9,59 €
Mehr erfahren.
- Herausgeber: Luath Press
- Kategorie: Sachliteratur, Reportagen, Biografien
- Sprache: Englisch
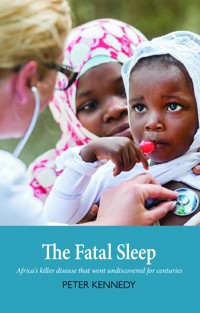
The bite of the tsetse fly - a burning sting into the skin - causes a descent into violent fever and aching pains. Severe bouts of insomnia are followed by mental deterioration, disruption of the nervous system, coma and ultimately death. Sleeping sickness, also known as Human African trypanosomiasis, is one of Africa's major killers. It puts 60 million people at risk of infection, occurs in 36 countries in sub-Saharan Africa, and claims the lives of many thousands of people every year. Transmitted by the tsetse fly, trypanosomiasis affects both humans and cattle. The animal form of the disease severely limits livestock production and farming, and in people the toxic effects of the treatment for the brain disease can be as painful and dangerous as the disease itself. Existing in the shadow of malaria and AIDS, it is an overlooked disease, ignored by pharmaceutical companies and largely neglected by the western world. Peter Kennedy has devoted much of his working life to researching sleeping sickness in Africa, and his autobiographical account shares not only his trials and experiences, evoking our empathy with the affected patients, but an explanation of the disease, including its history and its future. Interwoven with African geography, his compassionate story reveals what it is like to be a young doctor falling in love with Africa, and tells of his building of a vocation in the search for a cure for this cruel disease.
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 467
Veröffentlichungsjahr: 2020
Ähnliche
PETER KENNEDY is a world authority on infectious diseases of the nervous system. He trained as a medical doctor, and then a neurologist, in various institutions in London, and holds MD, PhD, and dsc degrees and two masters degrees in Philosophy (M.Phil, M.Litt). One of the youngest doctors ever appointed to lead a neurology department in the UK, he held the Burton Chair of Neurology at Glasgow University, Scotland for 29 years (1987–2016), where he is currently an honorary senior research fellow carrying out mainly research and teaching. He is a fellow of the Royal Society of Edinburgh and the Academy of Medical Sciences. He is the coeditor of two textbooks on neurological infections and has published more than 200 scientific papers in learned journals. He has also written five novels. He has received several awards for his scientific work including recently the Sir James Black Medal of the Royal Society of Edinburgh (its senior prize in the life sciences), and the Pioneer in Neurovirology Award of the International Society for Neurovirology of which he was President for six years. He received the CBE in the 2010 New Year Honour’s List for services to clinical science.
He became enamoured with Africa as a medical student on an elective in Zambia in the 1970s, and had visited Africa 28 times since. Now part of major international efforts to increase awareness of and funding for research into sleeping sickness, he is one of only a handful of medical doctors specialising in the disease and is dedicated to finding a cure.
The Fatal Sleep received a ‘Highly Commended’ award in the Popular Medicine category of the 2008 British Medical Association (BMA) Medical Book Competition.
This book is very readable and entertaining at the same time and sheds some light into how fate sometimes determines the outcome of a medical career. Professor Peter Kennedy has immersed himself totally in this commitment to the eradication of trypanosomiasis and his book is a testament to that
SCOTTISH MEDICAL JOURNAL
This is not a dry academic book, rather it reveals a clinical scientist who delights in his work and who shares his enthusiasm with his readers... If Kennedy’s book not only awakens readers to the problems of sleeping sickness but is the catalyst for new partnerships between North and South, it will have succeeded far beyond its original, and in this wider sphere, more limited aim
BRAIN
His book, as a memoir of a life in trypanosomiasis research, calls much-needed attention to a widespread disease of poor and isolated Africans, for whom pharmaceutical companies should spend more time developing therapeutic drugs
JOURNAL OF CLINICAL INVESTIGATION
Kennedy has provided a comprehensive account of the history of sleeping sickness, the biology of the trypanosome and of its tsetse fly vector, and how the disease affects humans and animals. These accounts are clear, comprehensive, and free of jargon and should be easily understood by the interested general reader with little scientific background... Kennedy is to be congratulated on writing a book for a general audience about an important but neglected tropical disease, and he has generously offered half his royalties to charities working to alleviate its results
BRITISH MEDICAL JOURNAL
The book has broad appeal, containing science, medicine, politics, economics, and geography. It closes with challenges and a call for organizational support to eradicate this disease. The reader would do well to allot a block of uninterrupted time for this relatively short book (just over 200 pages), because once started, it is hard to put down. It is a book you will want to share with family, friends, and colleagues
NEUROLOGY
The Fatal Sleep has a little bit of everything, and as such it is a great read… In this book Kennedy draws us into his passion for this disease, and indeed for all of Africa itself... As for medical readers I think they will be delighted, charmed, horrified and fascinated in equal measure. And even if the book does nothing more than raise awareness among medics of this terrible problem, it will have achieved a great deal.
ADVANCES IN CLINICAL NEUROSCIENCE AND REHABILITATION
First published 2007
Second edition 2010
This edition 2019
eISBN: 978-1-912387-86-1
The paper used in this book is recyclable. It is made from low chlorine pulps produced in a low energy, low emissions manner from renewable forests.
Printed and bound by
Ashford Colour Press, Gosport
Typeset in 10.5 point Sabon by
3btype.com
© Peter Kennedy 2007, 2019
Fifty per cent of the author’s royalties generated from sales of this book will be donated to Médecins Sans Frontières (MSF) to promote human health in Africa.
This book is dedicated to all the sufferers from sleeping sickness in Africa.
