10,49 €
Mehr erfahren.
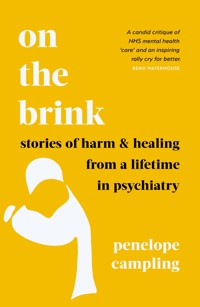
- Herausgeber: Elliott & Thompson
- Kategorie: Sachliteratur, Reportagen, Biografien
- Sprache: Englisch
We have lost our way when it comes to treating serious mental illness: this is a powerful call to arms from highly respected doctor and therapist, Penelope Campling. 'Deeply thoughtful and compassionate' Susie Orbach, author of In Therapy 'As a GP I wish I could send patients to Penelope Campling; as someone worried about failing mental health services, I wish she were in charge.' Gavin Francis, author of Adventures in Human Being NHS psychiatrist and psychotherapist Dr Penelope Campling has spent a lifetime on the frontline of mental health care, working with patients in crisis. Now she has an urgent message for us all: with our health service at breaking point, we are failing people in serious mental distress. We can and must do better. Dr Campling invites us into her therapy room. At the forefront of a radically new approach to working with mental illness, she shows how therapeutic communities have helped her patients to break generational cycles of trauma, change crippling internal narratives of shame and despair, overcome abuse and rebuild their lives to find meaning and hope. Moving and insightful, On the Brink combines patients' stories with candid self-reflections on the difficult business of helping others. 'A book with the power to move and inform . . . [Campling] is an expert in "intelligent kindness".' Gwen Adshead, author of The Devil You Know '[An] insightful, important book . . . an exhibition of what could be possible and an invitation to act to deliver that vision.' Kathryn Mannix, author of Listen 'This book oozes compassion and kindness and made me want to be a more understanding doctor.' Kate Milton, British Journal of GP Practice Previously published in hardback under the title Don't Turn Away: Stories of Troubled Minds in Fractured Times
Das E-Book können Sie in Legimi-Apps oder einer beliebigen App lesen, die das folgende Format unterstützen:
Seitenzahl: 435
Veröffentlichungsjahr: 2022
Ähnliche
‘A book which has the power to move and inform those who read it; and also to inspire curiosity and maybe even a bit of anger at what has happened to mental health services in the last 20 years . . . In this wise and compassionate work, Dr Penny Campling draws on decades of expertise to ask challenging questions about our mental health services and how we can make them better. She is an expert in ‘intelligent kindness’ and it shows.’
Gwen Adshead, author of The Devil You Know
‘A candid critique of current NHS mental health “care” and an inspiring rally cry for better. Politicians should read it.’
Benji Waterhouse, author of You Don’t Have to Be Mad to Work Here
‘“We do better together than on our own” is the rallying cry of this insightful, important book. Using case stories and a long view, Dr Penelope Campling shows us how chronic under-valuing of our mental health services has eroded their resources . . . This book is a crie de coeur from a wise elder of the art of psychotherapy. Unless and until we recognise every person’s right to mental and emotional wellness, with access to timely expert help that supports them on their journey to wholeness or to self-acceptance with a sense of agency, we are participants in a societal failure to act. This book is an exhibition of what could be possible and an invitation to act to deliver that vision.
Kathryn Mannix, author of With the End in Mind
‘Deeply thoughtful and compassionate: here is psychiatry at its very best as Penelope Camping shows us how she feels into the dilemmas of her patients as they search for ways to live more peaceably with themselves.’
Susie Orbach, author of In Therapy
‘As a GP I wish I could send patients to Penelope Campling; as someone worried about failing mental health services, I wish she were in charge.’
Gavin Francis, author of Adventures in Human Being
An important book spanning [Campling’s] decades-long career in mental health services. She provides a moving and honest account of her clinical experiences and insights alongside a full and accurate history of public mental healthcare practices in the UK.’
Dr Beth Guilding, TLS
‘This book oozes compassion and kindness and made me want to be a more understanding doctor. Penelope Campling worked for the NHS for 40 years as a Psychiatrist and Psychotherapist and her book uses touching patient stories to explain her points and so there is a lot of engaging humanity as well as learning points . . . extremely powerful. Despite diagnosing myself and the whole NHS with Moral Injury, this book was uplifting!’
Kate Milton, British Journal of GP Practice
‘A lucid and much-needed articulation of the frustration shared by so many struggling to keep the NHS afloat.’
Iona Heath, BMJ
‘A compassionate, polemical and often angry read.’
The Tablet
‘There are moving chapters here based on her time on in-patient wards, in therapeutic communities, forensic settings, young people’s units, and even within the brightly lit and noisy interiors of intensive therapy units as the COVID-19 pandemic rages. Best of all is the segment towards the end where Dr Campling sees her therapy patients, who have suffered from COVID-related isolations, under a makeshift awning in her back garden. Both the patients and Dr Campling are freezing cold but value the warmth of human contact. In this way she prioritises the quality of our relationships with each other over the shifting sands of our institutional settings . . . [A] fine book and is accessible for the seasoned psychiatrist and general reader alike.’
Alan Baban, British Journal of Psychiatry
‘A superb account of [Campling’s] life on the psychiatric frontline . . . Campling writes sympathetically on cases seen over her career, skilfully describing the complexities of dealing with damaged patients, the dilemmas of assessing risk and determining why some people enduring mental pain end up harming themselves. Some stories are bizarre, some depressing, but all are fascinating.’
