all in a folder labelled ‘Alice – Health’. She calls it my ‘health archive’.
‘Alice gets exhausted very easily,’ my mother wrote to one consultant. ‘Alice does not sleep easily but has never been a good sleeper. She gets an ill feeling in her chest region when she is exhausted.’
In rhetoric, but also in medicine, a report by a medical doctor is called an epicrisis, meaning ‘a second crisis’ from the Greek word for judgement or decision. Epicrises serve an explicit purpose as a contribution to medical knowledge, destined for other ‘men of science’ to study and learn from. Epicrises are also, by definition, a work in progress – a text that might be re-worked or returned to at any time, written for posterity. In his books on hysteria, Sigmund Freud wrote epicrises in order to share information with his colleagues and the public, to transmit his findings across generations, and create a community of knowledge. Epicrises are written by doctors, but there is also anamnesis, the account the patient writes themselves.
‘We just go from crisis to crisis with Alice,’ my mother wrote to the local child and adolescent mental health service.
As a mother, when you feel ill and your child feels ill, your instinct is to ask: what has caused these ill feelings? You think it might be something in your blood, or your bones, or your brain, or your lungs. It could be a pesticide 28in the air or a chemical in the products you use, a parasite, a dormant infection. If there is nothing wrong with your blood or your bones, your brain or your lungs, if all the tests come back negative or normal, that means you, as mother and daughter, are made to feel like you are bad for each other. From the outside, this kind of influence can seem dangerous.
Sometimes it is impossible to find an origin for ill feelings. I had contracted Giardia aged two, and my mother says I verbalized my persistent symptoms from when I could first speak, but it seemed my ill feelings were all read through my mother’s: they even sounded like the symptoms of atypical pneumonia, the trigger for her chronic illness. It was as if I had watched and learned how to be ill from my mother.
The doctors wrote back to my mother, and she has kept those letters too. They refer to me as if I was another symptom of my mother’s confounding ill health. A letter from an ME specialist in London to my mother’s GP confirming her original diagnosis also refers to her ‘remaining concern for her daughter Alice’, who ‘has some difficulties in adjustment and has anxieties and a variety of symptoms that superficially resemble those that her mother has’. Another letter, addressed to my mother, reads: ‘My interest in the matter’ – the matter being her concern for my health – ‘would be on the basis of a general wish for your situation to be helped by improving hers.’ The specialist writes of the unclear extent to which my symptoms reflect ‘the use of the common symptom language’ with my mother, which he refers to as ‘a familiar element in Chronic Fatigue Syndrome’, and asks whether these symptoms are in fact ‘a way of expressing (my) distress or difficulties’. I found a copy of this letter in a pile of papers relating to her own ill health, on which she had 29written the phone number for the 90s television show Changing Rooms, and a note to herself: ‘Alice is angry’.
My anger is a common theme in my mother’s letters – her anamnesis of my medical history. ‘Alice is full of anger which is often directed at me because I am ill,’ my mother writes. ‘She gets upset because she feels ill so much of the time and she can’t cope with what is expected of her.’ This is confirmed in a letter from my GP: ‘On direct questioning neither Alice nor her mother felt that she had been depressed although she undoubtedly has mood swings and has at times been low, angry and frustrated by her illness.’
If pain is a kind of evidence, anger is its antidote. ‘Art is the guarantee of sanity,’ reads the text stitched to the covers of a metal bed in Cell I (1991) by Louise Bourgeois. The second half of the quote goes: ‘Pain is the ransom of formalism.’ There is no mattress on the bed, just the covers, and it is surrounded by wooden doors, and what look like surgical instruments and glass containers. A piece of cotton in a drawer underneath reads ‘RAGE’. Bourgeois had her own language for her pain, but also a means to interpret it: her unconscious. In her sculpture and installation, the body is a site of suffering, made of marble, latex or cloth, stitched, bent, twisted and broken. ‘The subject of pain is the business I am in,’ she said. ‘To give meaning and shape to frustration and suffering. The existence of pain cannot be denied. I propose no remedies or excuses.’ Why remedy pain, and why excuse it? Pain is evidence of suffering, it’s marker. Without it, that suffering can be denied.