Acknowledgements
Many people have assisted me in the writing of this book, and each person has contributed in their own particular way. First and foremost, I must thank Max Murray who first introduced me to the problem of African trypanosomiasis, and has been a superb colleague, friend and mentor for the last 18 years. He read all the chapters in detail, and made a large number of suggestions and corrections, all of which have improved the original manuscript. Without Max, this book would never have been written. I also want to thank Joseph Ndung’u, who has played such a major part in my work and experience in Africa. Joseph has also been a great friend and colleague, and has taught me a great deal about sleeping sickness, Kenya in general, and the nature of leadership. He also read all the chapters and expertly advised on details of the text. Peter Holmes has also helped me considerably, especially in explaining so clearly the problems of tsetse fly control and drug treatment in animal trypanosomiasis. He also checked most of the chapters and made valuable suggestions. The fourth key person I wish to thank is Jane Nevins, a highly experienced American editor, who has given so generously of her masterly advice in the art of book writing. Her constant encouragement has been crucial, and she taught me a great deal about popular science writing, and, above all, the absolute necessity to make such writing both accessible and interesting to the reader. I have done my best to aspire to her high standards, and readers will have to judge for themselves whether I have succeeded.
I want to thank all of my past and present colleagues in the trypanosomiasis research group in Glasgow for their expert and inspirational collaboration. These include: Jean Rodgers, who also read some of the chapters; Frank Jennings; Barbara Bradley; Chris Hunter; Charity Gichuki; David Eckersall; Joanne Burke; and John Gow. Our other fine research collaborators outside Glasgow whom I wish to thank are Jeremy Sternberg, Jorge Atouguia, Susan Leeman, Krister Kristensson and Dennis Grab.
Several colleagues provided valuable assistance to me by reading individual chapters, or parts of chapters, or by giving advice on specific topics. These colleagues include the following: Serap Askoy, Christian Burri, Mike Turner, Hugh Willison, Mike Barrett, Malla Rao, Keith Vickerman, Martin Odiit, and Ian Maudlin. Of course none of these are responsible for any errors that I may have made, although I have gone to considerable lengths to avoid these. I am particularly grateful to Tom Dent for his reading of Chapter Two and sharing with me his recollections of life as a mine doctor in Zambia. I have changed the names of some individuals in the early chapters, usually because I have been unable to contact them after so many years.
I am most grateful to James Beaton of the library at the Royal College of Physicians and Surgeons of Glasgow for providing me with interesting information on the life of David Livingstone, and Karen Carruthers of the David Livingstone Centre in Blantyre for providing useful information about, and providing the photograph of, Livingstone. I am grateful to Anna Smith of the Wellcome Trust for providing some of the historical photographs. I owe a particular debt of gratitude to Colin Burns of the Clinical Physics department at the Southern General Hospital for his expert and generous help in producing all the photographs in the book, a task that was quite formidable. I also thank Marian Martin of our Medical Illustration department for her assistance with the figures. I was also most fortunate that Mike Shand, an expert cartographer in the Geography Department in the University of Glasgow, produced the map of Kenya in the beginning of the book. I am also grateful to the bmj Publishing Group, the Gyldendal Denmark (Karen Blixen’s Danish publishing house) and the Rungstedlund Foundation for giving me permission to reproduce copyright material.
Three friends also gave me a great deal of encouragement for the book in its early stages of gestation, and for this I would like to thank Elaine Snell, Douglas Hutchison and Heather Armstrong. One should never underestimate the power of encouragement. I am also very grateful to Gavin MacDougall, Director of Luath Press, for his great interest in the subject of sleeping sickness and his welcome decision to publish the book. He and his staff, especially Catriona Vernal, in their Edinburgh office have been a pleasure to work with. Finally, but of course not least, I want to thank my wife Catherine for her constant encouragement between the many solitary hours of writing, and for helping so much with the meticulous research involved in describing the historical and geographical aspects of the places in Africa that I have worked in.
Contents
Acknowledgements
Foreword
Preface to the First Edition
Preface to the Current Edition
List of Acronyms and Abbreviations
PART ONE KINDLING THE FLAME
CHAPTER ONE An Opportunity Arises
CHAPTER TWO Copper Mines and Spitting Cobras
PART TWO THE FLY AND THE MOUSE
CHAPTER THREE The Problem of Sleeping Sickness
CHAPTER FOUR Africa Revisited
CHAPTER FIVE Sleeping Sickness in the Human Patient
CHAPTER SIX The Mouse Model of Sleeping Sickness
CHAPTER SEVEN A Meeting with the Animal Reservoirs
CHAPTER EIGHT Fear and Wonder in Africa
PART THREE HOPE FOR THE FUTURE
CHAPTER NINE Further Afield and the Ugandan Dimension
CHAPTER TEN Future Priorities and Challenges for a Cinderella Disease
CHAPTER ELEVEN An Overview of Some Recent Developments in Sleeping Sickness
Postscript
Sources and Notes
Glossary of Medical and Scientific Terms
Foreword
THIS IS A REMARKABLE BOOK. It is filled in equal measure with passion for science and compassion for the people afflicted with this cruel disease. Yet it ends with hope.
The trypanosome, the organism causing the disease, plays ‘hide and seek’ and is difficult to find in the body. It is difficult to eliminate its vectors, and the disease is difficult to treat and cure. Yet sleeping sickness is an orphan disease, massively and sadly neglected by drug companies. They cannot recoup the billions they might have to spend on research to find a cure, when the only countries affected are amongst the poorest in the world, so that they cannot recover their costs from sales.
This book describes clearly all the difficulties. Suppression of the organism in vectors has not been successful so far. The current best available drug for the brain disease is so unpleasant that one patient described it as ‘like having chilli peppers injected into your heart’. Untreated, the disease is 100 per cent fatal but this drug kills one in 20 of those who take it. The final irony lies in the agonising decision of doctors who have to make the diagnosis before deciding where to treat, on the basis of unreliable or inconclusive tests.