Ian Birrell, Unherd.com
This book is dedicated to those struggling with severe mental health problems who find themselves unable to access the support they need and deserve; and to those mental health workers who continue to give their all in very difficult circumstances.
And in memory of Dr Steve Pearce, who died too young after a long illness, one of the kindest and the best.
AUTHOR’S NOTE
This book and the stories within it are based on my clinical experience. Some people have generously agreed to appear in these pages, but the book covers many years and it has not been possible to trace everyone. I have therefore anonymised them completely and changed details of incidents, trying to remain true to their essence, but mindful of the need to protect confidentiality and privacy.
The stories in this book touch on some difficult and distressing topics. If you are affected by any of the themes covered in these pages, you can call Samaritans on 08457 909090 or visit the Samaritans website to find details of the nearest branch.
Many mental health trusts now operate a central access line for acute problems. You can find the number by visiting your local trust’s website.
CONTENTS
Introduction
1 Out of Sight, Out of Mind
2 The Cabinet of Curiosities
3 Terrible Secrets
4 Experts by Experience
5 Locked In
6 Who’s in Charge?
7 Hope and Despair
8 Facing Up to Suicide
9 Give Sorrow Words
10 Hidden Histories
11 A Global Trauma
12 Moral Injury
13 A System of Exclusion
Epilogue
Acknowledgements
Notes
Further Reading and Resources
About the Author
INTRODUCTION
This book is about my experience working with people whose mental suffering has taken them right to the edge of human experience – many of them facing it with great courage.
It is also a reflection on our relationship as a society with mental illness,* about the precarious state of our mental healthcare services, about the fragility of progress and how easy it is for things to go into reverse.
Most importantly, it is about the potential for change, about how things can be turned around if we can only engage wisely and nurture the creative opportunities that are there even at the darkest and most chaotic of times.
I started my career as a psychiatrist nearly forty years ago at the Towers, one of two Victorian asylums in Leicester. It was a profoundly flawed institution where I encountered patients who had been locked away and forgotten for years – institutionalised, infantilised, their individuality eroded. And yet I began that first job full of optimism. We all knew that change was under way: plans to close the Towers were already in place, and the generation before us had taken huge steps towards humane care, reforming the Mental Health Act and breaking down the barriers between the asylums and the community. We believed in progress. It was an era filled with hope.
Just six months later, I moved on to a brand new mental health unit attached to the General Hospital. It was a hugely significant change, one that reflected the reforms taking place throughout the country, indeed throughout most of the richer countries in the world. The building itself seemed to embody a new and hopeful chapter in the history of psychiatry. At the time it felt as if I was part of a great leap forward, playing a small part on the right side of history, my future career glittering in my imagination with grateful patients, exciting discoveries, and a palpable sense of progress.
And indeed some things did improve. We now understand a lot more about the human mind and have a growing evidence base informing us how best to help people who are struggling. There has also been a sea change in attitudes to mental health more generally. People are more open about their feelings, and mental health problems are no longer the taboo they were a generation or two ago. Celebrities – even royalty – talk publicly about their battles with mental illness. Mental well-being and mindfulness have become part of everyday language and therapy is increasingly seen – in some sections of society, at least – as a normal, healthy thing to do. Public health campaigns reassure us that there is no shame in sharing feelings of despair and thoughts of suicide and remind us that mental health problems will affect as many as one in four of us at some point in our lives.
But despite all of this, mental health services have not thrived in recent years. Morale is desperately low on the front line. People with serious mental illness are likely to die on average fifteen to twenty-five years earlier than those without SMI, largely from preventable diseases such as heart disease and diabetes.1 Report after report has confirmed what every mental health worker knows: that the service is in a terrible state and that the shocking chasm between what is needed and what we are actually resourced to provide is getting larger, leaving an increasing number of vulnerable people and their families in dark and desperate states of mind. The theme tunes seem horribly familiar as the potential for depriving, brutalising and dehumanising mental health patients re-emerges in different settings. To my great sadness, we seem to be moving backwards: the progress made during my early career steadily eroding.
Now we have services where desperate patients wait for months to see a psychiatrist or therapist; where the bed shortage is such that we end up sending severely ill adolescents hundreds of miles away from their families; where traumatised refugees are housed in detention centres that are more like prisons than care facilities. Why, at a time when we seem so much more comfortable talking openly about mental health and have so much more knowledge than previous generations, do we put up with sparse, inadequate and sometimes even abusive services? There seems to be some sort of paradox here: a shadow as dark and gothic as those lunatic asylums of old.
Funding is, of course, a huge issue. Health ministers talk recurrently about ‘transforming’ services and promise more money, but action doesn’t seem to follow the rhetoric. Despite all the positive talk, the gap between what we spend on mental health care and the level of need in our society has been growing steadily since the 1950s. The proportion of healthcare money spent on mental health has also declined. Since 2013, the NHS constitution in England has included a commitment ‘to improve, prevent, diagnose and treat both physical and mental health problems with equal regard’. But despite strategies and legislation,* we continue to miss this by a long shot.
Much of the first edition of this book was written during the Covid-19 pandemic. Like most people I often felt frightened. The world seemed a dangerous place. As a psychiatrist, I know that a crisis can go both ways and always contains the seeds of opportunity. But early glimpses of values and priorities shifting and the hope of ‘building back better’ were not sustained after the pandemic. Far from binding us together, our country – the whole world, in fact – emerged more unequal and divided than ever; and individuals more fearful, more vulnerable, more unstable.