‘You were basically furious and wouldn’t speak to him,’ my mother says to me, about the doctor at the children’s hospital who first diagnosed me with chronic fatigue syndrome in the spring of 1998. ‘Our GP said I “needed 30to be ill” and you were “naughty”,’ she says, as if these were our real diagnoses. ‘She asked you to draw a picture and you refused.’ ME/CFS was not even my first unexplained illness. The first was called an ‘apparent failure to thrive’ – another kind of refusal, all appearances and no evidence.
I was naughty, but I was also ill. What did drawing a picture have to do with it?
I could ask why the child my mother described in her letters was so angry, but I am more interested in the question of what constituted that anger, or what seemed to be enacted in its expression.
Our diagnosis – and the symptom language we spoke – contained the histories of two centuries of gendered illness. It was as if that history was inside our actual bodies. As Adrienne Rich wrote in 1969: ‘My politics is in my body, accruing and expanding with every act of resistance and each of my failures. / Locked in the closet at 4 years old I beat the wall with my body and that act is in me still.’
Was I sick of feeling angry all day, or angry at feeling sick? I always hated being told to do things. What if I wanted to stay angry, to stay basically furious? What if I still do?
My health archive is a record of the help my mother tried so hard to get me, and by extension, herself. It is a paper trial, an archive of care and desire, anger and disbelief. This was a woman who had already advocated for her case to be referred to a Professor of Immunology, and was now advocating for her daughter, a child. Still, every attempt was doomed.
‘I am writing to you because I am very concerned about the wellbeing of my daughter Alice,’ my mother wrote to a consultant at Great Ormond Street Hospital 31for Children in London, Dr M.J. Dillon, on 10 November 1997. I was ten years old. She was in her mid-thirties. ‘Alice has been unwell both physically and emotionally for about two and a half years, which is the same length of time that I have had ME,’ she continues. ‘Before this she was fairly well, although since the Giardia bug she had when she was two, she has had tummy aches, upset tummies and leg pains. She was under our local children’s hospital because she is very small and underweight for her age. She was discharged nearly two years ago when regular visits proved that she was growing and putting on weight.’
She no longer took me to the GP; ‘nine times out of ten’ she simply let me have a day off school in order to rest. The GP did finally agree to refer me to the children’s hospital, but we would have to wait five months for the appointment and my mother was desperate. She went on to explain more about our situation, how my being ill was making her more ill, which was in turn affecting the emotional and mental health of my brother, aged eight at the time, who was ‘caught up in the middle’, and found the situation distressing too.
‘I have tried to do what I can to get help for Alice but just as it has been a battle to get appropriate care for myself it has been equally difficult to know what to do. I try and get her to school most of the time and often go against my gut feelings because of what my family and GP think about our situation. Even if Alice’s illness is the result of emotional stress, she is still suffering chronic physical symptoms and something must be done to help her and in turn me. The confrontations and trauma surrounding the situation make it impossible for me to avoid stressful situations which exacerbate my own symptoms, therefore making it very difficult to make a recovery of my own.’ 32
Despite being advised by the GP not to contact Dillon, she had done so anyway. She wanted to ask if he thought I too had chronic fatigue syndrome, and if not, whether he would he be able to point her in the direction of a therapist who could help my emotional state, indeed ‘the emotional state of the three of us as a family unit’. She enclosed a letter regarding her own health from the specialist, which explained her ‘circumstances’, details of her illness. It had taken a great deal of persuasion to arrange for her case to be referred to an immunologist in the first place, she adds. Finally, she apologized for taking matters into her own hands, but felt the situation had gone on too long. She had to ‘take steps to try and get help’.