Dr Kennedy is passionate about his scientific research. He describes the body’s immunological defences that can be overcome by the wily trypanosome. There is now a mouse model that should accelerate the search for better drugs. His compassion lies in his feelings for Africans, often surprisingly cheerful though surrounded by death and disease, including AIDS and malaria as well as sleeping sickness. He also writes lyrically about the beauty of Africa.
Yet finally I find two distinct strands of hope. The first is that there is still a generation of European doctors who are prepared to follow in the footsteps of Livingstone and Schweitzer, the missionaries who went to this troubled continent. Dr Kennedy went out 18 times in 31 years.
The second line of hope is that much of the pioneering scientific research has now been done and collaborative research is now successful between the African governments, world health agencies and private donors like the Gates Foundation. It is difficult not to feel some shame at the way European countries have exploited Africa in the past, but now a more respectable story is unfolding. I believe diseases like sleeping sickness can be controlled, if not eliminated. This excellent book is an inspiring tribute to the ways in which that happy day may be accelerated.
Sir Roger Bannister
March 2007
Preface to the First Edition
I HAVE WRITTEN THIS book for one main reason: to tell the non-scientist about the history and profound importance of human African trypanosomiasis, also known as sleeping sickness. The history of African trypanosomiasis in man and animals reflects the history of vast regions of the African continent itself. At the present time, one third of Africa is held captive by the tsetse fly which is so adept at transmitting the disease, and no less than 60 million people are at risk of acquiring the infection. The disease also has a profound effect on limiting the quality of life throughout sub-Saharan Africa, and both farming and livestock production have been greatly reduced by the twin scourges of the trypanosome parasite and the tsetse fly. Yet treatment of sleeping sickness has hardly progressed over the last century, and the most commonly used drug for treating late stage disease where the nervous system has been invaded actually kills one in 20 of the people who receive it. I sometimes ponder that figure and ask myself whether it can really be true. But sadly it is so. Since the infection is always fatal if untreated, African patients are at very high risk from dying from the treatment as well as the disease. Until quite recently, Western governments have shown little interest in supporting research into new drugs for sleeping sickness or for providing major funds to improve the infrastructure to better control the disease. Until now the power of the parasite and the fly has been predominant. But that does seem to be changing, slowly.
With these grim figures in mind, I decided to undertake a medical and literary journey into Africa, and I wanted the lay reader to join me and, most important of all, to truly understand everything I had to say about the disease. This is certainly not a textbook, but a popular science book that is aimed to communicate in what is currently called a ‘reader friendly’ way. I thought it would be fun and interesting to trace the origins of a personal passion for Africa, so I started off with some autobiographical vignettes. Fast forwarding to a welcome return to Kenya, we then learn about the institutions that have been set up in Africa to research the disease. We then reach the true horrors of the human disease and witness its extreme cruelty at first hand. After an encounter with the animal reservoirs, we look to the future and recognise all that various organisations are now doing to control the disease and to develop better drug therapy.
Most of all, I wanted this book to be enjoyable and easy to read. This has involved a completely different writing style than scientists are used to, and therein lay the real challenge. For this reason, I have continuously pestered many friends and colleagues to read various parts to test the waters so to speak, and I hope I have succeeded, at least in part, in explaining quite difficult scientific concepts while transmitting the wonders and extreme beauty of Africa. The various geographical and historical details that have been interspersed in the text have been included not only for their contextual relevance, but also to make the book easier to read. I believe that only chapter six might prove slightly challenging for the non-scientist. But I do urge the reader to persist even if it is a little tricky – just remember that it was even worse for me writing it! If that proves impossible, then the reader would not come to any harm by perusing just the opening and closing paragraphs of that chapter.
If I manage to make more people aware than before of the curse of sleeping sickness in sub-Saharan Africa, then this book will have succeeded in its most important aim. In that endeavour, let me now be your guide.
Peter Kennedy
March 2007
Preface to the Current Edition
SINCE THE SECOND EDITION of this book was published as a paperback in 2010 there have been several developments in our knowledge and understanding of sleeping sickness. It therefore seemed appropriate to produce a third and updated edition that would reflect these advances. I have now written an additional chapter (11) which provides an overview of what I think are the most significant advances in the field while making very few changes to the main text which I have left largely as it is. These advances have been summarised for five different aspects and this has been supported by several additional references for those who want to read to some of the original studies. I am grateful to my colleagues Professors Max Murray and Joseph Ndung’u for casting their expert eyes over this chapter when it was at the draft stage.
I feel I must mention my deep sadness at the recent death of the eminent Sir Roger Bannister who had so kindly written the foreword to the original 2007 hardback edition which is reproduced here. I knew him personally for many years and he was an inspiring figure. In my view, and I suspect also his, his seminal contributions to medical science and clinical neurology were at least, if not more, important to mankind than were his groundbreaking achievements in athletics.