Covid-19 exacerbated an already perilous situation. It is now clear to most people that the NHS itself is on the brink, in desperate need of proper attention, long-term planning and economic investment. Is there a special case for mental health services? Clearly some of the problems are being felt in other specialties across the NHS, but there are issues of scale and important differences not acknowledged or understood properly that I hope to clarify in this book.
Just how much mental health services had lost their way was brought home to me in the first few weeks of the pandemic. The edict from NHS England was to discharge as many inpatients as possible. Clearly the risk of infection was real, but the mental health charity MIND has published research suggesting that in some cases this was done with no review of ongoing mental health needs and worrying outcomes for the patients.2 Our local mental health trust, among others, discharged the majority of its outpatients at the beginning of March 2020, giving them instead a central crisis line number to ring in an emergency. Cutting off ongoing support at a very frightening time to those already identified as mentally vulnerable seemed utterly brutal to me. It showed no understanding that encouraging people to use support to pre-empt crises is a fundamental premise of mental health work, and that abruptly terminating an ongoing therapeutic relationship is likely to be disturbing and dangerous.
There has been a lot of talk in recent years about ‘parity of esteem’, treating mental health on a par with physical health, but these decisions seem to show just how low down the ranking order mental health services themselves see their patients. Compounding everything else, the pandemic presented the country with a mental health crisis. But extraordinarily, rather than stepping up, it seems that mental health services (with honourable exceptions) were stepped down.
Such a stark example of a whole organisation turning away from the mentally vulnerable patients it was responsible for, at the worst possible time, focused my thoughts on the uncertain progress of psychiatry over the last forty years.
How has it happened that we value our patients and our attempts to help them so little? How has it happened that our services are increasingly designed to deny people care instead of helping them to access it? We seem to have drifted into a culture, in many ways as harsh and neglectful as I encountered in the institutions of old.
Perhaps the truth is that severe mental illness is just as frightening, just as stigmatising, just as much a taboo as it always has been. Our relationship as a society with mental disorder is not straightforward. How we think about the mentally ill, how we relate to them, how we manage the feelings they evoke, whether we see them as deserving of serious investment, even where we house them – none of these questions seems to get easier, however much progress we make in other areas. We do not want to face the reality of the suffering of those with more serious mental health problems, nor to fund their care adequately – or perhaps we simply don’t know how. It is easier to tranquillise, restrain, separate, lock them up or ignore them than it is to engage properly with their needs and their pain.
The reality is that being up close with mental disturbance is difficult and discomforting. There will always be a degree of ambivalence. Connecting with others in severe mental distress can jolt us into facing our own vulnerability and hook into fears of dependency and losing our own sanity – fears that are often deeply buried. And the fact is that mental well-being is not something any of us can take for granted. Adverse life events can push most of us over a threshold where vicious circles – a complex mix of social, psychological and biological factors, all interacting and amplifying each other – start to take hold.
In the twenty-first century, mental health problems are not about the ‘other’, but about you and me, our families and friends. Most of us know families struggling with a parent with severe dementia, a child with autism or an eating disorder, a teenager with obsessive compulsive disorder or severe drug problems, a young person who has just been diagnosed with bipolar disorder or schizophrenia, a mother with post-natal depression. These conditions and many others are commonplace but can have a devastating impact on the individual and their family, and lead to a significant cost for society at large.
I want this book to reach patients, clinicians, politicians, and ‘ordinary people’ living in a society where mental health problems are escalating; to bridge the distance between us and those in severe mental distress. Keep in mind that mental health services are expected to take over where family love, friendship and community support can no longer manage a person’s disturbance, where patience has worn out and understanding has turned to bewilderment – or even worse, terror, anger or rejection. We professionals are invited in – or sometimes are duty-bound to intervene – when people are losing their grip on reality, when their brains are playing maddening tricks or when extreme emotion threatens to overwhelm them. We are privileged by society to see and to try to help people at their most desperate, frightened and exposed.
Bridging the world of psychiatry (the branch of medicine interested in ailments of the mind) and psychotherapy (the interpersonal process of healing the mind) through the last four decades, I am in a position to take you up close: to share my experience with patients and show you what is involved in genuinely struggling to connect with the psychological suffering of others. At its best this can be a surprisingly rewarding experience. But the seeds for such relationships to go wrong are always present. There’s a constant danger of finding oneself invaded by hopelessness and helplessness. There’s always the risk of falling into an us-and-them-type relationship – into an ‘othering’ dynamic. It’s only too easy for care and protectiveness to turn into control or even abuse.
I’ve tried to be honest about the way these dynamics can creep in and to help the reader understand how they can further complicate the relationship we have with mental ill-health as individuals and as a society. As we shall see, they can arise in all sorts of situations, good and bad, though they are much more likely to take root at times – like the present – when staff are overstretched, undervalued and feel forgotten.