During a symposium at the Royal Society of Medicine in 1978 on the subject of ‘epidemic neuromyasthenia’, the same Dr Dillon had reported on an outbreak of the illness at Great Ormond Street between the beginning of August 1970 and the end of January 1971. 145 patients had been admitted – all staff at the hospital, the majority of them nurses – with headaches, sore throats, nausea, pain in the back and neck and limbs, malaise, vomiting and depression, and some with sensory symptoms, faintness and blurred vision. Their symptoms lasted two to three weeks and then gradually resolved during the next two to three months, but Dillon observed the occurrence of symptomatic relapses over a prolonged period in at least 28 patients. No children who were in-patients during this period were affected, but several were referred in the years following the outbreak: five boys and two girls, aged nine to thirteen. These sporadic cases of what appeared to be the same disease amongst children showed Dillon that the condition was not limited to young adults (103 of the cases he encountered in 1970 were student nurses), and that it might have been more common in the community 33than was realized at the time. It also highlighted the possibility that adults and children with the disease might have ‘already been labelled as psychiatrically disturbed’. One particular symptom was too ‘difficult to quantify’: ‘rapid fatigability reported on exercise’ – the defining symptom of what would later be known as ME.
Dillon did not believe the illness he witnessed at Great Ormond Street in 1970–71 had a hysterical basis. Nevertheless, he deliberately limited the number of investigations undertaken in order to prevent fear and anxiety around the illness spreading to a theoretically susceptible population, knowing that this would foil attempts to discover the aetiology of the illness. Despite the fact that no specific infective agent could be isolated, evidence pointed to a possible infective cause: undoubted physical signs in many patients, some abnormalities in their blood serum and lymphocytes, and an observable biphasic pattern, which suggested infection followed by immune response. Dillon thought he might be able to find the infective particles within patients’ lymphocytes, some of which grew and multiplied in vitro, similar to lymphoproliferative disorders and infectious mononucleosis, but his investigation into these immune responses was cut short by the loss of the cultures at a relatively early stage: they all perished owing to an incubator failure. However, he felt that these techniques might be the basis of further attempts to define the cause of this disease in future outbreaks.
In January 1997, my mother received a letter back from Dillon. He was sorry to hear of my problems and indeed the problems that also afflicted my mother, ‘and hence indirectly her other child’, but, he replied, he was unable to review my case. ‘This certainly would have been something that I would have been prepared to undertake 34in days gone by,’ reads his letter to my mother, ‘but there have been rearrangements in my service to the Hospital such that my ability to provide the type of opinion you are requesting is officially unavailable and because of this I do find requests such as yours very difficult to handle.’
Unable to give a ‘clear view’ on my case from reading her letter, Dillon added that some of the features I had described to her ‘might well be those that one sees in youngsters with chronic fatigue syndromes’, but also could be due to ‘manifestations of childhood migraine’ and ‘other factors that might not be in the category of physical that could be contributing in view of the circumstances in which Alice finds herself’. On the top right-hand corner of the letter, sent 15 January 1998 (Dictated 1/12/97), is an illustration of a small child in the arms of their mother, with the phrase ‘The child first and always.’
What had happened in those two decades between 1978 and 1997, to make Dillon confident that my case probably had no physical aetiology, when he had been so convinced further lab testing of affected patients’ blood in vitro would uncover an infectious agent? The only conclusion available to me reading through my health archive was that the ‘circumstances’ in which I found myself were at least in part due to these ‘rearrangements’.
Michael Dillon is now in his eighties and is the Emeritus Professor of Paediatric Nephrology at UCL Great Ormond Street Institute of Child Health in the Faculty of Population Health Sciences. I emailed him to ask if he would be willing speak to me about his experiences at Great Ormond Street. ‘It would be lovely to meet you,’ I added. Despite the message of his letter to my mother – that he would not be able to help – he seemed kind from his comments at the 1978 symposium, and yet 35he remained unreal to me, alive only in correspondence and documentation, limited in his action by medical ethics but also bureaucracy. He would be very old by now; his experiences would disappear with his memory. I really wanted to speak to him before that happened.