Peter Kennedy
November 2019
List of Acronyms and Abbreviations
ADB
African Development Bank
AIDS
Acquired Immunodeficiency Syndrome
AU-IBAR
African Union-International Bureau for Animal Resources
BBB
Blood-Brain Barrier
CATT
Card Agglutination Trypanosomiasis Test
CGIAR
Consultative Group on International Agricultural Research
CNS
Central Nervous System
CSF
Cerebrospinal Fluid
CTVM
Centre for Tropical Veterinary Medicine
DALY’S
Disability of Adjusted Life Years Lost
DEET
diethyltoluamide
DFID
Department for International Development
DNDi
Drugs for Neglected Diseases Initiative
EAVRO
East African Veterinary Research Organisation
EATRO
East African Trypanosomiasis Research Organisation
EEG
Electroencephalogram
EMA
European Medicines Agency
ETEC
enterotoxigenic Escherichia coli
EU
European Union
FAO
Food and Agriculture Organisation
FDA
US Food and Drug Administration
FITCA
Farming in Tsetse Controlled Areas
GCS
Glasgow Coma Score
GIS
Geographic Information Systems
GPS
Global Positioning Systems
HAT
Human African Trypanosomiasis
HIV
Human Immunodeficiency Virus
IAEA
International Atomic Energy Agency
ICIPE
International Centre for Insect Physiology and Ecology
IFN
Interferon
IL
Interleukin
ILCA
International Livestock Centre for Africa
ILRAD
International Laboratory for Research in Animal Diseases
ILRI
International Livestock Research Institute
ISCTRC
International Scientific Council for Trypanosomiasis Research and Control
ITC
International Trypanotolerance Centre
KARI
Kenya Agricultural Research Institute
KEMRI
Kenya Medical Research Institute
KETRI
Kenya Trypanosomiasis Research Institute
LIRI
Livestock Health Research Institute
LRA
Lord’s Resistant Army
MRI
Magnetic Resonance Imaging
MSF
Médecins Sans Frontières
NARO
National Agricultural Research Organisation
NIAID
National Institute of Allergy and Infectious Disease
NIH
National Institutes of Health
OAU
Organisation of African Unity
ODA
Overseas Development Administration
PAAT
Programme Against African Trypanosomiasis
PATTEC
Pan-African Tsetse and Trypanosomiasis Eradication Campaign
PTRE
Post-Treatment Reactive Encephalopathy
RDTS
Rapid Diagnostic Tests
REM
Rapid Eye Movement
RTTCP
Regional Tsetse and Trypanosomiasis Control Programme
SAT
Sequential Aerosol Drift technique
SIT
Sterile Insect Technique
SP
Substance P
TDR
Special Programme for Research and Training in Tropical Diseases
TRC
Trypanosomiasis Research Centre
UTRO
Uganda Trypanosomiasis Research Organisation
VSG
Variable Surface Glycoprotein
WHO
World Health Organisation
PART ONE
Kindling the Flame
FIGURE 1
Map of Kenya showing key locations described in the book (Mike Shand)
CHAPTER ONE
An Opportunity Arises
APRIL 2001: the rainy season in Kenya and five months before the fall of the twin towers. The world was still sleeping and so was I. But that delicious twilight state between dreaming and awareness that was broken now and then by the jolting of our vehicle was just an illusion. How was I to know that my own nemesis was approaching just a few miles away? Ominous storm clouds were rising like grey mountains on the horizon soon after our departure from Busia in Western Kenya, only four miles from the Ugandan border. This meant a dangerous drive back to our regional base in Kisumu, 120 km away. But we had not imagined just how hazardous this passage home would be. One thing we knew for sure – it was critical to return to Kisumu before nightfall because of the extreme danger of night time driving on those hideously damaged roads. Craters of death do not respect good intentions in this part of the world.
So my long time friend and colleague Joseph Ndung’u, our driver Moses and I set out, maybe a little foolishly, in our lightly loaded Land Rover knowing full well that our route was taking us through the centre of a developing tropical storm. In Africa anxiety often trumps good judgement. Anything to get away from these roads. Anything to get home in one piece. The main danger came from the murderously heavy rain, monsoon quality, which soon came thundering down all around us. We gripped the seats and the window straps tightly as the vehicle swayed in surprising silence, and I watched the heaving of Moses’ broad shoulders as he wrenched the wheel first left, then right, and then left again, while all the time heavy goods lorries bound for Uganda were hurtling towards us. Every time we swerved my arms felt sickened with the strain. The lorries seemed strangely ruthless in their apparent disregard for all other vehicles on the road while they advanced towards us, long dusty monsters with a continuous snake-like sideways motion as if they were trying to intimidate us into submission. Add to this the constant need to negotiate the widest and deepest potholes that I have ever seen in any road in the world, almost magnificent in their appalling size, and then maybe you will understand the tense and rather chilly atmosphere that the sudden, nauseating jolt of our Land Rover so forcefully punctured. I silently but violently cursed, not for the first or last time, the local political rivalries that had led to such a sorry state of neglect of the country’s roads. ‘Opposition stronghold here,’ Joseph knowingly told me over his shoulder. This made me curse again, not so silently this time, and for a moment I experienced a surge of cold rage that made me feel even worse. This was a worrying and also deeply disappointing way to finish a very successful field trip which had left both Joseph and I feeling particularly gratified. Our visit to the sleeping sickness treatment hospital in Alupe had been one of the most productive so far, and had provided the seeds for several new ideas about this terrible disease we were fighting. Just for a while we had bordered on elation.
Looking back now at this incident it is evident that there was not one but four different problems – the driving rain, the monstrous lorries, the crater-like potholes and the lack of rear seatbelts. But it was this last factor that was the most significant for our safety. A speeding Uganda-bound lorry, skidding slightly because of the wet road, careered towards us leaving almost no clear road between itself and our Land Rover. Moses was left with no option but to swerve rapidly to avoid a collision, likely to be fatal for us, but in doing so our vehicle plunged at high speed into a particularly deep pothole. The Land Rover hurtled sharply downwards. Unrestrained by seatbelts, I sailed suddenly upwards, ramming the top of my head sharply, but not deeply, into the roof of the vehicle. I was stunned but not really hurt. Had I been any taller or the pothole any deeper then the damage would have been much greater. This event had three consequences, two definite and one suspected: both Joseph and Moses were, quite reasonably, horrified that I might have been injured: all my neck movements were extremely sore for weeks, if not months, afterwards; and I think I probably gained about half an inch in height as the stretching force of my sudden flight upward seemed greater than the compression when I hit.