We desperately need to find a way to rebuild faltering services. There are no easy answers here, no simple mantras. I don’t want to guilt-trip anyone or suggest the problems would go away if we were all a bit nicer. But I do invite you to care about these people, to take them and the often-awful experiences that have befallen them seriously. Sadly, such experiences are often the result of all-too-common inhumanities and shortcomings in our society. Facing up to these things is difficult but such understanding is vital if we are to build enough momentum to move things forward. The more open we are to thinking about mental ill-health in all its complicated, disturbing reality, the more in touch with ourselves we shall be. And the more in touch with ourselves we are, the better able we are to promote safe relationships, build strong and healthy communities, support mental well-being, and effectively lobby for better mental health care.
We need to think radically. The scale of the problem has always been too big to be left to specialist mental health staff alone. Encounters with mental distress – in a loved one, a neighbour, a stranger, a patient, or in society as a whole – can feel too difficult to bear, too weird and frightening, or just too bloody misery-inducing. But we have a choice and if we do turn away from people in distress and abandon our mental health services to their steady decline, there are serious costs for us all.
__________
* I use the term ‘mental illness’ as synonymous with severe mental health problems. It is not intended to imply causation.
* The ‘No Health Without Mental Health’ strategy in 2011 was enshrined in law in the 2012 Health and Social Care Act.
1
OUT OF SIGHT, OUT OF MIND
I have vivid memories of my first weekend on call as a junior psychiatrist. It was the long August bank holiday weekend, 1983. I was twenty-five and the only doctor around in a neo-Gothic building, the size of a small village: the Towers Hospital, one of two Victorian asylums serving the population of Leicestershire. Set on a hill in extensive, well-landscaped grounds, this outwardly grand building had been built over a hundred years earlier to stand imposing and isolated. Having six hundred beds, it was small in comparison to many such institutions, but still seemed gulpingly big to me.
It is hard to convey just how cold the corridors were: I soon learned to take my coat with me, even though it was high summer. The blue-tiled floors and high ceilings amplified any noise; the strip-lighting paled people’s faces; the heavy church-like doors on to the wards were almost always locked. The worst passage was outside the kitchens where it was hard to avoid the sound of cockroaches crunching under my feet. A handful of patients frequented this corridor, seemingly preferring it to sitting around on the wards. One man, Eric, would spend all day, every day, walking up and down with his hands behind his back, jutting his head up and down rather like a pigeon, completely oblivious of my presence. Every few minutes, he would start to wail, a chilling eerie sound that I found harrowing, particularly when I was there on my own. ‘Sweet Pete’ was a more welcome feature of that corridor, dressed in a smart suit jacket, tie and trilby hat, carrying a brolly in one hand and a briefcase in the other. Pete would pace intently from one end of that corridor to the other, over and over, as if he were late for a business meeting – rumour had it he had once been a bank manager. There was nothing frightening about Pete, who would doff his hat as he passed, offer a cheery greeting and then mutter that he was late and hurry off. He was presumably preserving an islet of dignity in his otherwise damaged mind. Sadly, his legs – decked out in pyjama bottoms – gave the game away.
Most Victorian mental asylums were built a few miles outside their home city, close enough to serve the population but not so close as to encroach on citizens’ consciousness, the fear of madness that they might engender kept a safe distance away. During my childhood in the 1960s, such institutions were referred to as ‘loony bins’. I can still remember the hushed and fearful tone of voice that my parents used whenever we drove past the gates of our local asylum. A decade or two later, a series of media investigations laid bare the brutal way some of these institutions were treating their vulnerable inhabitants.
Although it avoided national attention, the Towers was no exception when it came to maltreatment. Scandal was rife, but whispered rather than publicised. It’s difficult to get any perspective on the history we embody, especially when we’re young. As a medical student, I had read books by the famous sociologist Erving Goffman about asylums, outlining the theoretical dangers of large institutions that were closed off to the outside world, but at this early stage in my career, I hadn’t really applied these ideas to myself and my colleagues.1 Nothing had prepared me for the casual brutality and nihilism I was to encounter on some of those wards, the wretched condition of some of the inhabitants for whom this squalid institution was their only home.
A brand new unit on the General Hospital site was due to open in six months’ time, but that would only be for people with acute problems. Others would continue in the Towers for many years and it is the treatment of these patients that this chapter focuses on. Some of them, I was beginning to discover, had lived there for over half a century, everyday decisions being made for them, their lives organised by others and predictable in every detail, any sense of autonomy a far-distant memory, their individuality crushed by years of being treated the same as everyone else.
On Saturday morning, I was called by a nurse from one of the wards that housed these patients who were seen as chronic. We called these ‘back wards’ – derogatory enough – but ‘forgotten wards’ would have been more accurate. These were people who were not expected to get better and had spent many years in the hospital, too mad and too vulnerable – or, as we were beginning to understand, too institutionalised – to cope outside the asylum. Would I pop over and have a look at Sylvia? She had started refusing drinks, which was unlike her, and the nurse was worried she would become dehydrated.
It took me twenty minutes to locate the ward, which was up a winding staircase in one of the towers that gave the building its name. I was intrigued at what I would find as I’d already discovered that each ward had its own culture, largely determined by the personality of the lead nurse. As with many asylums, it was usual for staff to be recruited from the local neighbourhood, with closely knit nursing teams and stories going back well before the war when someone’s grandad had been the ward manager and someone else’s aunt had been a nursing assistant.