He replied, saying my plan to write about my and my mother’s experience of unexplained illness sounded like ‘a major project’, and he hoped that it all went well, but was sorry to say that he was not willing to talk to me about his experience at GOSH for a number of reasons. ‘Firstly, I’m now an octogenarian, having retired in 2002, and detailed memories of disorders that at one time I was familiar with are now far from clear. Secondly, many years ago, I decided, on principle, not to become involved in such activities on the basis that I was so far removed from the front line of clinical care and current thinking that I would be at risk of misleading those asking for information.’
There was no way to tell him I didn’t want information about his patients. I wanted to know what he experienced, and how he felt about it.
‘I am really sorry to disappoint you but hope that you understand my dilemma.’
I had already fantasized about going to his house and noting down all the objects on his writing desk – I imagined he had one, for replying to emails at least – and about him telling me the story of those twenty years of lost time. I wanted to know if he was ever excited about the prospect of being at the forefront of a disease, or whether research into ME/CFS was doomed from the start. I had so many unanswered, or unanswerable, questions. And I still wanted to know: what had changed at Great Ormond Street in the 1990s; what ‘rearrangements’ had occurred so that a doctor with twenty years’ experience 36of ME/CFS in children was officially unavailable to offer an opinion on a case of a child with the diagnosis? Had he just said there were ‘rearrangements in the hospital’ to let my mother down gently? What had happened to make this man, at one time able to consult on cases of ME/CFS in children, maybe even the first person to assert that children could have the same symptoms, unable to do so? In 1978, at the RSM symposium, those who had observed the illness concluded their patients were not fabricating their illness and expressed concern that they were being treated psychiatrically. Nevertheless, my mother and I, and many others like us, were still being called hysterical twenty years later.
Like my mother, I went against my gut feelings, and sent him another email. He did not reply again.
When I first read the doctors’ letters in my ‘health archive’, I felt like I was reading about someone I didn’t know, or vaguely remembered. I always thought my mother was trying to get me diagnosed with the same illness as her, an illness that she was convinced had a physical cause, but that wasn’t true at all. My mother remembers correctly that she was blamed for making me feel angry and ill, but she has forgotten they also suggested the opposite: I was making her sick. If they fixed me, they would inadvertently fix her. These circumstances were, of course, impossible to untangle, just like our ‘shared language’ of ‘common hysterical symptoms’. It wasn’t our symptoms that seemed to have no physical cause, it was our ‘circumstances’, to quote one of the doctors when referring to our relation to one another, that made both of us very difficult to handle.
The health archive she gave me was the first archive. But there were so many more. 37
– A sick diarist’s letters to her famous brothers, and the diary she dictated to the woman she loved
– My teenage diaries, which somehow didn’t get destroyed
– An academic’s letters to scientists, physicians and journal editors on bad medical trials that numbered into the hundreds, all stored on his colleague’s blog
– A bank of anonymized blood, and a database of hand grip test scores and consent forms
– An inaccessible paper archive in a house in Scotland that hadn’t been dusted since its custodian died
– Outdated guidelines, twice postponed – and then again
– Hundreds of research papers and trial results that cannot be compared because of sprawling definitions
There was always more being added, but there were also so many gaps, so many conferences undocumented and YouTube videos deleted, and accounts that never got written, let alone saved and stored and protected.
Then there was the question of piecing together an archive of illness. As anyone who works with archival material knows, as soon as you think it holds together pieces fall away. My mother knows this well. She is a collector, an archivist, a lover of the objects loved by other people. The archives I have access to are generally not made of dusty paper and books, or clothing, like the archives my mother cares for. My archive of illness is made up of digital scans, and websites hosted on university servers, accessed mainly from bed, cheap books I can get sent to my house, and photos on my phone.