Anyone who ever worked in Africa has a story like this to tell. My own time in the ‘Dark Continent’ has now spanned 18 individual visits over 31 years since medical student days, but the last 16 of these have mainly been spent in Kenya studying sleeping sickness. However much the perils come to mind – and there have been many like our dangerous drive that April evening, some worse and far more life-threatening – one simple question always arises: why do my colleagues and I keep going back? Why do these people risk serious and potentially chronic illness, the often very unpleasant side effects of anti-malarial drugs such as nausea, abdominal pain and psychiatric symptoms, the chance of physical injury from road traffic accidents, and sometimes isolation and fear, when they could be cocooned in relative safety back home in Europe or America? It’s really strange because when I’m in Africa some of me wants to be back in Scotland, and when I’m nice and safe back home in friendly Glasgow then most of me wants to be back in Africa. The grass is always greener, especially on the other side of the world.
While the answers to these questions are not immediately apparent, I’ll try hard in this book to provide some kind of an explanation, and one that really does ring true. Several of my medical colleagues who share a passion for Africa have often asked themselves the same question and also seem surprisingly unsure of the reasons for their repeated visits to and their enduring fascination with Africa, its people and its diseases. Mental as well as medical notes are often compared, and it is probably the dark continent itself, with its rich fabric of physical beauty, people, spirit and mystery, which is almost as much a magnet in this as the intrinsic interest of the diseases which we all study and the commitment – or even obsession – which many of us have to discovering more about the causes and cures of such dreadful killers as sleeping sickness and malaria. And one shouldn’t forget that these two diseases can frequently occur together in the same person.
My colleagues and I – and that includes medical doctors and scientists – work on these diseases mostly in Africa, but the implications are global. Not only do malaria and sleeping sickness help deprive the worldwide economy of Africa’s all but untouched potential, but, like Severe Acute Respiratory Syndrome (SARS) and West Nile infection of the nervous system, these diseases can travel. Malaria, of course, is familiar to people in North America and Europe, not only because of its reputation for killing millions of people worldwide, but also because some Western tourists to the African continent, distressed at the side effects or unaware of the great dangers of stopping, unwisely discontinue their anti-malarial tablets, and develop the disease weeks after their return. And a few die of its complications. Malaria is also an important occupational hazard for soldiers who are deployed in the tropics. A stunning example of this hazard occurred in 2003. Two hundred American marines who returned from service in Liberia in West Africa developed malaria, and 43 of them were ill enough to be hospitalised. Although none of the soldiers died, two of them developed cerebral malaria, the most dangerous form of the disease and one that has a 20 per cent mortality rate. Why so many soldiers developed the disease despite taking appropriate preventive anti-malarial tablets is not known for certain, but it seems likely that their blood levels of these preventive drugs were not adequate. A constant threat to travellers to Africa is that malaria parasites will develop resistance to these drugs, but no convincing evidence of resistance was apparent in the case of these unfortunate soldiers.
Sleeping sickness is the common name for human African trypanosomiasis, to give it its full medical title. For many people the words conjure up images of a mysterious and terrifying disease of the jungle and veldt, afflicting intrepid Western explorers and rural native Africans with scant access to medical care. That image is not entirely inaccurate, but this disease is staggeringly widespread and its potential for harm is no longer limited to Africa. Sleeping sickness is more exotic to us, but that could very well change. Global business and increasing tourism to Africa, together with easier and more accessible air travel between America, Europe and Africa, carries a real risk of Western travellers returning home with sleeping sickness. Several cases of Europeans developing this disease have appeared in medical literature, and travellers from America and other Western countries, as well as Asia, are vulnerable too, as their increasing numbers and time in Africa raise the odds of contact with the tsetse fly, the principal transmitter of the human form of the disease.
Sleeping sickness is often referred to as one of the ‘neglected diseases’. Others are Chagas disease in South America, and visceral leishmaniasis, a widespread disease found in regions of the Middle East, Asia, South America, the Mediterranean and Africa. These diseases affect very large numbers of people in the underdeveloped world, are always serious, and often fatal. Moreover, current therapies for them are frequently out of date, not very effective and sometimes toxic. In the case of sleeping sickness, the most frequently used drug for nervous system disease actually kills five per cent of those who receive it, which is a figure almost beyond comprehension. When I mention this figure to friends and medical colleagues they sometimes suspect I am exaggerating, yet this is indeed the case. But the numerous people affected by these diseases are very poor, and the populations they represent are unable to pay for suitable health care. As a result, the Western pharmaceutical companies who have the potential to develop more effective medicines for these diseases have so far shown little interest in doing so. With very little prospect of either short or long term financial return it is hardly surprising that the drug companies have had little or no incentive to invest in the therapeutics of these diseases. Market forces do not favour such investment despite the terrible price in morbidity and mortality that has to be paid by the millions of poor people who suffer from these ghastly conditions which have such magnitude and severity. This is a global public health need that both the private and public sectors in the world have so far consistently failed to address. With less than 10 per cent of the global health research spending being directed towards the health needs of 90 per cent of the world’s population, there is indeed a ‘fatal imbalance’ between the severity and scale of these diseases and the relatively meagre resources that are being devoted to them.
Despite considerable publicity in the medical press in 2000 when no treatment could be immediately found in London for two travellers who had recently returned from Africa with sleeping sickness – eventually medical authorities obtained and administered the drug (suramin) – Western health care systems are ill prepared for this kind of eventuality. However, some good signs are appearing. In 2000 the Bill and Melinda Gates Foundation awarded US$15 million to a multidisciplinary research programme involving teams in America, Africa and Europe to develop more effective drug therapies for sleeping sickness and leishmaniasis in Africa. The US National Institutes of Health also provides funding for research into this disease, as does the UK’s Wellcome Trust research charity and other agencies. So, clearly the message is getting through to some of those who are in positions to help the situation. For now it may be enough for people to be aware of the potential problem for Western civilisation and the existing problem in Africa where 60 million people are at risk from developing the disease.