The nurses on Sylvia’s ward seemed kind, and she had been allowed to put her best dress on for my visit, a dress she had brought with her when she’d been admitted thirty years earlier. It was a cotton summer frock patterned with yellow roses, the full skirt gathered at her waist with a golden satin sash and a heart-shaped neckline. It looked very like a party dress I’d had when I was a little girl, but I knew the style had been popular with adults in the fifties. Sylvia was sitting in a standard hospital armchair covered in tatty red plastic, but draped with a beautiful cream lace shawl, similar to the one she was wearing over her shoulders. She was perched on the edge of the chair, sitting with an impressively straight back, tatting with an antique ivory pointed shuttle. Tatting is a type of lace-making that, luckily for this encounter, I’d happened to learn as a child at my grandmother’s knee, so I was able to make informed and appreciative comments about the neatness of her ‘cow hitch knots’ and ‘picots’ that quickly established a rapport.
Sylvia bent her head towards me confidentially, speaking in not much more than a whisper.
‘I’m so sorry, doctor, I would have liked to wear my best jewellery but due to a number of unfortunate experiences, I don’t trust the hoi polloi in this vicinity of the city. They have their hands in everything’ – eyebrows archly raised as she swept her gaze around the room, before nodding at me complicitly.
I asked her where she’d come from. She was silent for a few seconds, then said, ‘Bath is a beautiful city. Have you ever visited the pump rooms?’ She then poured, as if from a teapot, and lifted her hand to her mouth as if she was sipping a cup of tea – little finger properly crooked, of course. It seemed we were in some genteel pretend game. I played along – rather self-consciously I have to admit, worried that I was being watched and would seem ridiculous, not at all sure what was expected of me.
Sylvia was the first patient I’d met from a chronic ward. How were we expected to behave with these institutionalised people? There seemed to be no expectation that we explore their long-term problems, find out what first brought them into hospital, or indeed do anything to change the status quo. While I was sipping my pretend tea, I tried to move the conversation on to the reason for my visit, why she was not drinking more. She simply smiled sweetly and asked if the tea was to my liking.
Later, I chatted to the nurses, wondering aloud if she might be frightened of wetting herself. I was right. She had been incontinent recently and that had preceded her refusing to drink. I could imagine that wetting herself had been horribly humiliating for someone like Sylvia, so desperately trying to hang on to her dignity, against all the odds. I ordered a urine test, preferring not to wonder how the nurses would get a sample from someone so fastidious. Sure enough, a urinary tract infection was eventually diagnosed and I started Sylvia on antibiotics. But how to get Sylvia drinking properly again? Rather to the surprise of the nurse on duty, I brought in a little teapot with old-fashioned bone-china teacups and saucers that I’d noticed in the resident doctor’s room and, to Sylvia’s delight, we sat down to another tea party – this time with proper tea.
Sylvia had been admitted as an involuntary patient in 1949, in an era when once you were admitted to an asylum, there was little expectation of getting out again, indeed little sense of the potential to recover from a mental illness. Compared with the amount we are expected to document these days, there was very little written in her file. The last entry was nearly four years old and described a rash she’d developed on her hands. Her admission note was particularly sparse. A one-sentence letter from a GP: ‘Please admit this post-partum young lady who has been acting in a crazy manner since she gave birth 3 weeks ago.’ And a few more lines from the admitting psychiatrist: ‘22-year-old lactating woman . . . gave birth to a healthy boy weighing 6lbs 2ozs at 5 o’clock on 15th June 1950 . . . has developed a condition of deep melancholia . . . prescribed ECT.’ There was no background history or any information about what had happened to the baby. For that I had to read through a handful of letters included in the file.
It seemed that Sylvia had fallen in love and married an exsoldier, who had recently returned from Thailand where he had been a prisoner at the end of the war. It transpired that this young man – presumably very damaged from the experience – already had a wife and two children in Scotland. Sylvia discovered that she had married a bigamist who, once this truth emerged, quickly moved back to Scotland, leaving Sylvia to face the shock, the shame and the pregnancy alone. No surprise that with this social and psychological disruption in the background, the rapid changes in hormones in the first weeks after giving birth had tipped her into some sort of mental breakdown. How severe was not clear from the notes, but there was nothing to suggest the start of what we would think of today as a serious mental illness: ‘agitated weeping’ and ‘attempts to escape the hospital’ were the main symptoms documented. I could only imagine Sylvia’s rage and despair.
Her medical notes, typical of their time, were written in an almost illegible scrawl. It is true we were probably better at deciphering other people’s handwriting in those days but, nevertheless, there was little sense in the psychiatric documents of this era that doctors were expecting anyone else to read them or felt the need to account for their decisions. This was to change with the 1959 Mental Health Act which was designed to abolish the difference between psychiatric hospitals and other types of hospital, and make it easier for treatment to be voluntary and informal. Compulsory treatment became dependent on a formal medical decision and legal framework that held psychiatrists to account for detaining someone against their will. This was progress indeed, and the start of a decline in the numbers shut away in asylums. But it had had little effect on Sylvia, who, like so many patients of her generation, had become dependent on the hospital for her basic needs: her food, her warmth and shelter, her medical care and her clothing – a victim of the ‘total institution’.