There is a copy of Carolyn Steedman’s Dust on my mother’s bookshelf, annotated, probably, with Post-it notes sticking out of the pages. In my memory, the book 38is about the material of archives, of being choked by your own dusty desire, of the muck of it getting in your hair and skin and mouth, how inhaling it can make you fall in love, inflict archive fever or mal d’archive, as Jacques Derrida famously called it in a lecture he gave in 1994, around the time my mother first fell ill. It can make you so sick you burn with passion, ‘never to rest, interminably, from searching for the archive right where it slips away’; ‘an irrepressible desire to return to the origin, a homesickness, a nostalgia for the return to the most archaic place of absolute commencement’. In this sense, archive fever is a kind of relapse.
39
¶ Unknown aetiology
The first outbreak of what was then called ‘epidemic neuromyasthenia’ occurred in the Los Angeles area in May 1934. There had been an unusual prevalence of poliomyelitis, commonly referred to as polio, in California for the season, of which localized epidemics had begun to appear in around 1900. Medical and nursing staff of Los Angeles County General Hospital began to present with what initially appeared to be polio – a systemic infection in the membrane surrounding the brain and spinal cord, affecting the whole body of the patient – but their symptoms were inconsistent with the disease, suggesting this infection was somehow related to polio and yet altogether new. Double vision, constipation and retention of urine were more common in these new patients, and weakness occurred without the usual severe atrophy; pain and muscle tenderness, tingling and excessive skin sensitivity persisted for longer. Members of staff admitted to the hospital also presented with mental disturbances, loss of concentration and lapses of memory, sleep disturbances, fatigue after walking short distances, and what was termed ‘emotional lability with hysterical episodes and trophic changes’. Recurrences of systemic and neurological symptoms were frequent, and, in some cases, patients were more disabled by a relapse than by the original illness. The main feature that distinguished this new infection from polio was its death count: although a high number of those affected fell ill – a total of 198 staff at the hospital, a case incidence of four-and-a-half per cent – none actually died.
There was, however, clearly something wrong. Pathological changes found in patients dying from polio in the 1934 Los Angeles epidemic, and in monkeys 40inoculated with the Californian strain of the virus, showed differences from those previously reported in polio. Destruction of neurones was reduced and there was more marked diffuse perivascular round cell infiltration – or inflammation – in the samples. Observers of this epidemic concluded that the disease was spread by direct personal contact, and not by contamination of the hospital milk or food supply, but they couldn’t find a definitive cause – either the strain was new, or they were dealing with a disease of unknown aetiology.
As members of the hospital staff most closely associated with patients and more likely to live in hospital residences, student nurses were the most affected, which meant three quarters of those affected were women. Considering many men have a diagnosis of ME/CFS, I have always wondered where the association between the diagnosis and women had actually come from. Perhaps it arose from the likelihood of nurses being affected in the early outbreaks of the disease, and of those nurses being women. The LA County Hospital outbreak might have been the first outbreak like it, but it was not the last.
In October 1957, Medical Staff of the Royal Free Hospital, then located on Gray’s Inn Road in London, reported an outbreak of an ‘obscure illness’, which had occurred two years earlier. On 13 July 1955, a resident doctor and a ward sister were admitted to hospital. Within two weeks, more than seventy members of the staff were affected. The hospital was closed because of the threat to the health of patients of what appeared to be an infection affecting the nervous system. Besides, a large number of nurses had taken sick, making it impossible to keep the Royal Free operational. By 24 November, 292 members of the medical, nursing, auxiliary medical, ancillary and administrative staff had been affected by the 41illness, and 255 people were hospitalised. Cases seemed to vary, both in the content of the extensive range of symptoms and signs, and the speed with which the illness evolved. Patients presented with malaise and headaches, but also sore throats, dizziness, nausea, and pain in their abdomen, limbs and back. As in LA in 1934, extensive investigations done in the hospital and many other institutes, including potential toxic causes, failed to reveal an aetiological agent of an infective nature, and no characteristic biochemical changes attributable to the disease were found. In many patients, the symptoms waxed and waned in intensity over a long period. These symptoms, the most characteristic of which was prolonged painful muscle spasms, were frequently associated with what the doctors treating them called ‘disproportionate depression and emotional lability’.
To obscure