That is the background to our story and a theme that will recur as we explore the nature and implications of sleeping sickness. Yet despite the scale of this health problem, there is so much that is wonderful and magical about working in Africa, which we shall also visit. For myself, like so many visitors, perhaps the most enduring and evocative visual image of Africa is the remarkable quality of the light, both mystical and clear, especially in the early evening when it gently illuminates and seems to bathe the countryside, whether it be in the majestic regions of the savannahs or the peaceful green hills closer to the cities. African light has a quality of serenity and stillness that is almost magical. Some visitors to Greece have said similar things about the light found there. While I have certainly seen the exquisite nature of that light too, especially in the mountainous and mystical regions near Delphi, somehow it is distinctly different from that which is uniquely of Africa.
So how did all this happen? To explain that I first have to take you back to the late 1960s.
Some people fall in love with Africa as children, from storybooks or movies, or the influence of a charismatic teacher, but that wasn’t the case for me. Instead I had a keen interest in biology fieldwork in the sixth form (which is more or less equivalent to the 12th grade in the US). I became progressively enamoured of the study of animal habitats in the countryside, largely due to the efforts of a young and extraordinarily enthusiastic biology teacher. Typically, Mr J would decide to discontinue or cancel a conventional school lesson and cart us all away to a pool near the school, which, until that moment, had seemed to be only that. By the time he had finished describing and demonstrating the myriad of interdependent microscopic animal and plant life contained within such a modest pool, indeed in a single drop of water, we would appreciate our previous blindness and marvel at the ecological wonders that had been there all the time had we only possessed the knowledge and insight to look for them.
Thus prepared, I decided to be a doctor and entered the 18-month ‘pre-clinical’ medicine course at University College London (UCL), leading to the academically demanding examination (called the ‘second MB’) a prerequisite to the three year clinical course at what was then University College Hospital (UCH) Medical School, which is now part of a much larger amalgamated medical school comprising several former medical schools). The University’s impressive classical main building had been used some years before as the fictional hospital for the first Doctor in the House film starring Dirk Bogarde as the young Simon Sparrow. One sometimes half expected to see a Sir Lancelot Spratt lookalike emerge briskly from his Rolls Royce and bound up the building’s steps to meet an admiring and obsequious medical and nursing entourage. As it happens, despite this character’s flamboyant and bullying personality, wonderfully immortalised by the actor James Robertson Justice, he was actually rather benign compared with some of the real medical bullies who unfortunately appear here and there on the landscape of our profession. Such behaviour on the hospital wards was just about tolerated up to about 10 years ago but is now largely regarded as anathema and seldom occurs to any degree. Besides, there is a very useful golden rule: one should always be nice to juniors on their way up the career ladder because you want them to be kind to you when you are on the way down. I have endeavoured to observe this rule.
The college and the hospital were located on opposite sides of Gower Street in London, a street steeped in a rich medical and intellectual history. While the concept of a teaching hospital is now extremely familiar to people in both North America and Europe, UCH was the first British hospital that was built, in 1833, specifically for teaching purposes as well as service delivery to patients. The great UCH surgeon Robert Liston (1794–1847) was the first British surgeon to operate on a patient under ether anaesthesia, and his original operating table was still displayed in the library there. Sir William Gowers (1845–1915) one of the pioneers of Clinical Neurology, also practised at UCH, a man of great intellectual brilliance. His name also continues in the ‘Gowers’ ward at the renowned National Hospital for Neurology and Neurosurgery, Queen Square in London, where he also worked during his career. On the other side of Gower Street at UCL, Jeremy Bentham (1748–1832), the legendary philosopher and pioneer of the doctrine of Utilitarianism, was memorialised for many years by a remarkably lifelike model which actually contained his bones! In a tremendous act consistent with his creed, Bentham had left his body for the purpose of anatomical dissection. Also, one of the four junior student ‘houses’ at University College School was named after Bentham (I know because I went there). But as students we were never fully aware of the intellectual heritage of Gower Street, as we were too wrapped up in our own medical student microcosm. We were oblivious to the rich tapestry of the outside world in what was, as it is now, one of the most exciting cities to live in. But that was typical of student life for many young people at the time.
I started the pre-clinical course in October 1969, a time that seems conformist in retrospect. The evolutionary biologist Julian Huxley, the philosopher Bertrand Russell and the author J.R.R. Tolkien were still alive, decimalisation was not yet implemented, the Beatles were still playing together (just about), Rod Laver had just won the Wimbledon singles title for the second year running, George Best was still in his football heyday, a Labour government was still in power (but that would change the following year) and racial prejudice was still widespread with nothing like the social integration of different cultures that one now takes for granted.
The typical annual student grant for those living at home was comparatively low at about £330. While this sum seems ludicrously paltry now, in fact it was very useful then, though a significant part of it was used to buy medical books. Fortunately I did not need to buy a skeleton for anatomical study as I inherited ‘Napoleon’ from my older brother Roger who had started the same medicine course there two years ahead of me. This diminutive skeleton was real, unlike most of those used by medical students today, and I believe had once been a man living somewhere in Asia. He still lives with me in a large cardboard box in my house in Glasgow where he is much respected and well looked after, and I have never ceased to remember that he was once a human being just like me.
On the very first day at UCL, two fellow students befriended me, and we would become a triumvirate throughout our college years. Oliver, whom I met on the first day on a creaking but elegant wooden staircase en route to the anatomy department, would become a lifelong friend and play a key role in my forming a bond with Africa. Oliver and I were aware of each other’s existence from the outset, as one of his close relatives was a very good friend of my parents. Oliver was extremely intelligent – he could dispose of The Times crossword puzzle in minimum time – and also very original in his way of thinking and in his general perception of the world. He saw people and things clearly for what they really were, devoid of any falseness, and this unusual quality is just as evident today. He was also very cultured compared with most of his peers, with a remarkable knowledge of musical history, and an extraordinary thirst for acquiring new knowledge and novel ideas. Such admirable qualities as these were not necessarily useful in studying medicine as it was systematically taught at that time; the necessary acquisition of vast numbers of facts, learned almost by rote, does not always come easily to people with highly intelligent and original minds. I was fortunate in having a good memory for factual information, so this was less of a problem for me. (Today the pendulum has swung in the opposite direction with an emphasis on understanding principles rather than facts, to the extent that it is quite possible for medical students in their third year to be unsure of the course of the three main nerves supplying the hand.) We also shared a very youthful appearance, and looked somewhat similar (as we still do), so that we were mistaken at least once for cousins. Both Oliver and our other friend Douglas went on to become successful general practitioners specialising in family medicine, while I took a longer path to become a hospital consultant in neurology. In a way I found the clinical course rather dull and I emerged from it worldly wiser but less analytical.