In October 1983, two months after I’d started in psychiatry, another Mental Health Act was passed, which tightened up the law around ‘sectioning’, making it harder to detain, assess and treat someone against their wishes. This meant no one could be brought into hospital against their will without the formal assessment of a legally approved and specially trained social worker, as well as two doctors and the signed consent of a close relative. It also offered more clarity about the nature of disorder where detention was deemed appropriate – the concept of ‘treatable condition’ was important – and held professionals to account through a system of appeals and tribunals. (The term ‘section’ refers to the particular Section of the Act involved.) Looking back, the timing of the new Act was fortuitous for me. It meant I spent two training days, right at the start of my career, immersed in mental health law and history, and engaged in a prolonged lively debate alongside psychiatrists, social workers and solicitors with decades of experience and widely differing views. There were some cynical voices, as you’d expect with any major change, but most people saw it as progress and spoke enthusiastically about the changes it would bring. When I look back on this time, I’m struck by the optimism around, our belief in ourselves and the strong sense of being part of a movement forward. To some degree, this mitigated the everyday grimness.
I have always been fascinated by the question of what it is to be human and psychiatry seemed a very obvious specialty to choose, but I was discovering that madness can lay you bare in very desperate ways and the urge to turn away was immense. The back wards at the Towers were full of people like Sylvia with their heart-breaking stories locked away inside themselves, scantily sketched in medical notes that nobody seemed to read, and lost even to the nursing teams who cared for them. The core symptoms of mental illness were often worryingly absent when people were admitted and, tragically, illegitimate pregnancies and homosexuality not uncommonly the main reason given.
Others had bizarre neurological symptoms, poorly understood at the time, that made them extremely difficult to nurse. I remember one man with a severe and interesting version of Capgras syndrome. He was convinced not only that the nurses were impostors but that the ward itself was a fake. His dementia was such that his psychotic beliefs were incoherent and often changing, but at times he was convinced we were the ‘Bosch’ and he was being held in a Colditz-like castle. At the time, we tried to understand this psychoanalytically, while the nurses tried to talk him out of it: ‘Stop being silly, Ernie. You know perfectly well I’m no Kraut!’ We know now that Capgras syndrome is common in the type of Alzheimer’s disease where there is damage to the right parietal lobe – the area of the brain that is responsible for spatial and facial recognition. I’m not sure if knowing this would have helped the nurses manage Ernie’s frightened state. He was quite obviously terrified of us and very afraid to walk through a door or even to cross the room.
I’d like to tell you that I spent hours with these long-stay patients, getting to know them, but this would be indulging in wishful thinking. In truth, I neglected them like everyone else. I was a bit frightened of them, although I wouldn’t have admitted this at the time. Perhaps disturbed is the better word. There was certainly a dark side to their madness, with occasional scenes of gothic lunacy – ripping clothes off, screaming obscenities, lashing out, biting and scratching at anyone who got in their way – that could have sat comfortably in the pages of a Brontë novel. They were not all like Sylvia, clinging so determinedly to her modicum of bourgeois gentility – dear Sylvia, who a few months later gave me a beautiful handmade lace shawl. Today we rarely see such extreme outward expressions of madness because patients are medicated with modern drugs from an early stage. Many in the ‘critical psychiatry’ movement would argue that they are just being put in chemical straitjackets, the underlying psychotic beliefs not much changed.2
I had loved my psychiatry placement as a medical student, fired up by the academic learning, the applied philosophy and the more prolonged contact with patients, but we’d been kept well away from the asylum and sheltered by particularly humane enthusiastic consultants. My experience at the Towers could not have been more different. The consultant I now worked for seemed to find my presence an irritant, shaking his head anxiously whenever I spoke, raising his eyebrows quizzically whenever I dared give an opinion. He had a few patients with whom he worked psychoanalytically. It was months into the job before I discovered that I was supposed to steer clear of these ‘special’ patients. It was as if by talking with them I’d been found doing something inappropriate and intrusive. Again and again, I found myself tripping over unwritten rules that made no sense. Everyone but me seemed to be ‘in the know’, but the culture somehow made it difficult to ask questions. I realise now that this sense of alienation, of being outside the group, is a classic scenario in institutions. At the time I just lost my bearings a bit.
I was spending a lot of time doing things I hated: prescribing ever higher levels of horrible drugs, doing depot (long-acting injection) clinics and administering electroconvulsive therapy (ECT). No one seemed to value the fact that I talked with patients. In fact, I was often expected to write up medicines without even seeing the person. Sometimes I was asked to ‘counsel’ a particular individual, which sounded more promising, but it turned out this meant I was supposed to ‘give them a good ticking off’ – the threat of increasing their medication implied – because they’d refused to eat their dinner, or pinched their friend’s doll, or tried to bite one of the nurses.
On one occasion, though, reading through someone’s notes going back over fifty years, I was surprised to come across a very different type of psychiatrist. It was his beautiful looped handwriting that first grabbed my attention, but then I was drawn in by the narrative. His description of his conversations with this particular patient, Hester May, read like a detective story: a working-class girl made pregnant by her upper-class ‘sweetheart’, she had refused to submit to the pressures put on her to disappear quietly and have the child adopted, which had eventually led to her being categorised as a ‘moral imbecile’ and incarcerated. (The category of ‘moral imbecile’ was eventually abolished in the 1959 Mental Health Act.)
A classic story but no less painful for that. The psychiatrist seemed fascinated by the patient’s story, enraged by it, unable to let it go, and I had a growing sense of encountering someone a bit like me. But his notes, which started in 1942, lasted only two years, then abruptly stopped. I felt I’d made a friend, then lost him. Who was this humane psychiatrist, kicking against the system back in the 1940s? Why wasn’t he part of the ‘war effort’? What had happened to him? After that, if I was seeing elderly long-stay patients, I always turned to 1942 to see if he had been involved. I was mostly disappointed. There were a handful of scripts by him in other patients’ notes, but short and to the point.