Oliver, myself, and Douglas became almost inseparable and studied together throughout the entire four-and-a-half year medical course. One of our particular habits was to have lunch virtually every day in the general refectory at the nearby Birkbeck College, where we mingled with older students, and, surprisingly, nobody ever asked us what we were doing there. They probably would now. Maybe some of them were also visitors like us. We liked the fact that these other students were studying non-medical subjects such as physics and chemistry as it made us feel more like ‘real’ university students, not ‘medics’. (In the UK, of course, this denotes a doctor and not a paramedic as it does in the US.) We both still have very fond memories of that friendly institution.
Douglas was more than a dozen years older than Oliver and me and so he had a great deal more life experience; he acted rather like a benign and wise older brother to us. He was also married with several children and, together with his good judgement and rather avuncular nature, added a valuable stabilising and balancing influence to our comparative immaturity and inexperience. The three of us spent many hours at lunch dissecting the merits and deficiencies of our various lecturers, and trying to work out exactly what they were trying so hard to teach us. This happy camaraderie proves the merit of UCL’s innovative policy of admitting students from widely differing social backgrounds and with quite large age variations. There were many ‘mature’ students of around 25–30 years, who to us teenagers seemed as old as Methuselah. Our year also included an older student from South Africa. While we got on well with him, he had a certain air of mystery and, while friendly, very much kept himself to himself, perhaps from a perceived fear of racial prejudice from some unexpected quarter.
The word ‘dissection’ immediately conjures up very specific memories, especially those of an olfactory nature, as many of us were never quite able to get used to the characteristic foul reek of dead bodies and formaldehyde emanating from the dissecting room where part of our anatomy studies were carried out (although it was nothing compared to the gut-wrenching smell of the post-mortem room which, as with many people, I found, and continue to find, almost intolerable). Real bodies were dissected at that time and it was obvious at the outset that a few students were deeply upset by the contact with dead people. For some reason I used to get particularly nauseated at the sight of thick layers of fat overlying the muscles. Why this was so I have no idea. We took some comfort from the knowledge that our own subject for dissection had reached the ripe old age of 100 years – we felt that he had had a good innings so to speak. I took care not to think of him as he might have been during life. To do this somehow seemed ghoulish and invited distress.
Usually six students worked on each of the approximately 20 cadavers. My group was reasonably assiduous in turning up for dissection sessions, and we would be tested orally on our knowledge of specific regions every few weeks by the anatomy demonstrators. Anatomy demonstrators were either senior academics, or more frequently, younger tutors who were either aspiring surgeons studying for their qualifying ‘fellowship’ examinations or doctoral students who had taken the pre-clinical course and were engaged in research rather than clinical medicine. A few of the doctoral students would eventually take the clinical course themselves; they were a very mixed bunch of people, some benign, some severe, some brilliant, and some disinterested – and some blended a few or all of these qualities. As a group we both respected and feared them.
Some of the demonstrators were far too kind and generous for our own good, having a very low threshold for giving ‘A’ grades during these tests. (The most generous and also stimulating of these tutors is now one of the world’s most distinguished neuroscientists whom I still see from time to time when I visit London.) On the other hand, a few of them were pretty mean with their grades and would reward really competent performances with ‘B minus’ or even ‘C’ grades. That really used to upset us. Somewhere in the middle was Dr M, a young general surgeon from Ceylon (as it was called at that time before it became Sri Lanka in 1972) in his late twenties. He was rather tall, somewhat stern and extremely fair in his mark allocation, and had an amusing dislike of people ‘inventing names’ of body parts. For example, he would get really irritated if students mixed up the names of major arteries and veins and then mistakenly identify some non-existent blood vessel with a hybrid name. ‘Don’t invent names!’ he would shout at the offender. He was a no-nonsense individual whom I liked immediately, and I think this feeling was mutual. It was he who three years later was to give Oliver and I the chance of a lifetime to experience life and work in Africa. If it were not for Dr M then I wouldn’t be writing this book.
Undergraduate life at UCL was pretty hard work but very stimulating. A number of the lecturers and staff were world-renowned scientists including Sir Andrew Huxley (whom we all found to be a profoundly modest man) and the late Sir Bernard Katz, both Nobel prize-winning physiologists. The teachers also included the remarkable Professor J.Z. Young who had been head of the anatomy department for many years. We students, like others, referred to this great man affectionately as ‘JZ’ and he had the unusual ability to communicate the excitement of science and medicine to his audience while ensuring that they were also competent in their basic knowledge. He had the ability to make everything he said clear, interesting and accessible. In a masterly and at times truly riveting series of lectures, he instructed us in a wide range of anatomical and general biological subjects, including the somewhat esoteric topic of the origin of life.
We also had the pleasure of meeting Dr Alex Comfort, the erudite scientist and expert on ageing who later won worldwide fame for his book The Joy of Sex. I remember most his seriousness in conversation, his obvious popularity with his students in the zoology department and his telling me, as if repeating a mantra, that ‘it is much easier to postpone a rate than to rewrite a programme’ when devising methods to overcome the process of ageing.