When I was asked to see this lady who had so fascinated him, more than forty years later, Hester May was very elderly, struggling with heart failure, and adamant that her symptoms had been caused by Ethel, another patient on the ward, casting a spell on her. She was particularly upset by her swollen legs: ‘Fred used to tell me I had beautiful ankles,’ she’d say, just as if it was yesterday rather than forty-five years ago. ‘I always knew she was jealous and would find a way to spoil them.’ Fred, I assumed, was the ‘sweetheart’ of her story. When I tried to explain to Hester about her heart failure and why I’d prescribed her diuretics, she’d cackled with painful laughter: ‘Don’t you go telling me about me old ’eart, me duck.’ Then, gasping to get her breath, ‘There’s nothing you can tell Hester May about a broken ’eart.’
I had become a psychiatrist because I was interested in people’s stories. I wanted to understand what made them tick. I wanted to find ways to connect with them. At the time my pretend tea party with Sylvia made me feel confused and ridiculous. In retrospect, however, my attempt to get alongside her reflects what my career has been about: a search to engage therapeutically, a quest to build and sustain empathy in a very non-empathetic world. I like to think my doctor with the beautiful handwriting would have understood that.
My friend, Marie, has had an impressive career, working for the Red Cross in some of the most dangerous, impoverished parts of the world. But she is quite clear that one of her worst experiences was her first placement as a student mental health nurse on an elderly ward at the Towers, where she was unlucky enough to encounter an outbreak of salmonella infection. The ward was put in quarantine, so what was meant to be a nine-hour shift turned out to be seventy-two hours: three days and three nights imprisoned on the ward nursing severely demented patients through a serious bout of gastroenteritis. She still has nightmares about the sheer force of the explosive diarrhoea and projectile vomiting happening around her and the utter wretchedness of those already frail old women. She had never seen anyone die before, but by the end of the three days she’d laid out four bodies.
Body waste and continence is an issue on all hospital wards, particularly elderly wards, but the stench of those at the Towers in the early 1980s was much worse than anything I’ve had to deal with before or since. It was hard to get away from excrement on these wards. It wasn’t just the smell: it seemed to always be there, defining our relationship with the patient, leaving little room for any other part of their story. Millie, for example, was known as ‘Mrs Teapot’ because she used to mould her faeces into tiny little beads, hide them away and then, when no one was looking, post them down the spout of the teapot. Needless to say we were repulsed, but no one thought to try to understand or help her communicate the feelings lurking beneath this behaviour.
I experimented with visiting the wards at different times of day, but it made no difference. There simply seemed to be an acceptance that elderly people who were losing their minds could sit around in their own shit. It was this nihilism, I think, that made it so different from medical wards where the smell of pathological waste products and decaying flesh can be equally or more abhorrent but attracts scientific interest or heroic action from the staff around. Here the sight and smell of faeces seemed to express the hopelessness and horror of bodies outliving their minds, the despair of people judged as beyond dignity or respect.
As a doctor, I was spared the worst of it. I tried not to judge the nurses who were stuck on one ward for their whole shift and were earning less than I was, despite their many years of experience. I remember once walking past one of the student nurses and noticing she was looking rather grim. I asked if she was all right and she thrust a bowl towards me with a load of nail clippings. ‘Smell them!’ she said, holding it up near my face. The smell was so disgusting and so unexpected that I gagged. Apparently, cutting the patients’ faecesencrusted nails was one of the jobs the students hated most. Some of the nurses were brilliant, of course, as repelled by the environment and some of the more inhumane rituals as I was. One or two were already involved in the design of a new unit, still years away, which they would go on to lead. But there’s no way to sugar-coat it: some of what I witnessed was vile.
I remember arriving on a male ward to find a queue of old men, standing in their greying underpants, waiting to be shaved. On another occasion, on the female ward, I came across two nurses systematically going around washing the women, one carrying a bowl of grimy-looking water, the other the flannel and hairbrush: ‘Come on, me love, open your legs for me, let’s get the dirty parts done.’ And then on to the next woman: same bowl of grimy water; same filthy flannel; same hairbrush.
The bathroom had two baths in the middle of the room and on the shelf above the basins was a row of twenty-four sets of false teeth in unmarked jars. One poor woman used to masturbate so violently in the bath that the nurses had to hold her down. Like most people faced with such encounters, I felt embarrassment, disgust and perhaps a bit of fascination. Mostly, we just pretended it wasn’t happening. It is easiest to deal with this uncomfortable mix of feelings with shocked disapproval or mirth. But the masturbation I was forced to encounter at the Towers wasn’t predatory in any way, and ‘lust’ doesn’t really capture it. It was more comfort-seeking than attention-seeking and when I look back at it from the safe distance of middle age, my heart goes out to those patients who had found perhaps the only way of being in touch with themselves.
I was also shocked to discover that there were still a handful of patients with neuro-syphilis or GPI (general paralysis of the insane) slowly dying in the Towers. Syphilis is a bacterial sexually transmitted disease that attacks the brain tissue in its tertiary stage, causing severe psychosis and dementia. It can be treated in its early stages with penicillin, so had become less common. Despite doing an infectious diseases job as a house officer, the nearest I’d come to the tragedy of this infection before doing time at the Towers was in the pages of Karen Blixen’s novel Out of Africa and watching a production of Henrik Ibsen’s play Ghosts.