Another scientist who made a very strong impression was the late and greatly missed Professor Patrick Wall, the eminent expert on pain whose theories have been very influential in the clinical management of chronic pain, in particular through the development of a treatment called transcutaneous electrical nerve stimulation (commonly abbreviated to TENS) which was based on the ‘gate’ theory of pain. He once expressed to us during an anatomy lecture the remarkable notion that a doctor treating a patient with a bullet wound has a duty to understand why that bullet came to be fired in the first place. Following on from this he thought that the doctor should pursue this line of enquiry and find out exactly how the patient came to be shot. Some of us thought that this introduced an inappropriate political dimension to patient management but it certainly made us think hard about the issue. He also used to roll his own cigarettes and I used to be mesmerised during his lectures by the deft way he would do this using a compact little oblong container that looked to me like one of my father’s oriental antiques. He would calmly lick the sticky end of the paper at some point during his lecture and seemingly out of nowhere a thin cigarette would emerge. I met him on many subsequent occasions, and it was he who first steered me towards my future PhD supervisor, the eminent Martin Raff in the zoology department at UCL several years later, so I owe him a debt of gratitude for his good judgement and sound career advice. He also demonstrated well how it is possible to be both a brilliant and innovative scientist and also a profoundly decent and kind human being. I miss him a lot.
From time to time we would have a foretaste of the lecturing styles and personalities of the clinically active university staff of UCH, the teaching hospital right beside us. Exposure to these ‘real doctors’ could be inspiring, amusing and daunting at the same time, and students were usually impressed by the calm and authoritative demeanour of these suave medical doctors. And they all wore smart suits. A senior neurosurgeon who exuded gravitas managed to terrify many of us with his ‘in your face’ brain operation slides with bloody tissues and swabs everywhere, and an unsuspecting physician failed to notice the silver fairy wand that a mischievous student had secretly stuck on to the tip of his wooden pointer. The unfortunate man completely misinterpreted the audience’s laughter as a reaction to his own sparkling wit as he leaped around the lecture podium.
I particularly remember the stern warning given to us all by Professor Charles Dent, an extremely eminent expert in metabolic medicine and one of only a few clinicians to be elected a fellow of the Royal Society (the direct equivalent of the US National Academy of Sciences). He transfixed us with his penetrating gaze and told us that there were two rules that we were always to observe during our medical careers. The first was to have clean fingernails and hands, and the second was to never get emotionally involved with a patient under our care, a crime punishable by possibly being struck off the medical register. Thinking about it now this was actually pretty sound advice, especially at that early impressionable stage. The next time you are in the presence of a group of medical doctors I suggest you try the following experiment. Try counting how many of them have clean fingernails. I guarantee that most, if not all, will! Through an odd twist of fate Professor Dent had a lasting influence on our later African experience.
Each department at UCL also seemed to have its own distinctive physical environment. For example, the anatomy department had a distinctive ‘academic’ smell, not at all unpleasant, and its floors and walls, and each small laboratory or office, seemed wrapped in an individual mystique that we hoped we would experience one day. Many of us deeply envied the cool PhD students who worked in those romantic corridors. The Cerebral Functions Research Group, headed by Patrick Wall, glowed as the epitome of scientific achievement. The physiology department, full of current and future scientific stars, had a more spacious architectural style compared with the intimate dwellings of anatomy, while the biochemistry department was a vast series of modern laboratories with wooden brown sliding doors and rows of laboratory glassware and chemicals, and housed ultra bright people, not all of whom seemed to enjoy teaching medical students. The well-stocked library was nearby and for many months I was unable to identify a rhythmic hooting noise that seemed to emanate from there. Eventually I realised that it was merely the cries of the local pigeons which were clearly of an academic bent.
Oliver, Douglas and I passed the second MB examinations without much trouble and skipped the opportunity of spending another 18 months’ studying for an additional Bachelor of Science degree. I came to later regret that decision. We shared an overwhelming desire to get onto the wards and become ‘real’ doctors, and therefore started the three year clinical course at UCH in April 1971.
UCH was profoundly different from UCL, because it involved seeing live patients. Our contact with the hospital, which had an interesting physical structure resembling a Maltese cross, had been virtually non-existent during the previous 18 months. Apart from exposure to the few visiting lecturers, it had been limited to a brief obligatory visit to the operating theatre – where the green-gowned surgeon uttered a kind of low growl as a form of greeting on being alerted to our presence – and also the radiology department which appeared less forbidding despite X-ray machines that would not have been out of place in the recent War of the Worlds movie. Now that we were at the hospital to study sick people and healing, it was necessary to rapidly alter one’s whole perception of life and to adopt a more mature attitude. In these initial few months we had our first contact with the processes of dying, both quick and slow, and we were impressed by the extent to which some people are so incredibly unlucky with their health. How unwittingly fortunate the rest of us were!
During the introductory week many of us were inspired by the encouraging words of the UCH Professor of Medicine, Lord Rosenheim, who sadly died shortly afterwards. He assured us that many chronic untreatable diseases that we were currently seeing would be cured in our lifetimes, and that some of us would almost certainly play a role in making that happen. We kind of believed him, and in fact he was partly right. Perhaps the most inspirational teacher we met during that week, and indeed in the entire course, was the neurologist Gerald Stern, who remains to this day a good friend and mentor. Immediately after his three hour session with us on neurological disorders I had made my mind up to be a neurologist, and never wavered from this course such was the strength of the impression that he made.
UCH had an outstanding reputation in both clinical medicine and scientific achievement. A number of physicians working at UCH at that time possessed exceptional clinical acumen and judgement. Some of the younger of these went on to occupy major Chairs and other high positions in London and elsewhere in the United Kingdom as well as North America, and the clinical skills of many of the physicians and surgeons at UCH were legendary.
During the first year we were divided into small groups of about six students, and rotated on medical and surgical ‘firms’ which were clinical units consisting of two or more consultants both at UCH and the affiliated Whittington Hospital in Archway, London. Our small London group was a friendly and motley crew that, in typical UCL style, was drawn from many different walks of life and age ranges.