Of all dehumanising diseases, tertiary syphilis must be one of the worst. Oozing sores become foul-smelling ulcers and abscesses that can spread across the face into bone and other organs. One of the men in the Towers had a disfigured chin with raw open flesh where his bottom lip should have been; another had half his nose missing. It was hard not to flinch with repulsion as well as pity and I had no difficulty understanding why victims of the disease had been shunned and isolated, the repellent necrotic symptoms read by previous generations as a sign of sin. Even in the first half of the twentieth century, prior to the establishment of the NHS, health insurance schemes did not cover self-inflicted conditions, so treatment for venereal disease was often withheld.
Penicillin had been available since 1943, but somehow these stragglers still around in the Towers in the early eighties had gone undiagnosed and untreated for years while the necrotic damage progressed. In the past, they would have died within a few months. Now we had the means to stop the disease progressing, but they literally had holes where brain tissue should be and there was little we could do to help. There was often severe frontal-lobe damage, which meant they were particularly disinhibited and difficult to nurse. I remember one man forever stripping off his clothes, underwear and all, and singing a crude version of a sea shanty – the first two lines over and over again.
Most distressing was the pain. I was called on a couple of occasions to see one man who seemed particularly tortured. His ravaged face and throat and brain disease made words impossible. But he tossed in agony and keened, a sound between a frightened squeal and a howl, more like an injured fox or a cat, the scream of an animal in the throes of death, which was desperately distressing for everyone around him. Bone pain is particularly difficult to bear and hard to alleviate. He was already on a large dose of morphine and a too high dose of tranquillisers, which I didn’t dare increase. All I could do was make impotent soothing noises drowned out by his agony and sit for a while with the nurses before returning to my bed. It was hard to get back to sleep.
I don’t want to give the impression that everything about the Towers was bad. Once off the long corridor and on the other side of the big heavy doors into the wards, I found little empires of their own, the regimes varying widely. The acute wards had a much stronger link with consultant psychiatrists and some of them were humane, progressive and pushing hard for reform. Nevertheless, much of the Towers exhibited the worst characteristics associated with what Erving Goffman described as a ‘total institution’, with most of the inhabitants – including many of the nurses, whose home was the nurses’ residence – living and sleeping in the place, and institutional needs taking precedence over patient care. A particular problem for such institutions was their tendency to become inward-looking and to not question their own practices. I found it extraordinary that tea was served in huge metal pots, the milk and sugar already mixed in. And surely anybody could see that giving patients their final meal of the day at 4.30 p.m. followed by a mug of Ovaltine and bed at 7 p.m. was treating them as if they were children? But although these were issues I could moan about with other junior psychiatrists, none of us thought to challenge the powers that be. It was a hierarchical culture that was all-embracing, that could twist one’s moral values and actions. Cut off from outside scrutiny, the staff had enormous power over the patients and there was always the potential for such power to be used abusively. The loss of liberty and social isolation from family and community left the patients pretty well at the mercy of however the staff chose to behave.
It’s easy to work for a short time in a total institution and produce a satirical analysis of those whose lives were so narrowly defined. Easy for the junior doctor, always the visitor, always moving on after six months, always the outsider. So different for the nurses, leaving their late shifts at 9.15 p.m., back in for their ‘earlies’ at 7 a.m., long hours cooped up on one ward, day in day out, year after year, their lives entangled with their teammates and their disturbing patients. And as for the long-stay patients – wearing cheap, ill-fitting clothes bought by the nurses in a batch at a knock-down price in a sale; sleeping in dormitories with the next bed a hand-hold away; washing themselves in bathrooms and defecating in toilets with unlockable doors; eating bland, monotonous food served at times to suit the institution – they were a textbook example of the way total institutions are prone to putting people’s needs second to those of the institution, demeaning and degrading them in the process.
But I was affected as much as anyone in my own way. It wasn’t the grown-up temper tantrums, desperate though they were, that upset me most: at least in those cases there was still a person there, feeling something tangible. It was more the number of people who had totally retreated into their heads, completely mute, their personhood eroded and locked away, meaningful human connection long since deemed hopeless. Some of the patients had holes in their forehead, a sign that they’d been subjected to brain surgery – a frontal-lobe lobotomy. One man had lost his speech completely during the operation, his attempts to communicate reduced to barking.
At times I felt I was coming up against raw need that had overwhelmed any sense of dignity and broken through any conventionally civil inter-human boundary. I can still remember my first experience of this, working in Mumbai as a medical student; the staring hungry eyes of people begging, the aggression, the injuries and disabilities that we were told, rightly or wrongly, were sometimes self-inflicted to arouse our pity – as if our pity needed further amplifying. Pity is such a disturbing feeling anyway: the vast gap between oneself and the other somehow dehumanising; the impotent compassion too painful.
It felt a little bit like this walking onto some of the wards at the Towers, with a chorus of ‘Gimme a smoke!’ emanating from half a dozen or so voices, their sense of desperation condensed down to the task of procuring a free fag. Not aggressive exactly but certainly persistent: bodies sidling up to me, grabbing my hand, pawing at my hair, dropping ash on my clothes.